Korean J Radiol.
2013 Feb;14(1):70-80. 10.3348/kjr.2013.14.1.70.
Treatment of Hemodialysis Vascular Access Rupture Irresponsive to Prolonged Balloon Tamponade: Retrospective Evaluation of the Effectiveness of N-Butyl Cyanoacrylate Seal-Off Technique
- Affiliations
-
- 1Department of Radiology, Kaohsiung Veterans General Hospital, Kaohsiung 802, Taiwan.
- 2Department of Radiology, Yuan's General Hospital, Kaohsiung 802, Taiwan. jjychen@gmail.com
- 3National Yang-Ming University, School of Medicine, Taipei 112, Taiwan.
- KMID: 1430046
- DOI: http://doi.org/10.3348/kjr.2013.14.1.70
Abstract
OBJECTIVE
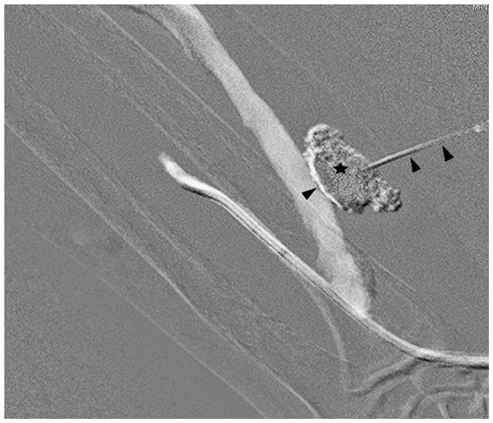
The current study retrospectively evaluated whether the percutaneous N-butyl cyanoacrylate (NBCA) seal-off technique is an effective treatment for controlling the angioplasty-related ruptures, which are irresponsive to prolonged balloon tamponade, during interventions for failed or failing hemodialysis vascular accesses.
MATERIALS AND METHODS
We reviewed 1588 interventions performed during a 2-year period for dysfunction and/or failed hemodialysis vascular access sites in 1569 patients. For the angioplasty-related ruptures, which could not be controlled with repeated prolonged balloon tamponade, the rupture sites were sealed off with an injection of a glue mixture (NBCA and lipiodol), via a needle/needle sheath to the rupture site, under a sonographic guidance. Technical success rate, complications and clinical success rate were reported. The post-seal-off primary and secondary functional patency rates were calculated by a survival analysis with the Kaplan-Meier method.
RESULTS
Twenty ruptures irresponsive to prolonged balloon tamponade occurred in 1588 interventions (1.3%). Two technical failures were noted; one was salvaged with a bailout stent-graft insertion and the other was lost after access embolization. Eighteen accesses (90.0%) were salvaged with the seal-off technique; of them, 16 ruptures were completely sealed off, and two lesions were controlled as acute pseudoaneurysms. Acute pseudoaneurysms were corrected with stentgraft insertion in one patient, and access ligation in the other. The most significant complication during the follow-up was delayed pseudoaneurysm, which occurred in 43.8% (7 of 16) of the completely sealed off accesses. Delayed pseudoaneurysms were treated with surgical revision (n = 2), access ligation (n = 2) and observation (n = 3). During the follow-up, despite the presence of pseudoaneurysms (acute = 1, delayed = 7), a high clinical success rate of 94.4% (17 of 18) was achieved, and they were utilized for hemodialysis at the mean of 411.0 days. The post-seal-off primary patency vs. secondary patency at 90, 180 and 360 days were 66.7 +/- 11.1% vs. 94.4 +/- 5.4%; 33.3 +/- 11.1% vs. 83.3 +/- 8.8%; and 13.3 +/- 8.5% vs. 63.3 +/- 12.1%, respectively.
CONCLUSION
Our results suggest that the NBCA seal-off technique is effective for immediate control of a venous rupture irresponsive to prolonged balloon tamponade, during interventions for hemodialysis accesses. Both high technical and clinical success rates can be achieved. However, the treatment is not durable, and about 40% of the completely sealed off accesses are associated with developed delayed pseudoaneurysms in a 2-month of follow-up. Further repair of the vascular tear site, with surgery or stent-graft insertion, is often necessary.
