Korean J Radiol.
2012 Apr;13(2):210-226. 10.3348/kjr.2012.13.2.210.
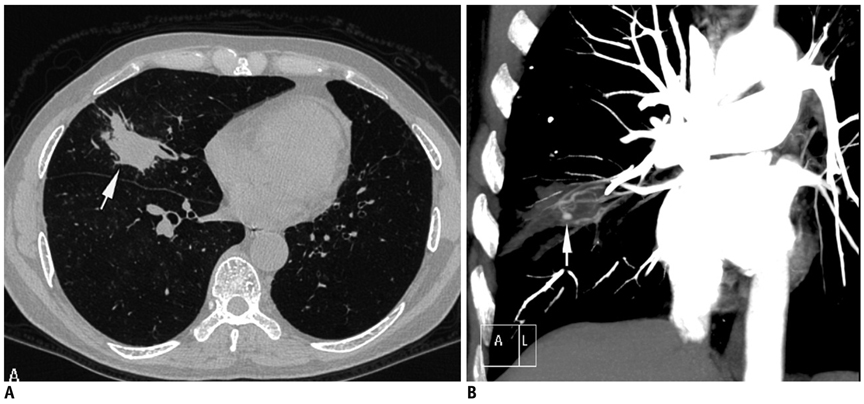
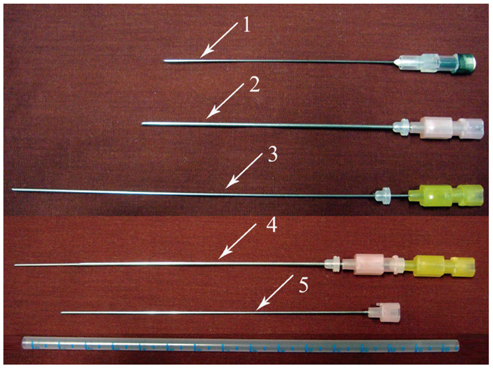
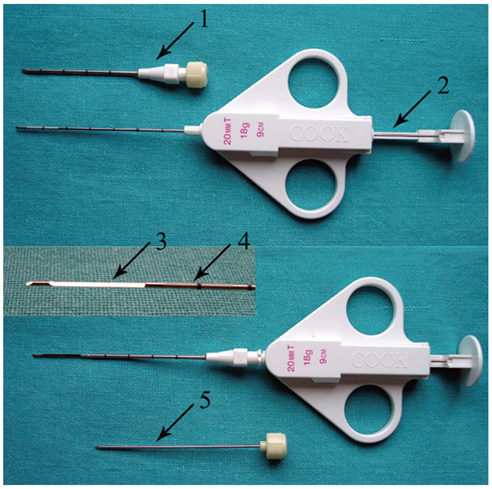
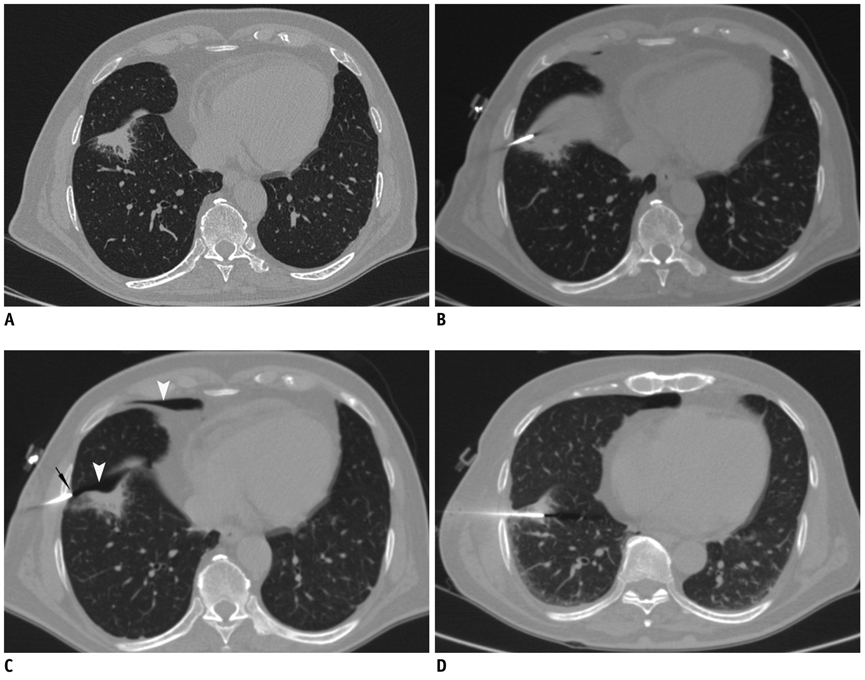
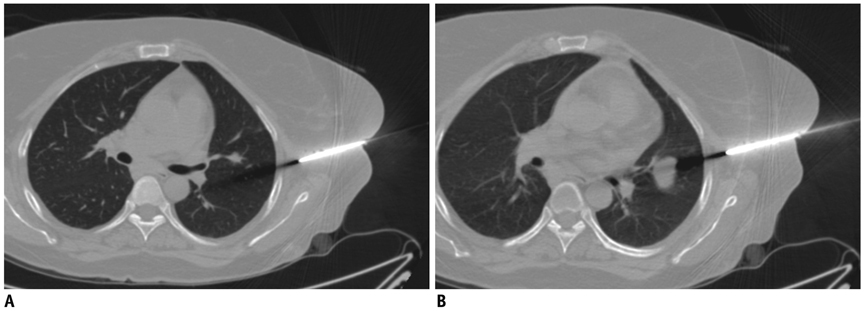
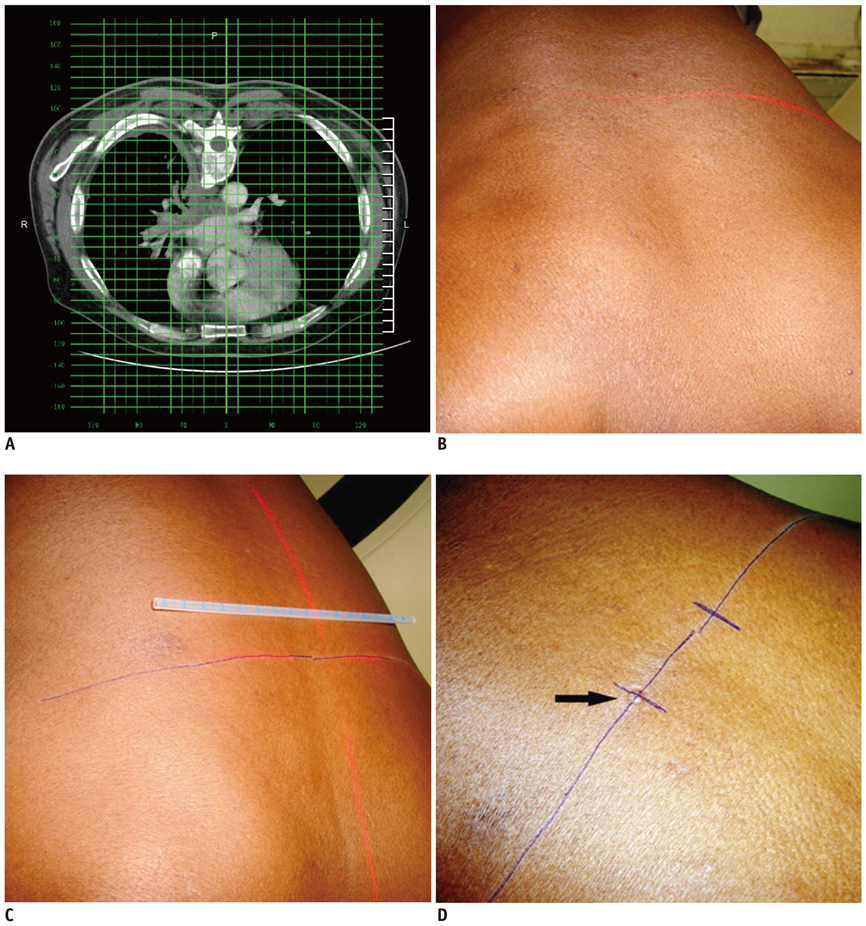
