J Korean Assoc Oral Maxillofac Surg.
2012 Feb;38(1):44-49. 10.5125/jkaoms.2012.38.1.44.
Clinical, statistical and chemical study of sialolithiasis
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, Seoul National University Dental Hospital, Seoul, Korea. leejongh@snu.ac.kr
- KMID: 1434378
- DOI: http://doi.org/10.5125/jkaoms.2012.38.1.44
Abstract
- INTRODUCTION
Sialolithes are initiated by localized deposition of calcified material in the salivary glands. And that may even cause various symptom especially swelling and pain. This study purposes to collect statistical data of sialolithiasis for clinical analysis.
MATERIALS AND METHODS
Among forty seven patients who have visited Seoul National University Dental Hospital during 2004-2009, patients' age, sex, location and size of stone, radiodensity of stone, symptom, surgical procedure were investigated. Statistical correlation between size, location, symptom was evaluated. Chemical composition was analyzed for 3 sialolithes.
RESULTS
The average age was 41.4 years. Sialolithiasis had slight female predilection (57.4%). Most cases occurred in the submandibular glands (91.5%). And most cases had radiopaque features (95.8%). The average size was 7.17 mm. The most frequent location of the stones were the duct orifice and the submandibular gland hilum (16 cases in each), followed by the middle part of the duct (n=8), the intraglandular area (n=4), and the proximal part of the duct (n=3). Eleven cases were asymptomatic. Thirty six cases had complaints of pain, swelling, hardness, and decrease in saliva flow (multiple symptoms). Various methods of surgery was performed. Two cases were self-removed. Thirty seven cases underwent procedure involving stone removal alone. Six cases underwent gland extirpation, and two cases underwent ductoplasty.
CONCLUSION
There was no statistical correlation between size, location, and symptoms. Sialolith was composed of Ca (58.5-69.3%), P (30.7-35.7%), organic material, and trace inorganic material.
MeSH Terms
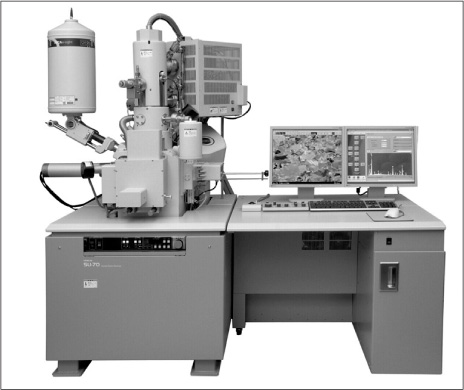
Figure
Cited by 2 articles
-
Incidental findings in a consecutive series of digital panoramic radiographs
David MacDonald, Warrick Yu
Imaging Sci Dent. 2020;50(1):53-64. doi: 10.5624/isd.2020.50.1.53.Elemental characteristics of sialoliths extracted from a patient with recurrent sialolithiasis
Buyanbileg Sodnom-Ish, Mi Young Eo, Kezia Rachellea Mustakim, Yun Ju Cho, Soung Min Kim
J Korean Assoc Oral Maxillofac Surg. 2024;50(2):94-102. doi: 10.5125/jkaoms.2024.50.2.94.
Reference
-
1. Escudier MP, McGurk M. Symptomatic sialoadenitis and sialolithiasis in the English population, an estimate of the cost of hospital treatment. Br Dent J. 1999. 186:463–466.
Article2. Gorlin RJ, Goldman HM. Thoma's oral pathology. 1970. 6th ed. St. Louis: C.V. Mosby.3. Haubrich J. Clinical aspects of non-tumorous diseases of the salivary glands. Arch Otorhinolaryngol. 1976. 213:1–59.4. Lustmann J, Regev E, Melamed Y. Sialolithiasis. A survey on 245 patients and a review of the literature. Int J Oral Maxillofac Surg. 1990. 19:135–138.5. Nahlieli O, Eliav E, Hasson O, Zagury A, Baruchin AM. Pediatric sialolithiasis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000. 90:709–712.
Article6. Ledesma-Montes C, Garcés-Ortíz M, Salcido-García JF, Hernández-Flores F, Hernández-Guerrero JC. Giant sialolith: case report and review of the literature. J Oral Maxillofac Surg. 2007. 65:128–130.
Article7. Bodner L. Giant salivary gland calculi: diagnostic imaging and surgical management. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002. 94:320–323.
Article8. Bodner L. Salivary gland calculi: diagnostic imaging and surgical management. Compendium. 1993. 14:572.9. Capaccio P, Bottero A, Pompilio M, Ottaviani F. Conservative transoral removal of hilar submandibular salivary calculi. Laryngoscope. 2005. 115:750–752.
Article10. Escudier MP. The current status and possible future for lithotripsy of salivary calculi. Atlas Oral Maxillofac Surg Clin North Am. 1998. 6:117–132.
Article11. Harrison JD, Triantafyllou A, Garrett JR. Ultrastructural localization of microliths in salivary glands of cat. J Oral Pathol Med. 1993. 22:358–362.
Article12. Marchal F, Kurt AM, Dulguerov P, Lehmann W. Retrograde theory in sialolithiasis formation. Arch Otolaryngol Head Neck Surg. 2001. 127:66–68.
