J Korean Soc Radiol.
2011 Aug;65(2):191-198. 10.3348/jksr.2011.65.2.191.
Multi-Detector CT Findings of the Normal Appendix in Children: Evaluation of the Position, Diameter, and Presence or Absence of Intraluminal Gas
- Affiliations
-
- 1Department of Radiology, College of Medicine, Chungnam National University, Daejeon, Korea. jckim@cnu.ac.kr
- KMID: 1443484
- DOI: http://doi.org/10.3348/jksr.2011.65.2.191
Abstract
- PURPOSE
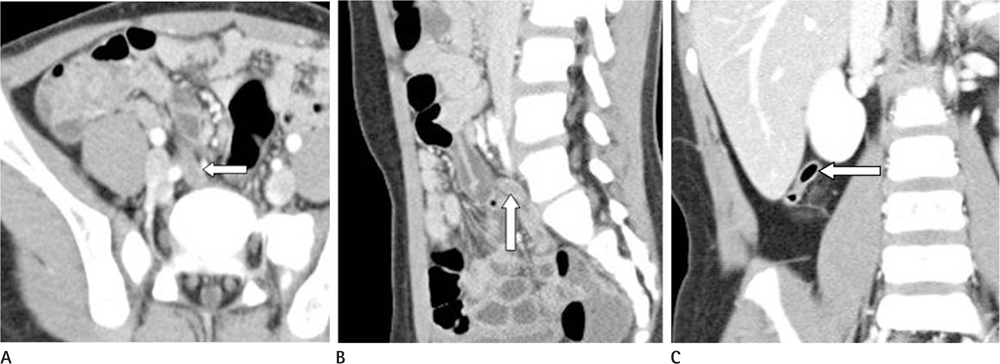
To assess the usefulness of multi-detector CT (MDCT) with multiplanar reformations (MPR) for the evaluation of the position, diameter and presence or absence of intraluminal gas in the normal appendix in children.
MATERIALS AND METHODS
From 2007 to 2010, we retrospectively analyzed the MDCT images of normal appendices in 133 children, and evaluated the position, diameter, and presence or absence of intraluminal gas in the appendix.
RESULTS
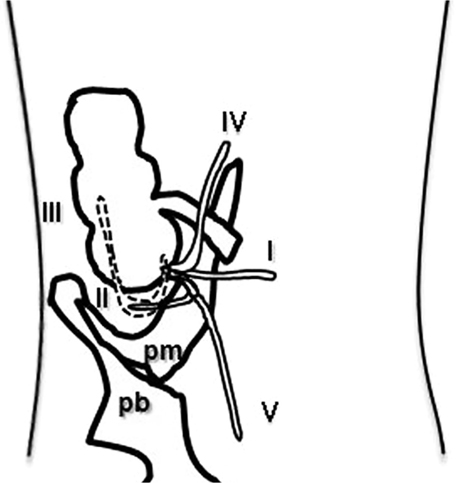
Among the 133 appendices, type I (postileal and medial paracecal position) was found in 64 children, type II (subcecal position) in 22, type III (retrocecal and retrocolic/laterocolic position) in 15, type IV (preileal and medial colic position) in 16, and type V (lower pelvic position) in 16 children. The mean diameter was 5.8 mm +/- 1.2 (SD) (range; 3.2-8.7 mm). There was a high correlation between the appendiceal diameter and age (p = 0.000).There was no statistically significant difference in the appendiceal diameter between boys and girls (p = 0.470). Intraluminal gas was found in 115 appendices and there was no statistically significant correlation between the appendiceal diameter and intraluminal gas (p = 0.502).
CONCLUSION
The MDCT with MPR was useful for the evaluation of the normal appendices in children. The procedure may be useful for the diagnosis of equivocal or unusual appendicitis in children.