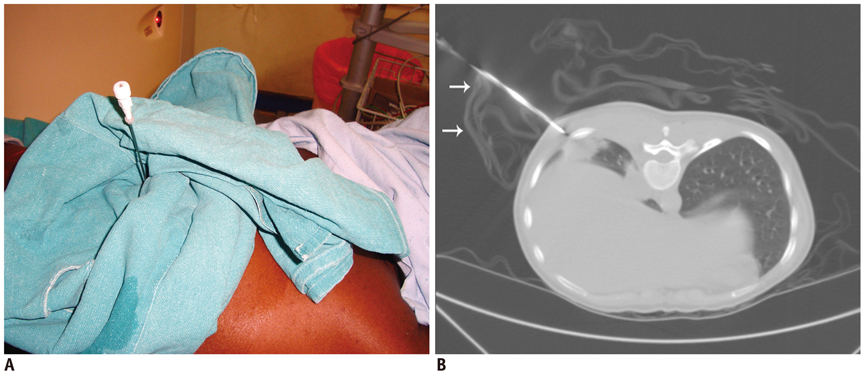
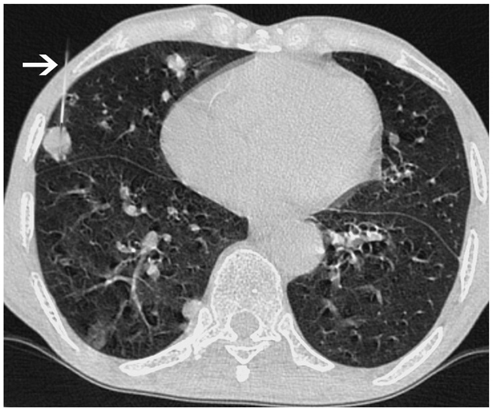
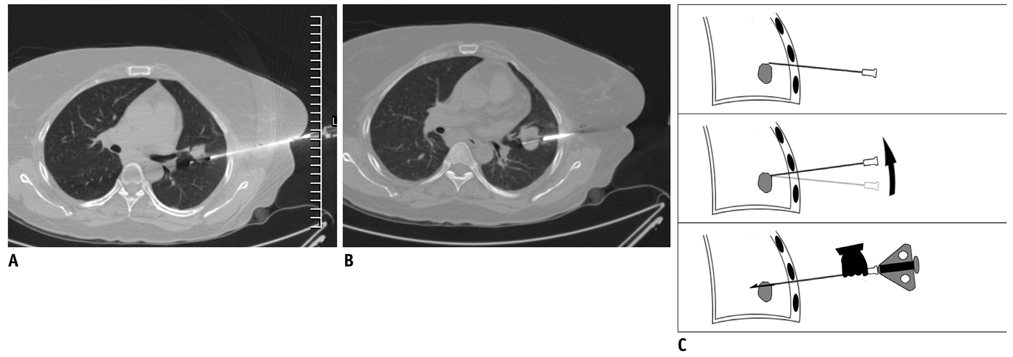
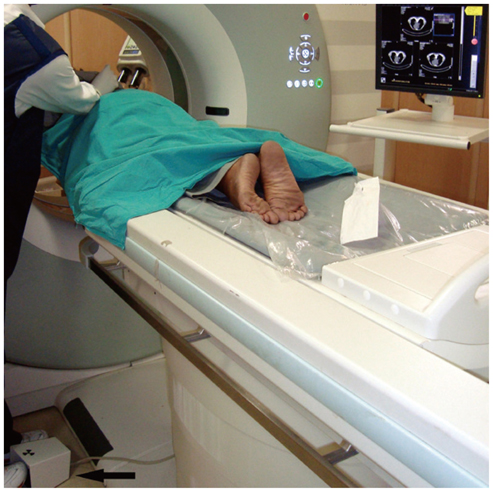
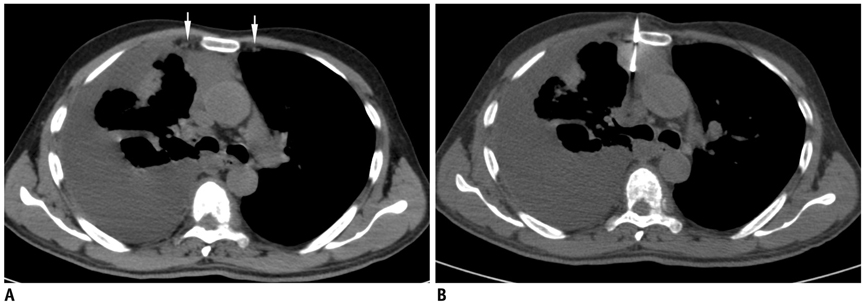
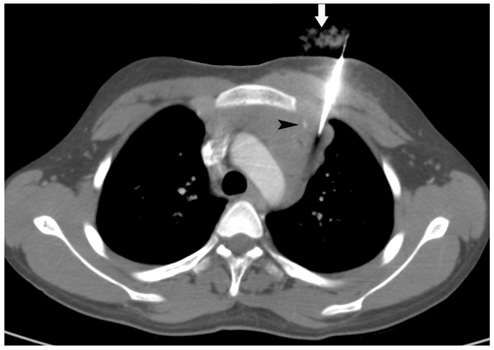
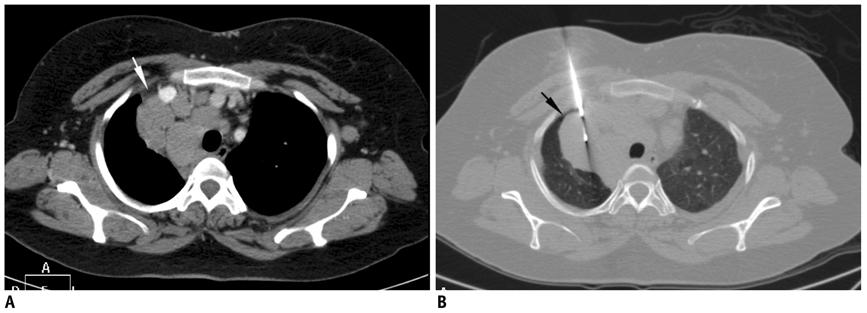
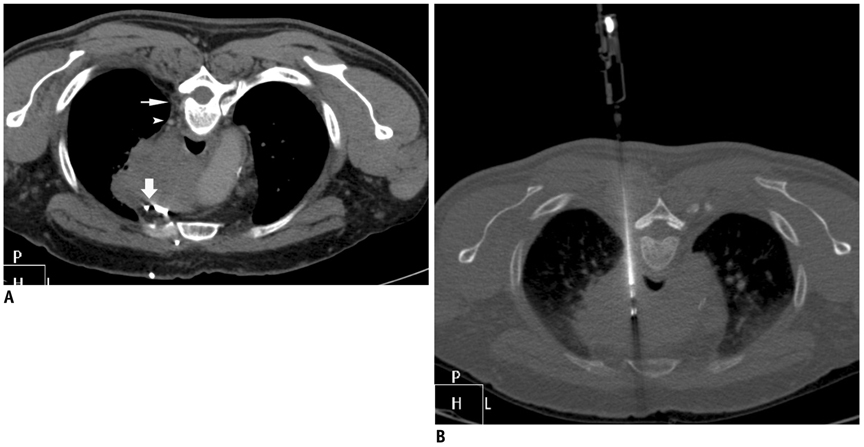
