Korean J Radiol.
2012 Aug;13(4):403-411. 10.3348/kjr.2012.13.4.403.
Differentiation between Symptomatic and Asymptomatic Extraforaminal Stenosis in Lumbosacral Transitional Vertebra: Role of Three-Dimensional Magnetic Resonance Lumbosacral Radiculography
- Affiliations
-
- 1Department of Diagnostic Radiology, College of Medicine, Yeungnam University, Daegu 705-717, Korea. wmbyun@yu.ac.kr
- KMID: 1383851
- DOI: http://doi.org/10.3348/kjr.2012.13.4.403
Abstract
OBJECTIVE
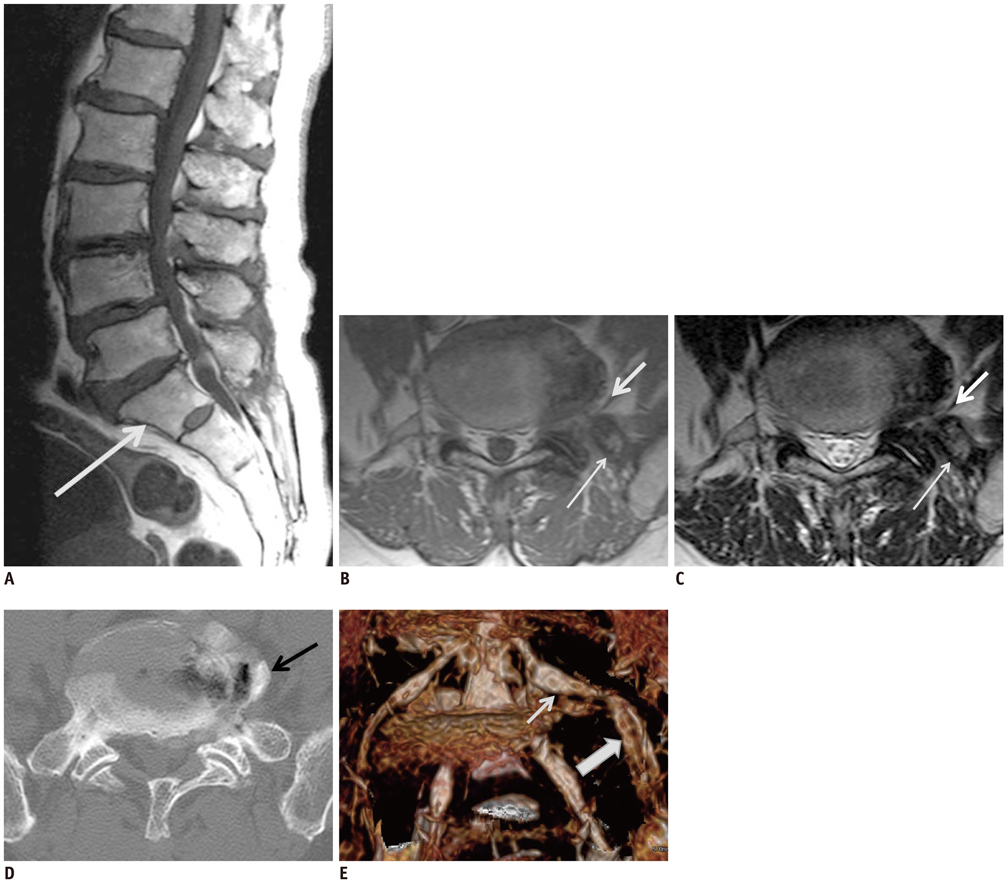
To investigate the role of lumbosacral radiculography using 3-dimentional (3D) magnetic resonance (MR) rendering for diagnostic information of symptomatic extraforaminal stenosis in lumbosacral transitional vertebra.
MATERIALS AND METHODS
The study population consisted of 18 patients with symptomatic (n = 10) and asymptomatic extraforaminal stenosis (n = 8) in lumbosacral transitional vertebra. Each patient underwent 3D coronal fast-field echo sequences with selective water excitation using the principles of the selective excitation technique (Proset imaging). Morphologic changes of the L5 nerve roots at the symptomatic and asymptomatic extraforaminal stenosis were evaluated on 3D MR rendered images of the lumbosacral spine.
RESULTS
Ten cases with symptomatic extraforaminal stenosis showed hyperplasia and degenerative osteophytes of the sacral ala and/or osteophytes at the lateral margin of the L5 body. On 3D MR lumbosacral radiculography, indentation of the L5 nerve roots was found in two cases, while swelling of the nerve roots was seen in eight cases at the exiting nerve root. Eight cases with asymptomatic extraforaminal stenosis showed hyperplasia and degenerative osteophytes of the sacral ala and/or osteophytes at the lateral margin of the L5 body. Based on 3D MR lumbosacral radiculography, indentation or swelling of the L5 nerve roots was not found in any cases with asymptomatic extraforaminal stenosis.
