Korean J Radiol.
2012 Dec;13(6):694-701. 10.3348/kjr.2012.13.6.694.
CT-Guided Percutaneous Transthoracic Localization of Pulmonary Nodules Prior to Video-Assisted Thoracoscopic Surgery Using Barium Suspension
- Affiliations
-
- 1Department of Radiology, Seoul National University College of Medicine, and Institute of Radiation Medicine, Seoul National University Medical Research Center, Seoul 110-744, Korea. cmpark@radiol.snu.ac.kr
- 2Department of Thoracic and Cardiovascular Surgery, Seoul National University College of Medicine, Seoul 110-744, Korea.
- 3Department of Pathology, Seoul National University College of Medicine, Seoul 110-744, Korea.
- KMID: 1397499
- DOI: http://doi.org/10.3348/kjr.2012.13.6.694
Abstract
OBJECTIVE
To describe our initial experience with CT-guided percutaneous barium marking for the localization of small pulmonary nodules prior to video-assisted thoracoscopic surgery (VATS).
MATERIALS AND METHODS
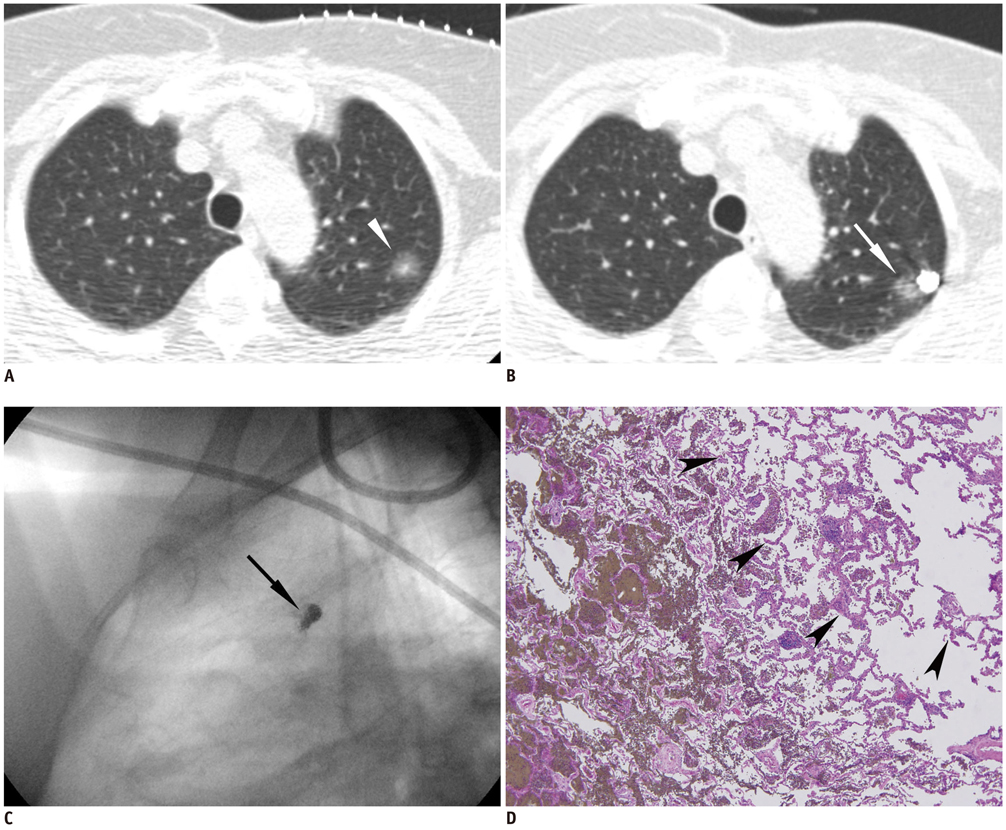
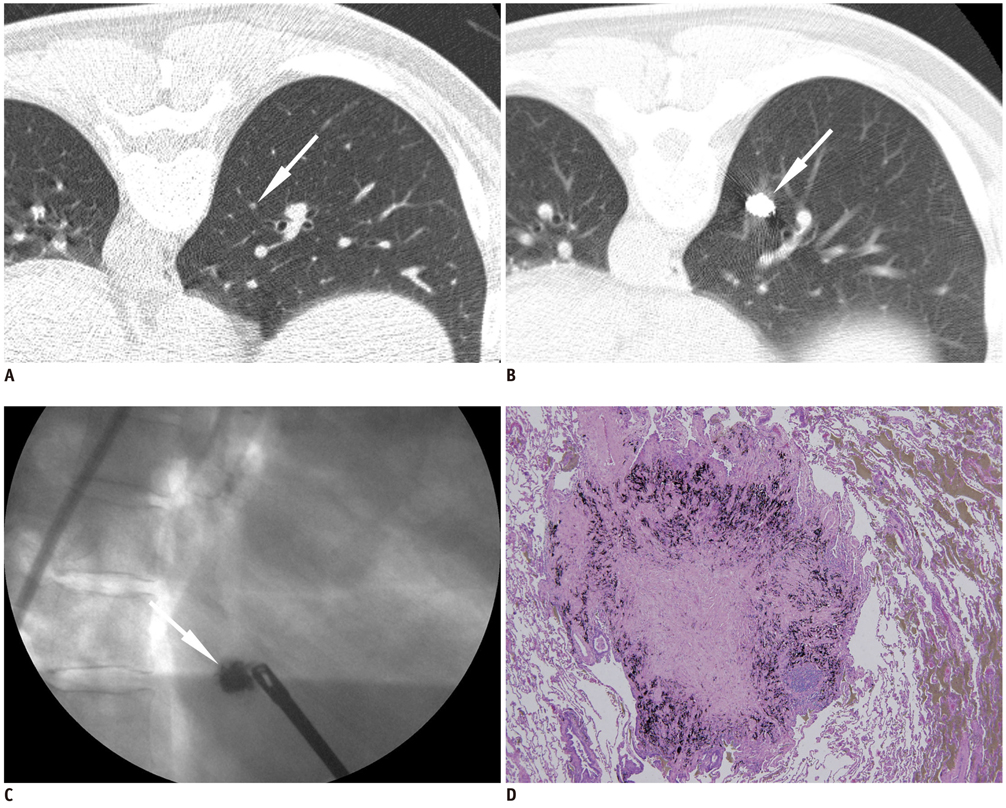
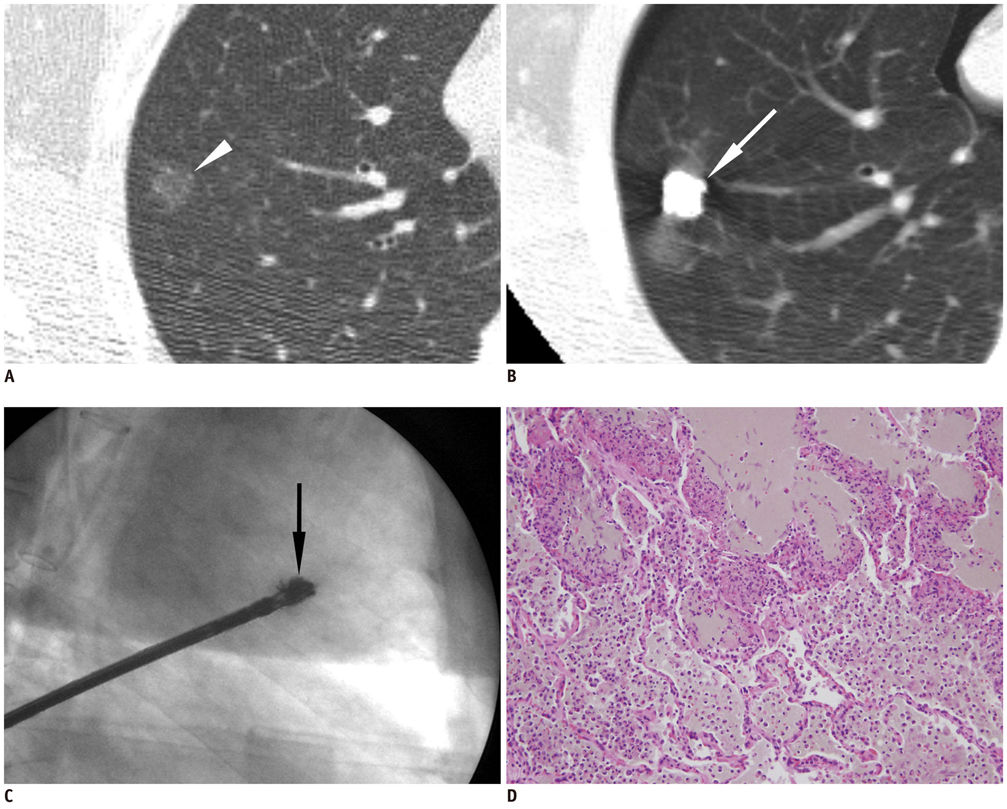
From October 2010 to April 2011, 10 consecutive patients (4 men and 6 women; mean age, 60 years) underwent CT-guided percutaneous barium marking for the localization of 10 small pulmonary nodules (mean size, 7.6 mm; range, 3-14 mm): 6 pure ground-glass nodules, 3 part-solid nodules, and 1 solid nodule. A 140% barium sulfate suspension (mean amount, 0.2 mL; range, 0.15-0.25 mL) was injected around the nodules with a 21-gauge needle. The technical details, surgical findings and pathologic features associated with barium localizations were evaluated.