Keyword
MeSH Terms
-
Aged
Aneurysm, False/etiology/therapy
Angioplasty, Balloon/*adverse effects
Arteriovenous Shunt, Surgical/*adverse effects
Enbucrilate/*administration & dosage
Ethiodized Oil/administration & dosage
Female
Graft Occlusion, Vascular/etiology/*therapy
Humans
Male
*Renal Dialysis
Retrospective Studies
Rupture
Survival Analysis
Treatment Outcome
Ultrasonography, Interventional
Vascular Patency
Figure
Reference
-
1. Pappas JN, Vesely TM. Vascular rupture during angioplasty of hemodialysis raft-related stenoses. J Vasc Access. 2002. 3:120–126.2. Kim DH, Goo DE, Yang SB, Moon C, Choi DL. Endovascular management of immediate procedure-related complications of failed hemodialysis access recanalization. Korean J Radiol. 2005. 6:185–195.3. Funaki B, Szymski GX, Leef JA, Rosenblum JD, Burke R, Hackworth CA. Wallstent deployment to salvage dialysis graft thrombolysis complicated by venous rupture: early and intermediate results. AJR Am J Roentgenol. 1997. 169:1435–1437.4. Rundback JH, Leonardo RF, Poplausky MR, Rozenblit G. Venous rupture complicating hemodialysis access angioplasty: percutaneous treatment and outcomes in seven patients. AJR Am J Roentgenol. 1998. 171:1081–1084.5. Dale JD, Dolmatch BL, Duch JM, Winder R, Davidson IJ. Expanded polytetrafluoroethylene-covered stent treatment of angioplasty-related extravasation during hemodialysis access intervention: technical and 180-day patency. J Vasc Interv Radiol. 2010. 21:322–326.6. Vesely TM. Role of stents and stent grafts in management of hemodialysis access complications. Semin Vasc Surg. 2007. 20:175–183.7. Beathard GA. Management of complications of endovascular dialysis access procedures. Semin Dial. 2003. 16:309–313.8. Gray RJ, Sacks D, Martin LG, Trerotola SO. Society of Interventional Radiology Technology Assessment Committee. Reporting standards for percutaneous interventions in dialysis access. J Vasc Interv Radiol. 2003. 14(9 Pt 2):S433–S442.9. Sidawy AN, Gray R, Besarab A, Henry M, Ascher E, Silva M Jr, et al. Recommended standards for reports dealing with arteriovenous hemodialysis accesses. J Vasc Surg. 2002. 35:603–610.10. Weng MJ, Chen MC, Chi WC, Liu YC, Liang HL, Pan HB. Endovascular revascularization of chronically thrombosed arteriovenous fistulas and grafts for hemodialysis: a retrospective study in 15 patients with 18 access sites. Cardiovasc Intervent Radiol. 2011. 34:319–330.11. Sacks D, Marinelli DL, Martin LG, Spies JB. Society of Interventional Radiology Technology Assessment Committee. Reporting standards for clinical evaluation of new peripheral arterial revascularization devices. J Vasc Interv Radiol. 2003. 14(9 Pt 2):S395–S404.12. Kornfield ZN, Kwak A, Soulen MC, Patel AA, Kobrin SM, Cohen RM, et al. Incidence and management of percutaneous transluminal angioplasty-induced venous rupture in the "fistula first" era. J Vasc Interv Radiol. 2009. 20:744–751.13. Turmel-Rodrigues L, Pengloan J, Baudin S, Testou D, Abaza M, Dahdah G, et al. Treatment of stenosis and thrombosis in haemodialysis fistulas and grafts by interventional radiology. Nephrol Dial Transplant. 2000. 15:2029–2036.14. Turmel-Rodrigues L, Pengloan J, Rodrigue H, Brillet G, Lataste A, Pierre D, et al. Treatment of failed native arteriovenous fistulae for hemodialysis by interventional radiology. Kidney Int. 2000. 57:1124–1140.15. Turmel-Rodrigues L, Pengloan J, Bourquelot P. Interventional radiology in hemodialysis fistulae and grafts: a multidisciplinary approach. Cardiovasc Intervent Radiol. 2002. 25:3–16.16. Rajan DK, Clark TW, Simons ME, Kachura JR, Sniderman K. Procedural success and patency after percutaneous treatment of thrombosed autogenous arteriovenous dialysis fistulas. J Vasc Interv Radiol. 2002. 13:1211–1218.17. Liang HL, Pan HB, Chung HM, Ger LP, Fang HC, Wu TH, et al. Restoration of thrombosed Brescia-Cimino dialysis fistulas by using percutaneous transluminal angioplasty. Radiology. 2002. 223:339–344.18. Requejo F, Schumacher M, van Velthoven V. Coating the wall of an injured intracranial carotid artery during tumor removal with n-butyl-2-cyanoacrylate: technical case report. Neurosurgery. 2006. 59:4 Suppl 2. ONSE484–ONSE485. discussion ONSE485.19. Sheikh BY. Efficacy of acrylate tissue adhesive as vascular repair and hemostatic material. Ann Vasc Surg. 2007. 21:56–60.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prevalence and Management of Venous Rupture Following Percutaneous Transluminal Angioplasty in Dysfunctional Arteriovenous Access: A Comparative Study of Primary Patency Rates with Non-Ruptured Access Circuits
- Multiple Cerebral Infarction after Injection of N-Butyl-2-Cyanoacrylate for Gastric Variceal Bleeding
- Balloon Tamponade Treatment of a Stent-graft Related Rupture with a Splenic Artery Pseudoaneurysm: A Case Report
- Detection of an Infected N-butyl-2-cyanoacrylate Plug by F-18 FDG PET/CT Scan in a Patient Who Received Endoscopic Intervention for Gastric Variceal Bleeding
- Proximal Vein Obstruction or Stenosis Failed to Angioplasty in Hemodialysis Patients: Treatment with Endovascular Stent