CONCLUSION
Results from 3D MR lumbosacral radiculography Indicate the indentation or swelling of the L5 nerve root in symptomatic extraforaminal stenosis. Based on these findings, 3D MR radiculography may be helpful in the diagnosis of the symptomatic extraforaminal stenosis with lumbosacral transitional vertebra.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Usefulness of the ProSet MRI for Diagnosis of the Extraforaminal Disc Herniation
Myun-Whan Ahn, Ui-Sik Kim, Gi-Beom Kim
J Korean Soc Spine Surg. 2013;20(1):28-33. doi: 10.4184/JKSS.2021.20.1.28.
Reference
-
1. Bron JL, van Royen BJ, Wuisman PI. The clinical significance of lumbosacral transitional anomalies. Acta Orthop Belg. 2007. 73:687–695.2. O'Driscoll CM, Irwin A, Saifuddin A. Variations in morphology of the lumbosacral junction on sagittal MRI: correlation with plain radiography. Skeletal Radiol. 1996. 25:225–230.3. Elster AD. Bertolotti's syndrome revisited. Transitional vertebrae of the lumbar spine. Spine (Phila Pa 1976). 1989. 14:1373–1377.4. Quinlan JF, Duke D, Eustace S. Bertolotti's syndrome. A cause of back pain in young people. J Bone Joint Surg Br. 2006. 88:1183–1186.5. Wiltse LL, Guyer RD, Spencer CW, Glenn WV, Porter IS. Alar transverse process impingement of the L5 spinal nerve: the far-out syndrome. Spine (Phila Pa 1976). 1984. 9:31–41.6. Abe E, Sato K, Shimada Y, Okada K, Yan K, Mizutani Y. Anterior decompression of foraminal stenosis below a lumbosacral transitional vertebra. A case report. Spine (Phila Pa 1976). 1997. 22:823–826.7. Hashimoto M, Watanabe O, Hirano H. Extraforaminal stenosis in the lumbosacral spine. Efficacy of MR imaging in the coronal plane. Acta Radiol. 1996. 37:610–613.8. Moon KH, Jang JS, Lee SH, Lee SC, Lee HY. The role of computed tomography in the presurgical diagnosis of foraminal entrapment of lumbosacral junction. J Korean Neurosurg Soc. 2010. 47:1–6.9. Boden SD, Davis DO, Dina TS, Patronas NJ, Wiesel SW. Abnormal magnetic-resonance scans of the lumbar spine in asymptomatic subjects. A prospective investigation. J Bone Joint Surg Am. 1990. 72:403–408.10. Deyo RA, Ciol MA, Cherkin DC, Loeser JD, Bigos SJ. Lumbar spinal fusion. A cohort study of complications, reoperations, and resource use in the Medicare population. Spine (Phila Pa 1976). 1993. 18:1463–1470.11. Nakao S, Yoshida M, Yamada H, Hashizume H. A new 3-dimensional computed tomography imaging method to diagnose extraforaminal stenosis at the lumbosacral junction. J Spinal Disord Tech. 2010. 23:e47–e52.12. Castellvi AE, Goldstein LA, Chan DP. Lumbosacral transitional vertebrae and their relationship with lumbar extradural defects. Spine (Phila Pa 1976). 1984. 9:493–495.13. Transfeldt EE, Robertson D, Bradford DS. Ligaments of the lumbosacral spine and their role in possible extraforaminal spinal nerve entrapment and tethering. J Spinal Disord. 1993. 6:507–512.14. Olsewski JM, Simmons EH, Kallen FC, Mendel FC. Evidence from cadavers suggestive of entrapment of fifth lumbar spinal nerves by lumbosacral ligaments. Spine (Phila Pa 1976). 1991. 16:336–347.15. Nathan H, Weizenbluth M, Halperin N. The lumbosacral ligament (LSL), with special emphasis on the "lumbosacral tunnel" and the entrapment of the 5th lumbar nerve. Int Orthop. 1982. 6:197–202.16. Otani K, Konno S, Kikuchi S. Lumbosacral transitional vertebrae and nerve-root symptoms. J Bone Joint Surg Br. 2001. 83:1137–1140.17. Matsumoto M, Chiba K, Nojiri K, Ishikawa M, Toyama Y, Nishikawa Y. Extraforaminal entrapment of the fifth lumbar spinal nerve by osteophytes of the lumbosacral spine: anatomic study and a report of four cases. Spine (Phila Pa 1976). 2002. 27:E169–E173.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Three-Dimension Magnetic Resonance Lumbosacral Radiculography by Principles of the Selective Excitation Technique Imaging in the Diagnosis of Symptomatic Foraminal Stenosis
- Low Back Pain due to Lumbosacral Transitional Vertebra
- Paramedian Tangential Approach for the Lumbosacral Extraforaminal Disc Herniations
- Far-out Stenosis by the Lumbosacral Transitional Vertebrae
- The Morphometric Analysis of the Extraforamen in the Lumbosacral Spine: Magnetic Resonance Imaging and Computed Tomography Study