Korean J Neurotrauma.
2012 Oct;8(2):104-109. 10.13004/kjnt.2012.8.2.104.
Efficacy of Short-Term versus Long-Term Post-Operative Antimicrobial Prophylaxis for Preventing Surgical Site Infection after Clean Neurosurgical Operations
- Affiliations
-
- 1Department of Neurosurgery, Hallym University College of Medicine, Seoul, Korea. osm@hallym.or.kr
- KMID: 1427720
- DOI: http://doi.org/10.13004/kjnt.2012.8.2.104
Abstract
OBJECTIVE
Surgical site infection (SSI) is a problem constantly uppermost in the minds of all surgeons, although the actual rate of occurrence is only 1-5% in general surgery. In neurosurgical fields, there have been a few papers published about efficacy of post-operative antimicrobial prophylaxis (PAMP) to prevent SSI, compared to well known effectiveness of pre-operative antibiotics. Thus, infection rates of short-term PAMP groups and those of long-term PAMP groups were investigated to evaluate the effectiveness of PAMP and the efficacy of short-term PAMP compared to long-term PAMP for prevention of SSI.
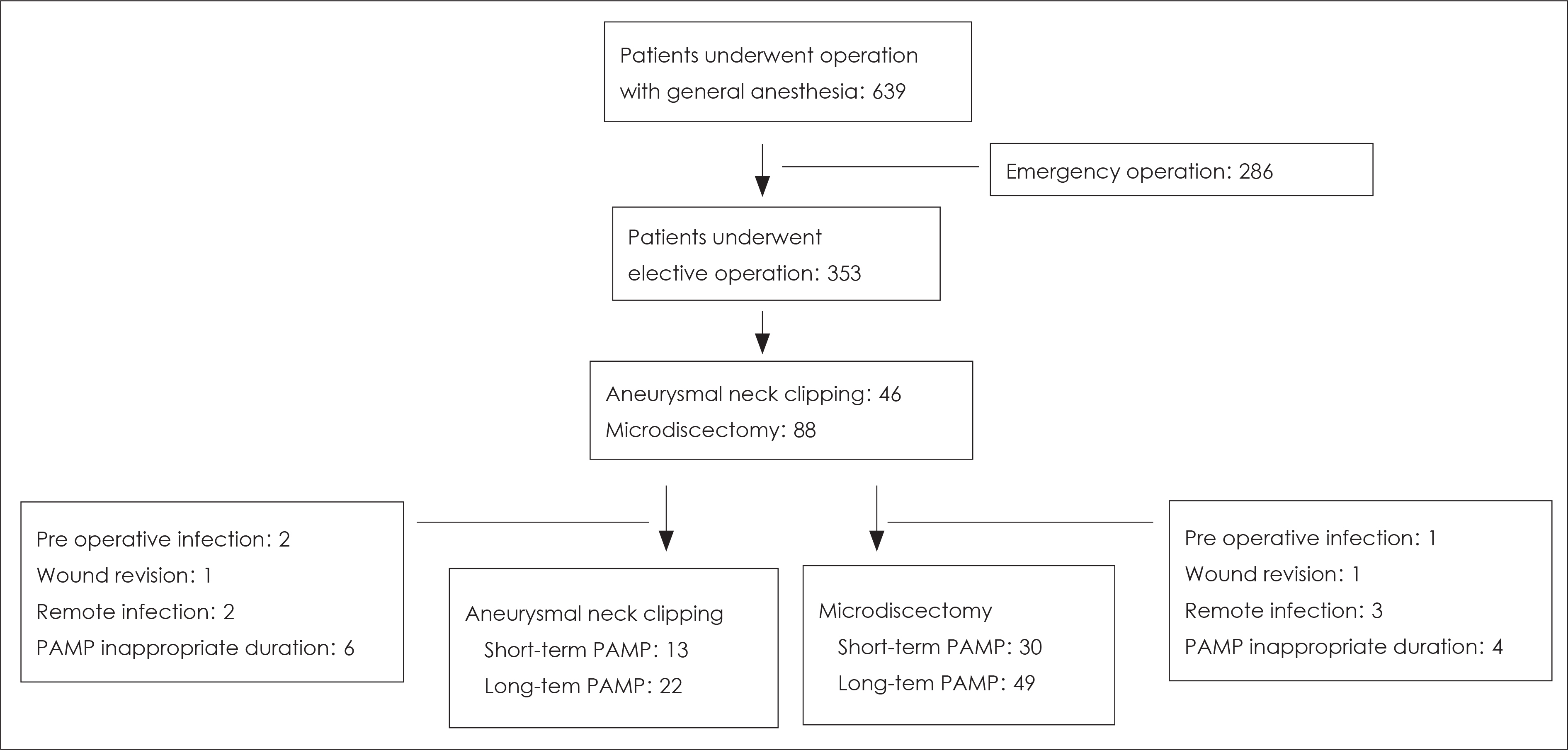
METHODS
Between April 2010 and April 2012, we retrospectively analyzed the data of 35 patients in the aneurysmal neck clipping groups (short-term PAMP group: PAMP for 3 days and fewer, long-term PAMP group: PAMP for 10 days and more) and 79 patients in the microdiscectomy groups (short-term PAMP group: 3 days and fewer, long-term PAMP group: PAMP for 6 days and more).
RESULTS
In aneurysmal neck clipping groups, SSI occurred 23.1% of short-term PAMP group and 9.1% of long-term PAMP group (p=0.3370). And in microdiscectomy groups, SSI occurred 6.7% of short-term PAMP group and 4.1% of long-term PAMP group (p=0.9840).
