J Korean Assoc Oral Maxillofac Surg.
2012 Feb;38(1):50-54. 10.5125/jkaoms.2012.38.1.50.
Surgical management of edentulous/atrophic mandibular fracture: a report of two cases
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, College of Dentistry, Yonsei University, Seoul, Korea. kimoms@yuhs.ac
- 2Research Center for Orofacial Hard Tissue Regeneration, College of Dentistry, Yonsei University, Seoul, Korea.
- KMID: 1434379
- DOI: http://doi.org/10.5125/jkaoms.2012.38.1.50
Abstract
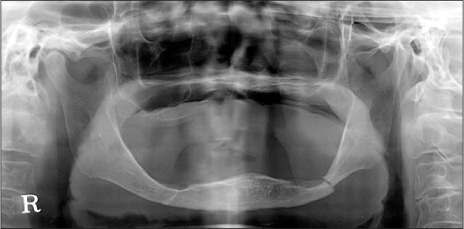
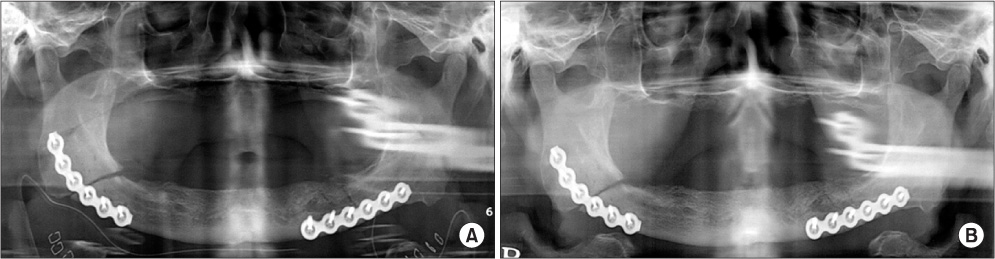
- According to Luhr's classification, a fracture in the mandible with a width of less than 15-20 mm is considered to be an atrophic mandibular fracture and its incidence is very rare. Because of the reduced cross-sectional area and smaller contact area of the fractured ends as well as the poorly vascularized bony structure and delayed bone healing, an atrophic mandibular fracture is a great challenge for oral and maxillofacial surgeons. Surgeons tend to perform closed reduction, because open reduction is considered a non-life-saving surgery among elderly patients. Thus, most of them have limited experience in surgical management. According to recent reports, open reduction yields a good result, and the Association for Osteosynthesis (AO) group has recommended open reduction. This is a case report of our two experiences of open reduction and rigid fixation of atrophic mandibular fractures by the AO principle. Articles were also reviewed here.
Figure
Reference
-
1. Luhr HG, Reidick T, Merten HA. Results of treatment of fractures of the atrophic edentulous mandible by compression plating: a retrospective evaluation of 84 consecutive cases. J Oral Maxillofac Surg. 1996. 54:250–254.
Article2. Reich KM, Huber CD, Lippnig WR, Ulm C, Watzek G, Tangl S. Atrophy of the residual alveolar ridge following tooth loss in an historical population. Oral Dis. 2011. 17:33–44.
Article3. Yang SB, Moon HS, Han DH, Lee HY, Chung MK. Oral health status and treatment need of institutionalized elderly patients. J Korean Acad Prosthodont. 2008. 46:455–469.
Article4. Mugino H, Takagi S, Oya R, Nakamura S, Ikemura K. Miniplate osteosynthesis of fractures of the edentulous mandible. Clin Oral Investig. 2005. 9:266–270.
Article5. Ellis E 3rd, Price C. Treatment protocol for fractures of the atrophic mandible. J Oral Maxillofac Surg. 2008. 66:421–435.
Article6. Zide MF, Ducic Y. Fibula microvascular free tissue reconstruction of the severely comminuted atrophic mandible fracture-- case report. J Craniomaxillofac Surg. 2003. 31:296–298.
Article7. Prein J. Arbeitsgemeinschaft für O. Manual of internal fixation in the cranio-facial skeleton: techniques recommended by the AO/ASIF-Maxillofacial Group. 1998. New York: Springer.8. Madsen MJ, Haug RH, Christensen BS, Aldridge E. Management of atrophic mandible fractures. Oral Maxillofac Surg Clin North Am. 2009. 21:175–183.
Article9. Pargger H, Scheidegger D. Surgical risk and anesthesia in geriatric patients. Orthopade. 1994. 23:16–20.10. Bradley JC. Age changes in the vascular supply of the mandible. Br Dent J. 1972. 132:142–144.
Article11. Phillips JH, Rahn BA. Fixation effects on membranous and endochondral onlay bone-graft resorption. Plast Reconstr Surg. 1988. 82:872–877.
Article12. Lin KY, Bartlett SP, Yaremchuk MJ, Fallon M, Grossman RF, Whitaker LA. The effect of rigid fixation on the survival of onlay bone grafts: an experimental study. Plast Reconstr Surg. 1990. 86:449–456.13. Rücker M, Binger T, Deltcheva K, Menger MD. Reduction of midfacial periosteal perfusion failure by subperiosteal versus supraperiosteal dissection. J Oral Maxillofac Surg. 2005. 63:87–92.
Article14. Champy M, Loddé JP, Schmitt R, Jaeger JH, Muster D. Mandibular osteosynthesis by miniature screwed plates via a buccal approach. J Maxillofac Surg. 1978. 6:14–21.
Article15. Sikes JW Jr, Smith BR, Mukherjee DP, Coward KA. Comparison of fixation strengths of locking head and conventional screws, in fracture and reconstruction models. J Oral Maxillofac Surg. 1998. 56:468–473.
Article16. Schmelzeisen R, McIff T, Rahn B. Further development of titanium miniplate fixation for mandibular fractures. Experience gained and questions raised from a prospective clinical pilot study with 2.0 mm fixation plates. J Craniomaxillofac Surg. 1992. 20:251–256.
Article17. Sikes JW Jr, Smith BR, Mukherjee DP. An in vitro study of the effect of bony buttressing on fixation strength of a fractured atrophic edentulous mandible model. J Oral Maxillofac Surg. 2000. 58:56–61.
Article18. Kunz C, Hammer B, Prein J. Fractures of the edentulous atrophic mandible. Fracture management and complications. Mund Kiefer Gesichtschir. 2001. 5:227–232.19. Haug RH, Street CC, Goltz M. Does plate adaptation affect stability? A biomechanical comparison of locking and nonlocking plates. J Oral Maxillofac Surg. 2002. 60:1319–1326.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Surgical Management of Edentulous Atrophic Mandible Fractures in the Elderly
- The remodeling of the posterior edentulous mandible as illustrated by computed tomography
- Protraction of mandibular molars through a severely atrophic edentulous space in a case of juvenile periodontitis
- Functional impression technique using temporary denture for rehabilitation of severely atrophic maxillary and mandibular ridges
- Management of the Third Molar Tooth in Mandibular Angle Fracture