Figure
Reference
-
1. Karakas SP, Guelfguat M, Leonidas JC, Springer S, Singh SP. Acute appendicitis in children: comparison of clinical diagnosis with ultrasound and CT imaging. Pediatr Radiol. 2000; 30:94–98.2. Mullins ME, Kircher MF, Ryan DP, Doody D, Mullins TC, Rhea JT, et al. Evaluation of suspected appendicitis in children using limited helical CT and colonic contrast material. AJR Am J Roentgenol. 2001; 176:37–41.3. Brender JD, Marcuse EK, Koepsell TD, Hatch EI. Childhood appendicitis: factors associated with perforation. Pediatrics. 1985; 76:301–306.4. Savrin RA, Clatworthy HW Jr. Appendiceal rupture: a continuing diagnostic problem. Pediatrics. 1979; 63:36–43.5. Lewis FR, Holcroft JW, Boey J, Dunphy E. Appendicitis. A critical review of diagnosis and treatment in 1,000 cases. Arch Surg. 1975; 110:677–668.6. Lee HS, Kim YT, Kim HC, Bae WK, Kim IY. CT Findings of Acute Appendicitis in Children. J Korean Radiol Soc. 2005; 52:271–277.7. Rao PM, Rhea JT, Novelline RA, McCabe CJ, Lawrason JN, Berger DL, et al. Helical CT technique for the diagnosis of appendicitis: prospective evaluation of a focused appendix CT examination. Radiology. 1997; 202:139–144.8. Rao PM, Rhea JT, Novelline RA, Mostafavi AA, Lawrason JN, McCabe CJ. Helical CT combined with contrast material administered only through the colon for imaging of suspected appendicitis. AJR Am J Roentgenol. 1997; 169:1275–1280.9. Rettenbacher T, Hollerweger A, Macheiner P, Gritzmann N. [Ultrasonography of the normal vermiform appendix]. Ultraschall Med. 1997; 18:139–142.10. Oh KJ, Cho JS, Shin KS, Kim HY, Lim SK, Ohm JY, et al. Normal Appendix in Adults: MDCT Findings about the Location, Thickness and the Presence or Absence of Intraluminal Gas. J Korean Radiol Soc. 2006; 55:373–379.11. Rettenbacher T, Hollerweger A, Macheiner P, Rettenbacher L, Frass R, Schneider B, et al. Presence or absence of gas in the appendix: additional criteria to rule out or confirm acute appendicitis--evaluation with US. Radiology. 2000; 214:183–187.12. Neville AM, Paulson EK. MDCT of acute appendicitis: value of coronal reformations. Abdom Imaging. 2009; 34:42–48.13. Keyzer C, Pargov S, Tack D, Créteur V, Bohy P, De Maertelaer V, et al. Normal appendix in adults: reproducibility of detection with unenhanced and contrast-enhanced MDCT. AJR Am J Roentgenol. 2008; 191:507–514.14. Benjaminov O, Atri M, Hamilton P, Rappaport D. Frequency of visualization and thickness of normal appendix at nonenhanced helical CT. Radiology. 2002; 225:400–406.15. Ghiatas AA, Chopra S, Chintapalli KN, Esola CC, Daskalogiannaki M, Dodd GD 3rd, et al. Computed tomography of the normal appendix and acute appendicitis. Eur Radiol. 1997; 7:1043–1047.16. Wiersma F, Srámek A, Holscher HC. US features of the normal appendix and surrounding area in children. Radiology. 2005; 235:1018–1022.17. Applegate KE, Sivit CJ, Myers MT, Pschesang B. Using helical CT to diagnosis acute appendicitis in children: spectrum of findings. AJR Am J Roentgenol. 2001; 176:501–505.18. Ozturkmen Akay H, Akpinar E, Akgul Ozmen C, Ergun O, Haliloglu M. Visualization of the normal appendix in children by non-contrast MDCT. Acta Chir Belg. 2007; 107:531–534.19. Puylaert JB. Acute appendicitis: US evaluation using graded compression. Radiology. 1986; 158:355–360.20. Garcia K, Hernanz-Schulman M, Bennett DL, Morrow SE, Yu C, Kan JH. Suspected appendicitis in children: diagnostic importance of normal abdominopelvic CT findings with nonvisualized appendix. Radiology. 2009; 250:531–537.21. Jan YT, Yang FS, Huang JK. Visualization rate and pattern of normal appendix on multidetector computed tomography by using multiplanar reformation display. J Comput Assist Tomogr. 2005; 29:446–451.22. Birnbaum BA, Wilson SR. Appendicitis at the millennium. Radiology. 2000; 215:337–348.23. Baldisserotto M, Marchiori E. Accuracy of noncompressive sonography of children with appendicitis according to the potential positions of the appendix. AJR Am J Roentgenol. 2000; 175:1387–1392.24. Schumpelick V, Dreuw B, Ophoff K, Prescher A. Appendix and cecum. Embryology, anatomy, and surgical applications. Surg Clin North Am. 2000; 80:295–231.25. Rao PM, Rhea JT, Rattner DW, Venus LG, Novelline RA. Introduction of appendiceal CT: impact on negative appendectomy and appendiceal perforation rates. Ann Surg. 1999; 229:344–349.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Normal Appendix in Adults: MDCT Findings about the Location, Thickness and the Presence or Absence of Intraluminal Gas
- The Value of Sonographic Evaluation of the Appendix in Patient with Pelvic Inflammatory Disease: Correlation with CT, clinical, and Pathological Findings
- CT Features of Appendiceal Mucocele
- Multi-Detector CT Findings of Palpable Chest Wall Masses in Children: A Pictorial Essay
- Usefulness of Multiplanar Reformatted Images of Multi-detector Row Helical CT in Assessment of Biliary Stent Patency