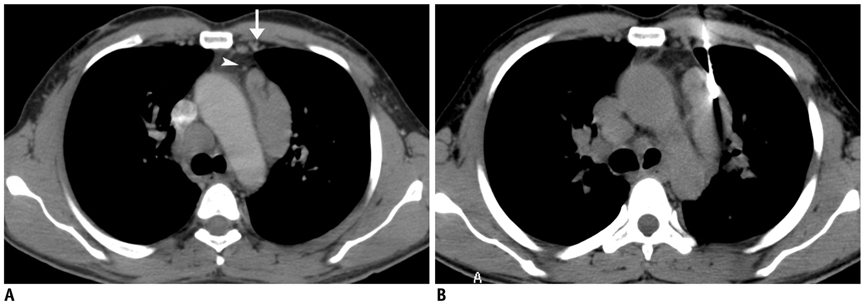
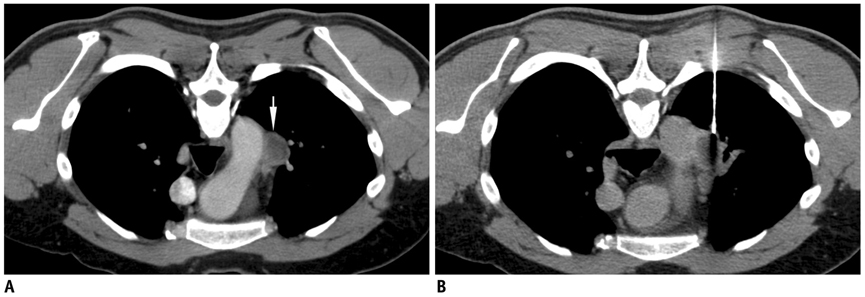
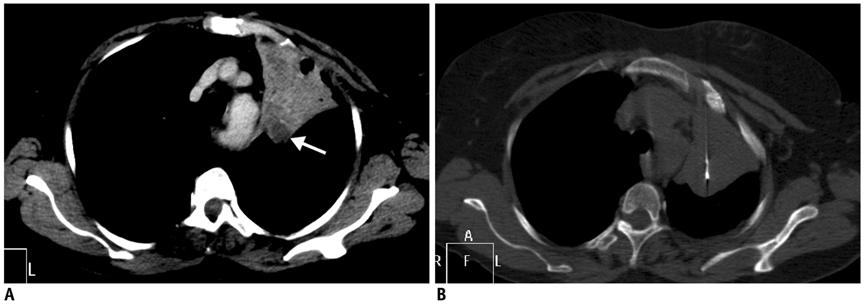
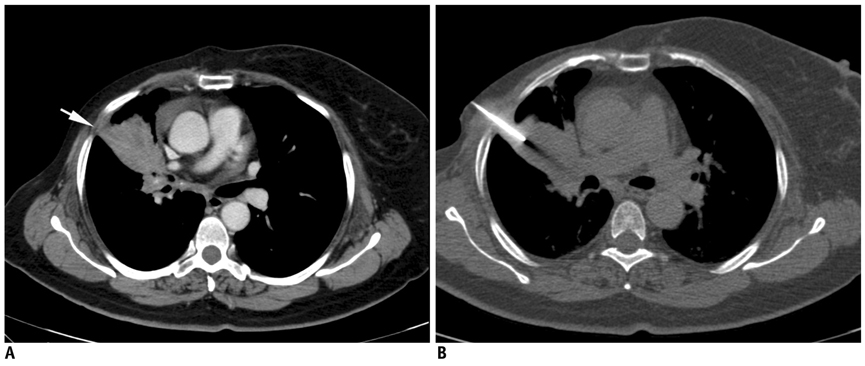
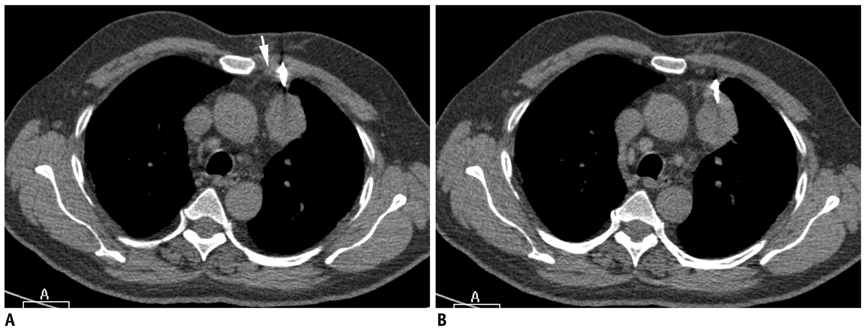
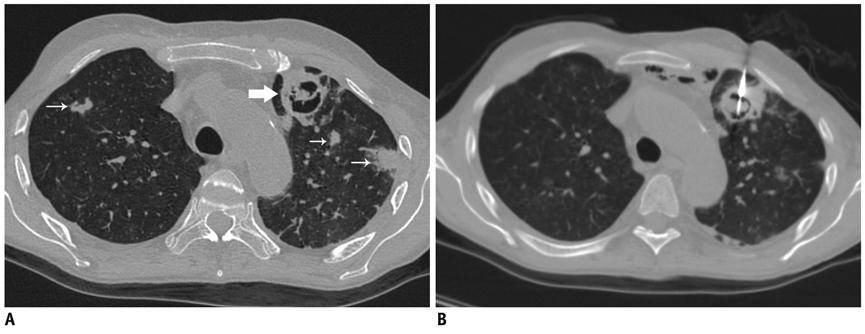
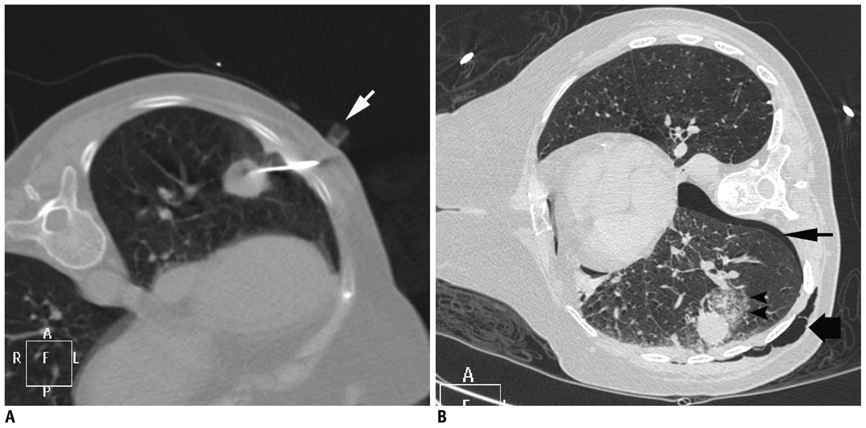
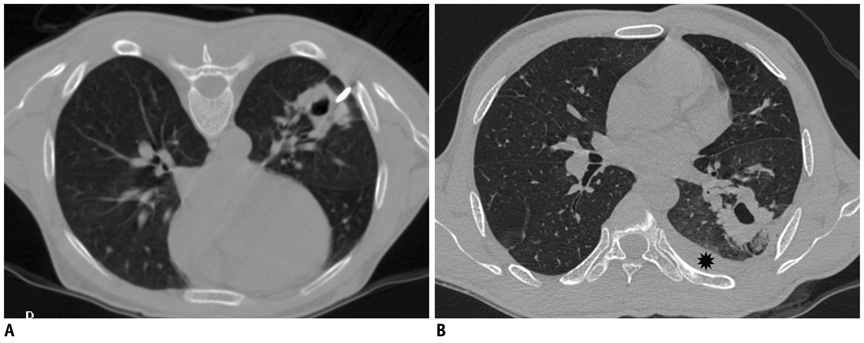