RESULTS
All nodules were marked within 3 mm (mean distance, 1.1 mm; range, 0-3 mm) from the barium ball (mean diameter, 9.6 mm; range, 8-16 mm) formed by the injected barium suspension. Pneumothorax occurred in two cases, for which one needed aspiration. However, there were no other complications. All barium balls were palpable during VATS and visible on intraoperative fluoroscopy, and were completely resected. Both the whitish barium balls and target nodules were identifiable in the frozen specimens. Pathology revealed one invasive adenocarcinoma, five adenocarcinoma-in-situ, two atypical adenomatous hyperplasias, and two benign lesions. In all cases, there were acute inflammations around the barium balls which did not hamper the histological diagnosis of the nodules.
CONCLUSION
CT-guided percutaneous barium marking can be an effective, convenient and safe pre-operative localization procedure prior to VATS, enabling accurate resection and diagnosis of small or faint pulmonary nodules.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Planting Seeds into the Lung: Image-Guided Percutaneous Localization to Guide Minimally Invasive Thoracic Surgery
Ji Won Lee, Chul Hwan Park, Sang Min Lee, Miri Jeong, Jin Hur
Korean J Radiol. 2019;20(11):1498-1514. doi: 10.3348/kjr.2019.0155.
Reference
-
1. Pastorino U. Lung cancer screening. Br J Cancer. 2010. 102:1681–1686.2. Swensen SJ, Jett JR, Hartman TE, Midthun DE, Mandrekar SJ, Hillman SL, et al. CT screening for lung cancer: five-year prospective experience. Radiology. 2005. 235:259–265.3. Henschke CI, McCauley DI, Yankelevitz DF, Naidich DP, McGuinness G, Miettinen OS, et al. Early Lung Cancer Action Project: overall design and findings from baseline screening. Lancet. 1999. 354:99–105.4. Henschke CI, Yankelevitz DF, Mirtcheva R, McGuinness G, McCauley D, Miettinen OS. ELCAP Group. CT screening for lung cancer: frequency and significance of part-solid and nonsolid nodules. AJR Am J Roentgenol. 2002. 178:1053–1057.5. Congregado M, Merchan RJ, Gallardo G, Ayarra J, Loscertales J. Video-assisted thoracic surgery (VATS) lobectomy: 13 years' experience. Surg Endosc. 2008. 22:1852–1857.6. Karasaki T, Nakajima J, Murakawa T, Fukami T, Yoshida Y, Kusakabe M, et al. Video-assisted thoracic surgery lobectomy preserves more latissimus dorsi muscle than conventional surgery. Interact Cardiovasc Thorac Surg. 2009. 8:316–319. discussion 319-320.7. Chen S, Zhou J, Zhang J, Hu H, Luo X, Zhang Y, et al. Video-assisted thoracoscopic solitary pulmonary nodule resection after CT-guided hookwire localization: 43 cases report and literature review. Surg Endosc. 2011. 25:1723–1729.8. Horan TA, Pinheiro PM, Araújo LM, Santiago FF, Rodrigues MR. Massive gas embolism during pulmonary nodule hook wire localization. Ann Thorac Surg. 2002. 73:1647–1649.9. Iguchi T, Yoshioka T, Muro M, Miyasho K, Inoue D, Hiraki T, et al. Systemic air embolism during preoperative pulmonary marking with a short hook wire and suture system under CT fluoroscopy guidance. Jpn J Radiol. 2009. 27:385–388.10. Kobayashi T, Kaneko M, Kondo H, Nakayama H, Asamura H, Tsuchiya R, et al. CT-guided bronchoscopic barium marking for resection of a fluoroscopically invisible peripheral pulmonary lesion. Jpn J Clin Oncol. 1997. 27:204–205.11. Okumura T, Kondo H, Suzuki K, Asamura H, Kobayashi T, Kaneko M, et al. Fluoroscopy-assisted thoracoscopic surgery after computed tomography-guided bronchoscopic barium marking. Ann Thorac Surg. 2001. 71:439–442.12. Asano F, Shindoh J, Shigemitsu K, Miya K, Abe T, Horiba M, et al. Ultrathin bronchoscopic barium marking with virtual bronchoscopic navigation for fluoroscopy-assisted thoracoscopic surgery. Chest. 2004. 126:1687–1693.13. Iwasaki Y, Nagata K, Yuba T, Hosogi S, Kohno K, Ohsugi S, et al. Fluoroscopy-guided barium marking for localizing small pulmonary lesions before video-assisted thoracic surgery. Respir Med. 2005. 