Yonsei Med J.
2012 Nov;53(6):1224-1227. 10.3349/ymj.2012.53.6.1224.
Malignant Hypertension with an Unusual Presentation Mimicking the Immune Mediated Pulmonary Renal Syndrome
- Affiliations
-
- 1Division of Nephrology, Department of Internal Medicine, The Catholic University of Korea, School of Medicine, Seoul, Korea. sooncb@catholic.ac.kr
- KMID: 1414269
- DOI: http://doi.org/10.3349/ymj.2012.53.6.1224
Abstract
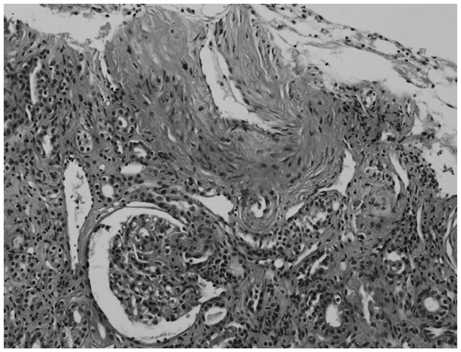
- A 27-year-old man presented at the emergency room with hemoptysis. His blood pressure was 180/100 mm Hg, and he had no history of hypertension. Chest radiographs showed bilateral infiltration, suggestive of alveolar hemorrhage. His laboratory data were consistent with acute kidney injury. His serum creatinine level increased abruptly; therefore, renal biopsy was performed. Steroid pulse therapy was administered because of a strong suspicion of immune-mediated pulmonary renal syndrome. Renal biopsy showed proliferative endarteritis, fibrinoid necrosis, and intraluminal thrombi in the vessels without crescent formation or necrotizing lesions. Steroid pulse therapy rapidly tapered and stopped. His serum creatinine level gradually decreased with strict blood pressure control. Ten months after discharge, his blood pressure was approximately 120/80 mm Hg with a serum creatinine level of 1.98 mg/dL. Pulmonary renal syndrome is generally caused by an immune-mediated mechanism. However, malignant hypertension accompanying renal insufficiency and heart dysfunction causing end-organ damage can create a pulmonary hemorrhage, similar to pulmonary renal syndrome caused by an immune-mediated mechanism. The present case shows that hypertension, a common disease, can possibly cause pulmonary renal syndrome, a rare condition.
MeSH Terms
Figure
Reference
-
1. Hida K, Wada J, Odawara M, Kunitomi M, Hayakawa N, Kashihara N, et al. Malignant hypertension with a rare complication of pulmonary alveolar hemorrhage. Am J Nephrol. 2000. 20:64–67.
Article2. Hirayama K, Yamagata K, Kobayashi M, Koyama A. Anti-glomerular basement membrane antibody disease in Japan: part of the nationwide rapidly progressive glomerulonephritis survey in Japan. Clin Exp Nephrol. 2008. 12:339–347.
Article3. Slama M, Modeliar SS. Hypertension in the intensive care unit. Curr Opin Cardiol. 2006. 21:279–287.
Article4. Haas AR, Marik PE. Current diagnosis and management of hypertensive emergency. Semin Dial. 2006. 19:502–512.5. Sato Y, Hara S, Yamada K, Fujimoto S. A rare case of alveolar haemorrhage due to malignant hypertension. Nephrol Dial Transplant. 2005. 20:2289–2290.
Article6. Aithal S, Marley N, Venkat-Raman G. An unusual non-immunological cause of renal pulmonary syndrome. Clin Nephrol. 2009. 72:322–325.
Article7. Agarwal M, Lynn KL, Richards AM, Nicholls MG. Hyponatremic-hypertensive syndrome with renal ischemia: an underrecognized disorder. Hypertension. 1999. 33:1020–1024.
Article8. Saxena R, Isaksson B, Bygren P, Wieslander J. A rapid assay for circulating anti-glomerular basement membrane antibodies in Goodpasture syndrome. J Immunol Methods. 1989. 118:73–78.
Article9. Westman KW, Bygren PG, Eilert I, Wiik A, Wieslander J. Rapid screening assay for anti-GBM antibody and ANCAs; an important tool for the differential diagnosis of pulmonary renal syndromes. Nephrol Dial Transplant. 1997. 12:1863–1868.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Noonan Syndrome Presenting with Malignant Hypertension in an Adult
- Middle Aortic Syndrome with Superior Mesenteric and Bilateral Renal Artery Involvement: Unusual Type of Aortic Coarctation
- Malignant Hypertension with Pulmonary Alveolar Hemorrhage Needing Dialysis
- A Case of Cerebellar Infarction with Renal Artery Stenosis
- Furosemide induced medullary nephrocalcinosis mimicking Bartter syndrome