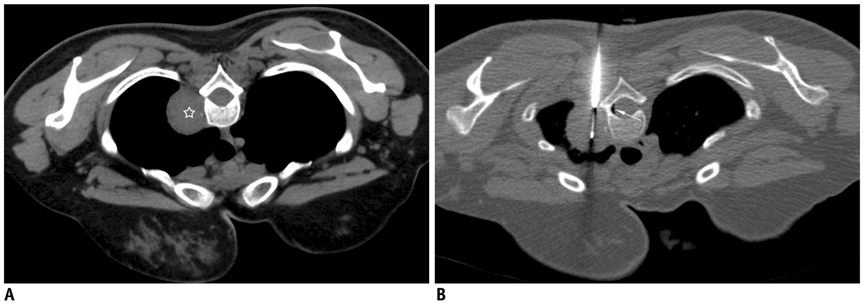
CT-Guided Percutaneous Biopsy of Intrathoracic Lesions
- Affiliations
-
- 1Department of Radiodiagnosis, Sanjay Gandhi Post Graduate Institute of Medical Sciences, Lucknow, Uttar Pradesh 226014, India. zafarneyaz@hotmail.com
- 2Department of Pulmonary Medicine, Sanjay Gandhi Post Graduate Institute of Medical Sciences, Lucknow, Uttar Pradesh 226014, India.
- KMID: 1245386
- DOI: http://doi.org/10.3348/kjr.2012.13.2.210
Abstract
- Percutaneous CT-guided needle biopsy of mediastinal and pulmonary lesions is a minimally invasive approach for obtaining tissue for histopathological examination. Although it is a widely accepted procedure with relatively few complications, precise planning and detailed knowledge of various aspects of the biopsy procedure is mandatory to avert complications. In this pictorial review, we reviewed important anatomical approaches, technical aspects of the procedure, and its associated complications.
