J Korean Orthop Assoc.
2011 Oct;46(5):438-442.
Far-out Stenosis by the Lumbosacral Transitional Vertebrae
- Affiliations
-
- 1Department of Orthopedic Surgery, Seoul St.Mary's Hospital, The Catholic University of Korea, Seoul, Korea. boscoa@empal.com
Abstract
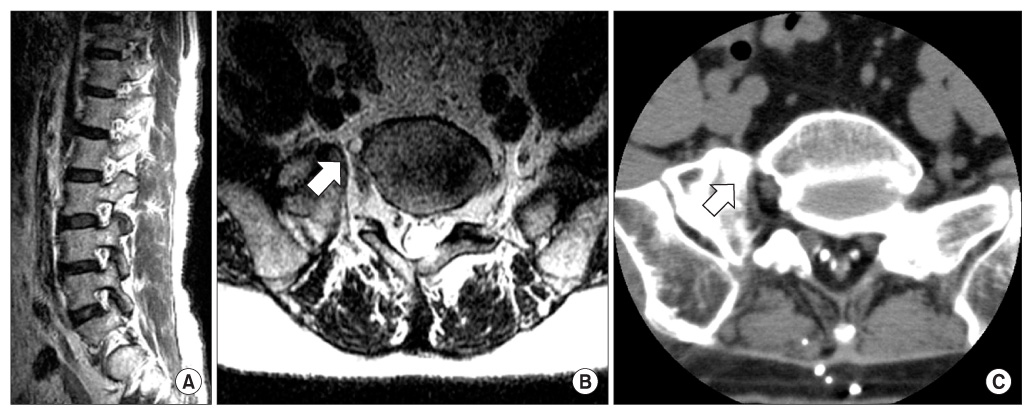
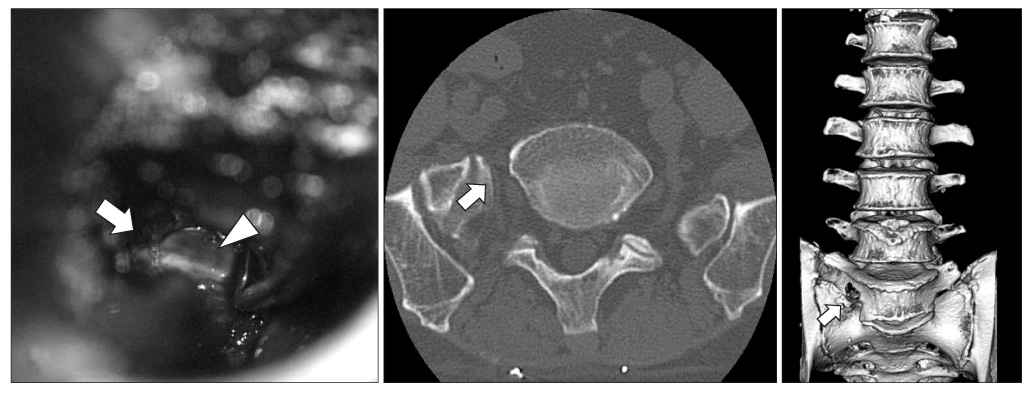
- Surgeons still have many different views on the clinical significances of the lumbosacral transitional vertebrae as one of the causes of chronic low back pain and a higher incidence of adjacent disc degeneration. Moreover, in rare case reports, compression of the exiting nerve root due to abnormal articulation between the hypertrophied transverse process and the sacral ala has been proposed as one of the reasons for the far-out lumbosacral stenosis. Anterior or posterior surgical decompression is recommended in the cases that are refractory to conservative treatment. We reviewed the related literatures and report on a case that suffered from the far-out stenosis due to lumbosacral transitional vertebra and this was successfully treated by decompression using the posterolateral approach.
MeSH Terms
Figure
Reference
-
1. Abe E, Sato K, Shimada Y, Okada K, Yan K, Mizutani Y. Anterior decompression of foraminal stenosis below a lumbosacral transitional vertebra. A case report. Spine (Phila Pa 1976). 1997. 22:823–826.2. Ichihara K, Taguchi T, Hashida T, Ochi Y, Murakami T, Kawai S. The treatment of far-out foraminal stenosis below a lumbosacral transitional vertebra: a report of two cases. J Spinal Disord Tech. 2004. 17:154–157.3. Castellvi AE, Goldstein LA, Chan DP. Lumbosacral transitional vertebrae and their relationship with lumbar extradural defects. Spine (Phila Pa 1976). 1984. 9:493–495.
Article4. Bertolotti M. Contribute alla conoscenza dei vizi di differenzazione del rachide con speciale reguardo all assimilazione sacrale della v lombare. La Radiologia Medica. 1917. 4:113–144.5. Epstein JA, Epstein NE, Marc J, Rosenthal AD, Lavine LS. Lumbar intervertebral disk herniation in teenage children: recognition and management of associated anomalies. Spine (Phila Pa 1976). 1984. 9:427–432.6. Luoma K, Vehmas T, Raininko R, Luukkonen R, Riihimäki H. Lumbosacral transitional vertebra: relation to disc degeneration and low back pain. Spine (Phila Pa 1976). 2004. 29:200–205.7. Tini PG, Wieser C, Zinn WM. The transitional vertebra of the lumbosacral spine: its radiological classification, incidence, prevalence, and clinical significance. Rheumatol Rehabil. 1977. 16:180–185.
Article8. Elster AD. Bertolotti's syndrome revisited. Transitional vertebrae of the lumbar spine. Spine (Phila Pa 1976). 1989. 14:1373–1377.9. Nathan H, Weizenbluth M, Halperin N. The lumbosacral ligament (LSL), with special emphasis on the "lumbosacral tunnel" and the entrapment of the 5th lumbar nerve. Int Orthop. 1982. 6:197–202.
Article10. Matsumoto M, Chiba K, Nojiri K, Ishikawa M, Toyama Y, Nishikawa Y. Extraforaminal entrapment of the fifth lumbar spinal nerve by osteophytes of the lumbosacral spine: anatomic study and a report of four cases. Spine (Phila Pa 1976). 2002. 27:E169–E173.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Bertolloti Syndrome
- The Role of Transitional Vertebra in Spondylolysis and Spondyloytic Spondylolisthesis
- Differentiation between Symptomatic and Asymptomatic Extraforaminal Stenosis in Lumbosacral Transitional Vertebra: Role of Three-Dimensional Magnetic Resonance Lumbosacral Radiculography
- Low Back Pain due to Lumbosacral Transitional Vertebra
- Prevalence of Lumbosacral Transitional Vertebra in Individuals with Low Back Pain: Evaluation Using Plain Radiography and Magnetic Resonance Imaging