99:285–289.14. Suzuki K, Nagai K, Yoshida J, Ohmatsu H, Takahashi K, Nishimura M, et al. Video-assisted thoracoscopic surgery for small indeterminate pulmonary nodules: indications for preoperative marking. Chest. 1999. 115:563–568.15. Wang YZ, Boudreaux JP, Dowling A, Woltering EA. Percutaneous localisation of pulmonary nodules prior to video-assisted thoracoscopic surgery using methylene blue and TC-99. Eur J Cardiothorac Surg. 2010. 37:237–238.16. Nomori H, Horio H. Colored collagen is a long-lasting point marker for small pulmonary nodules in thoracoscopic operations. Ann Thorac Surg. 1996. 61:1070–1073.17. Kwon WJ, Kim HJ, Jeong YJ, Lee CH, Kim KI, Kim YD, et al. Direct lipiodol injection used for a radio-opaque lung marker: stability and histopathologic effects. Exp Lung Res. 2011. 37:310–317.18. Kawanaka K, Nomori H, Mori T, Ikeda K, Ikeda O, Tomiguchi S, et al. Marking of small pulmonary nodules before thoracoscopic resection: injection of lipiodol under CT-fluoroscopic guidance. Acad Radiol. 2009. 16:39–45.19. Moon SW, Wang YP, Jo KH, Kwack MS, Kim SW, Kwon OK, et al. Fluoroscopy-aided thoracoscopic resection of pulmonary nodule localized with contrast media. Ann Thorac Surg. 1999. 68:1815–1820.20. Federici S, Ratta A, Mordenti M, Domenichell V, Pelusi G, Italiano F, et al. Successful thoracoscopic resection of pulmonary metastasis less than 1 cm in size utilizing preoperative CT-guided wire localization. J Laparoendosc Adv Surg Tech A. 2009. 19:Suppl 1. S171–S173.21. Chen YR, Yeow KM, Lee JY, Su IH, Chu SY, Lee CH, et al. CT-guided hook wire localization of subpleural lung lesions for video-assisted thoracoscopic surgery (VATS). J Formos Med Assoc. 2007. 106:911–918.22. Lizza N, Eucher P, Haxhe JP, De Wispelaere JF, Johnson PM, Delaunois L. Thoracoscopic resection of pulmonary nodules after computed tomographic-guided coil labeling. Ann Thorac Surg. 2001. 71:986–988.23. Mayo JR, Clifton JC, Powell TI, English JC, Evans KG, Yee J, et al. Lung nodules: CT-guided placement of microcoils to direct video-assisted thoracoscopic surgical resection. Radiology. 2009. 250:576–585.24. Felton WL. The reaction of pulmonary tissue to lipiodol. J Thorac Surg. 1953. 25:530–542.25. Erickson LM, Shaw D, MacDonald FR. Prolonged barium retention in the lung following bronchography. Radiology. 1979. 130:635–636.26. Gray C, Sivaloganathan S, Simpkins KC. Aspiration of high-density barium contrast medium causing acute pulmonary inflammation--report of two fatal cases in elderly women with disordered swallowing. Clin Radiol. 1989. 40:397–400.27. Ginai AZ, ten Kate FJ, ten Berg RG, Hoornstra K. Experimental evaluation of various available contrast agents for use in the upper gastrointestinal tract in case of suspected leakage. Effects on lungs. Br J Radiol. 1984. 57:895–890.28. Thompson IM, Whittlesey GC, Slovis TL, Chang CH, Cullen ML, Philippart AI, et al. Evaluation of contrast media for bronchography. Pediatr Radiol. 1997. 27:598–605.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Planting Seeds into the Lung: Image-Guided Percutaneous Localization to Guide Minimally Invasive Thoracic Surgery
- CT-Guided Microcoil Localization of Small Peripheral Pulmonary Nodules to Direct Video-Assisted Thoracoscopic Resection without the Aid of Intraoperative Fluoroscopy
- Percutaneous Electromagnetic Transthoracic Nodule Localization for Ground Glass Nodules
- Computed Tomography Guided Percutaneous Injection of a Mixture of Lipiodol and Methylene Blue in Rabbit Lungs: Evaluation of Localization Ability for Video-Assisted Thoracoscopic Surgery
- Computed Tomography-guided Localization with a Hook-wire Followed by Video-assistedThoracic Surgery for Small Intrapulmonary and Ground Glass Opacity Lesions