MeSH Terms
Figure
Reference
-
1. Klein JS, Salomon G, Stewart EA. Transthoracic needle biopsy with a coaxially placed 20-gauge automated cutting needle: results in 122 patients. Radiology. 1996. 198:715–720.2. Manhire A, Charig M, Clelland C, Gleeson F, Miller R, Moss H, et al. Guidelines for radiologically guided lung biopsy. Thorax. 2003. 58:920–936.3. Cham MD, Henschke CI, Yankelevitz DF. Kandarpa K, Machan L, editors. Biopsy procedures of the lung, mediastnum, and chest wall. Handbook of interventional radiologic procedures. 2011. 4th ed. Philadelphia, USA: Wolters Kluwer/Lippincott Williams & Wilkins;478–485.4. Cham MD, Lane ME, Henschke CI, Yankelevitz DF. Lung biopsy: special techniques. Semin Respir Crit Care Med. 2008. 29:335–349.5. Gupta S, Seaberg K, Wallace MJ, Madoff DC, Morello FA Jr, Ahrar K, et al. Imaging-guided percutaneous biopsy of mediastinal lesions: different approaches and anatomic considerations. Radiographics. 2005. 25:763–788.6. Moore EH. Technical aspects of needle aspiration lung biopsy: a personal perspective. Radiology. 1998. 208:303–318.7. Tsai IC, Tsai WL, Chen MC, Chang GC, Tzeng WS, Chan SW, et al. CT-guided core biopsy of lung lesions: a primer. AJR Am J Roentgenol. 2009. 193:1228–1235.8. Kinoshita F, Kato T, Sugiura K, Nishimura M, Kinoshita T, Hashimoto M, et al. CT-guided transthoracic needle biopsy using a puncture site-down positioning technique. AJR Am J Roentgenol. 2006. 187:926–932.9. Wallace AB, Suh RD. Percutaneous transthoracic nnedle biopsy:special considerations and techniques used in lung transplant recipients. Semin Intervent Radiol. 2004. 21:247–258.10. Cox JE, Chiles C, McManus CM, Aquino SL, Choplin RH. Transthoracic needle aspiration biopsy: variables that affect risk of pneumothorax. Radiology. 1999. 212:165–168.11. Yamagami T, Kato T, Iida S, Hirota T, Nishimura T. Percutaneous needle biopsy for small lung nodules beneath the rib under CT scan fluoroscopic guidance with gantry tilt. Chest. 2004. 126:744–747.12. Paulson EK, Sheafor DH, Enterline DS, McAdams HP, Yoshizumi TT. CT fluoroscopy-guided interventional procedures: techniques and radiation dose to radiologists. Radiology. 2001. 220:161–167.13. Kim GR, Hur J, Lee SM, Lee HJ, Hong YJ, Nam JE, et al. CT fluoroscopy-guided lung biopsy versus conventional CT-guided lung biopsy: a prospective controlled study to assess radiation doses and diagnostic performance. Eur Radiol. 2011. 21:232–239.14. Bandoh S, Fujita J, Fukunaga Y, Yokota K, Ueda Y, Okada H, et al. Cavitary lung cancer with an aspergilloma-like shadow. Lung Cancer. 1999. 26:195–198.15. Collings CL, Westcott JL, Banson NL, Lange RC. Pneumothorax and dependent versus nondependent patient position after needle biopsy of the lung. Radiology. 1999. 210:59–64.16. Wu CC, Maher MM, Shepard JA. Complications of CT-guided percutaneous needle biopsy of the chest: prevention and management. AJR. 2011. 196:W678–W682.17. Hare SS, Gupta A, Goncalves AT, Souza CA, Matzinger F, Seely JM. Systemic arterial air embolism after percutaneous lung biopsy. Clin Radiol. 2011. 66:589–596.18. Oertel MF, Korinth MC, Reinges MH, Krings T, Terbeck S, Gilsbach JM. Pathogenesis, diagnosis and management of pneumorrhachis. Eur Spine J. 2006. 15:Suppl 5. 636–643.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Painful Percutaneous Transthoracic Needle Biopsy of Schwannoma: A Case Report
- CT-Guided Percutaneous Automated Gun Biopsy of Pulmonary Lesions: Complications and Diagnostic Accuracy
- Analysis of the result and merit of computed tomography guided percutaneous needle aspiration biopsy of focal lung lesion
- Usefulness of Computed Tomography Guided Percutaneous Fine Needle Aspiration Lung Biopsy
- Usefulness of Automated Biopsy Guns in Image-guided Biopsy