CONCLUSION
There is no significant difference between the short-term PAMP group and the long-term PAMP group in terms of SSI, regardless of operation type. We therefore suggest that short-term PAMP usage could be an appropriate therapy for preventing SSI in clean neurosurgical operations.
MeSH Terms
Figure
Reference
-
1). Antimicrobial prophylaxis in neurosurgery and after head injury. Infection in Neurosurgery Working Party of the British Society for Antimicrobial Chemotherapy. Lancet. 344:1547–1551. 1994.2). ASHP Therapeutic Guidelines on Antimicrobial Prophylaxis in Surgery. American Society of Health-System Pharmacists. Am J Health Syst Pharm. 56:1839–1888. 1999.3). Barker FG 2nd. Efficacy of prophylactic antibiotic therapy in spinal surgery: a meta-analysis. Neurosurgery. 51:391–400. discussion 400-401. 2002.
Article4). Barker FG 2nd. Efficacy of prophylactic antibiotics against meningitis after craniotomy: a meta-analysis. Neurosurgery. 60:887–894. discussion 887-894. 2007.
Article5). Brown EM. Antimicrobial prophylaxis in neurosurgery. J Antimicrob Chemother 31 Suppl B: 49-63. 1993.
Article6). Castella A., Charrier L., Di Legami V., Pastorino F., Farina EC., Ar-gentero PA, et al. Surgical site infection surveillance: analysis of adherence to recommendations for routine infection control practices. Infect Control Hosp Epidemiol. 27:835–840. 2006.
Article7). de Lissovoy G., Fraeman K., Hutchins V., Murphy D., Song D., Vaughn BB. Surgical site infection: incidence and impact on hospital utilization and treatment costs. Am J Infect Control. 37:387–397. 2009.
Article8). Dellinger EP., Gross PA., Barrett TL., Krause PJ., Martone WJ., Mc-Gowan JE Jr, et al. Quality standard for antimicrobial prophylaxis in surgical procedures. The Infectious Diseases Society of America. Infect Control Hosp Epidemiol. 15:182–188. 1994.9). Durando P., Bassetti M., Orengo G., Crimi P., Battistini A., Bellina D, et al. Adherence to international and national recommendations for the prevention of surgical site infections in Italy: Results from an observational prospective study in elective surgery. Am J Infect Control, 2012 [Epub ahead of print].10). Fry DE. Fifty ways to cause surgical site infections. Surg Infect (Larchmt). 12:497–500. 2011.
Article11). Korinek AM., Baugnon T., Golmard JL., van Effenterre R., Coriat P., Puybasset L. Risk factors for adult nosocomial meningitis after craniotomy: role of antibiotic prophylaxis. Neurosurgery 62 Suppl. 2:532–539. 2008.12). Korinek AM., Golmard JL., Elcheick A., Bismuth R., van Effenterre R., Coriat P, et al. Risk factors for neurosurgical site infections after craniotomy: a critical reappraisal of antibiotic prophylaxis on 4,578 patients. Br J Neurosurg. 19:155–162. 2005.
Article13). Lee KY., Coleman K., Paech D., Norris S., Tan JT. The epidemiology and cost of surgical site infections in Korea: a systematic review. J Korean Surg Soc. 81:295–307. 2011.
Article14). Lietard C., Thébaud V., Besson G., Lejeune B. Risk factors for neurosurgical site infections: an 18-month prospective survey. J Neurosurg. 109:729–734. 2008.
Article15). Mangram AJ., Horan TC., Pearson ML., Silver LC., Jarvis WR. Guideline for Prevention of Surgical Site Infection, 1999. Centers for Disease Control and Prevention (CDC) Hospital Infection Control Practices Advisory Committee. Am J Infect Control. 27:97–132. quiz 133-134; discussion 96. 1999.16). Nichols RL. Surgical antibiotic prophylaxis. Med Clin North Am. 79:509–522. 1995.
Article17). Patir R., Mahapatra AK., Banerji AK. Risk factors in postoperative neurosurgical infection. A prospective study. Acta Neurochir (Wien). 119:80–84. 1992.18). Pople I., Poon W., Assaker R., Mathieu D., Iantosca M., Wang E, et al. Comparison of infection rate with the use of antibiotic-impregnated vs standard extraventricular drainage devices: a prospective, randomized controlled trial. Neurosurgery. 71:6–13. 2012.19). Ryska O., Serclová Z., Konecná E., Fulík J., Kneifl T., Dytrych P, et al. [Antibiotic prophylaxis in acute surgical procedures—the current praxis in Czech Republic]. Rozhl Chir. 90:402–407. 2011.20). Tanner J., Swarbrook S., Stuart J. Surgical hand antisepsis to reduce surgical site infection. Cochrane Database Syst Rev: CD004288. 2008.
Article21). Waddell TK., Rotstein OD. Antimicrobial prophylaxis in surgery. Committee on Antimicrobial Agents, Canadian Infectious Disease Society. CMAJ. 151:925–931. 1994.22). Webster J., Osborne S. Preoperative bathing or showering with skin antiseptics to prevent surgical site infection. Cochrane Database Syst Rev: CD004985. 2006.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Antimicrobial Prophylaxis in Urological Surgery
- Appropriate Administration of Prophylactic Antibiotics in Clean Operations: A Preliminary Report
- Antimicrobial Prophylaxis for Recurrent Urinary Tract Infection
- Antimicrobial Prophylaxis in Instrumented Spinal Fusion Surgery: A Comparative Analysis of 24-Hour and 72-Hour Dosages
- Long-term Efficacy and Safety of Risperidone in Patients with Schizophrenia