Article13. Teymoortash A, Buck P, Jepsen H, Werner JA. Sialolith crystals localized intraglandularly and in the Whartons duct of the human submandibular gland: an X-ray diffraction analysis. Arch Oral Biol. 2003. 48:233–236.
Article14. Norman JED, McGurk M. Color atlas and text of the salivary glands diseases, disorders and surgery. 1995. London: Mosby-Wolfe.15. Kasaboğlu O, Er N, Tümer C, Akkocaoğlu M. Micromorphology of sialoliths in submandibular salivary gland: a scanning electron microscope and X-ray diffraction analysis. J Oral Maxillofac Surg. 2004. 62:1253–1258.
Article16. Yamamoto H, Sakae T, Takagi M, Otake S. Scanning electron microscopic and X-ray microdiffractometeric studies on sialolithcrystals in human submandibular glands. Acta Pathol Jpn. 1984. 34:47–53.
Article17. Anneroth G, Eneroth CM, Isacsson G. Crystalline structure of salivary calculi. A microradiographic and microdiffractometric study. J Oral Pathol. 1975. 4:266–272.
Article18. Koutsoukos PG, Nancollas GH. Crystal growth of calcium phosphates-epitaxial considerations. J Cryst Growth. 1981. 53:10–19.19. Schratter M, Steiner E, Imhof H. Conventional roentgen diagnosis of the salivary glands. Still of clinical value or "traditional care"-. Radiologe. 1994. 34:248–253.20. Avrahami E, Englender M, Chen E, Shabtay D, Katz R, Harell M. CT of submandibular gland sialolithiasis. Neuroradiology. 1996. 38:287–290.
Article21. Becker M, Marchal F, Becker CD, Dulguerov P, Georgakopoulos G, Lehmann W, et al. Sialolithiasis and salivary ductal stenosis: diagnostic accuracy of MR sialography with a three-dimensional extended-phase conjugate-symmetry rapid spin-echo sequence. Radiology. 2000. 217:347–358.
Article22. Wackym PA, Rice DH, Schaefer SD. Minimally invasive surgery of the head, neck and cranial base. 2002. Philadelphia: Lippincott Williams & Wilkins.23. Gundlach P, Hopf J, Linnarz M. Introduction of a new diagnostic procedure: salivary duct endoscopy (sialendoscopy) clinical evaluation of sialendoscopy, sialography, and X-ray imaging. Endosc Surg Allied Technol. 1994. 2:294–296.24. Hald J, Andreassen UK. Submandibular gland excision: shortand long-term complications. ORL J Otorhinolaryngol Relat Spec. 1994. 56:87–91.25. Beahrs OH. The facial nerve in parotid surgery. Surg Clin North Am. 1963. 43:973–977.
Article26. Dulguerov P, Marchal F, Lehmann W. Postparotidectomy facial nerve paralysis: possible etiologic factors and results with routine facial nerve monitoring. Laryngoscope. 1999. 109:754–762.
Article27. Ellies M, Laskawi R, Arglebe C, Schott A. Surgical management of nonneoplastic diseases of the submandibular gland. A follow-up study. Int J Oral Maxillofac Surg. 1996. 25:285–289.
Article28. Berini-Aytes L, Gay-Escoda C. Morbidity associated with removal of the submandibular gland. J Craniomaxillofac Surg. 1992. 20:216–219.
Article29. Bates D, O'Brien CJ, Tikaram K, Painter DM. Parotid and submandibular sialadenitis treated by salivary gland excision. Aust N Z J Surg. 1998. 68:120–124.
Article30. Moody AB, Avery CM, Taylor J, Langdon JD. A comparison of one hundred and fifty consecutive parotidectomies for tumours and inflammatory disease. Int J Oral Maxillofac Surg. 1999. 28:211–215.
Article31. Amin MA, Bailey BM, Patel SR. Clinical and radiological evidence to support superficial parotidectomy as the treatment of choice for chronic parotid sialadenitis: a retrospective study. Br J Oral Maxillofac Surg. 2001. 39:348–352.
Article32. Makdissi J, Escudier MP, Brown JE, Osailan S, Drage N, McGurk M. Glandular function after intraoral removal of salivary calculi from the hilum of the submandibular gland. Br J Oral Maxillofac Surg. 2004. 42:538–541.
Article33. Yoshimura Y, Morishita T, Sugihara T. Salivary gland function after sialolithiasis: scintigraphic examination of submandibular glands with 99mTc-pertechnetate. J Oral Maxillofac Surg. 1989. 47:704–710.
Article34. Marchal F, Kurt AM, Dulguerov P, Becker M, Oedman M, Lehmann W. Histopathology of submandibular glands removed for sialolithiasis. Ann Otol Rhinol Laryngol. 2001. 110:464–469.
Article35. Nahlieli O, Shacham R, Bar T, Eliav E. Endoscopic mechanical retrieval of sialoliths. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003. 95:396–402.
Article36. Nahlieli O, Nakar LH, Nazarian Y, Turner MD. Sialoendoscopy: A new approach to salivary gland obstructive pathology. J Am Dent Assoc. 2006. 137:1394–1400.37. Ziegler CM, Steveling H, Seubert M, Mühling J. Endoscopy: a minimally invasive procedure for diagnosis and treatment of diseases of the salivary glands. Six years of practical experience. Br J Oral Maxillofac Surg. 2004. 42:1–7.
Article