Clin Orthop Surg.
2009 Mar;1(1):34-39. 10.4055/cios.2009.1.1.34.
Inter- and Intra-observer Reliability of MRI for Lumbar Lateral Disc Herniation
- Affiliations
-
- 1Department of Orthopaedic Surgery, Seoul National University College of Medicine, Seoul, Korea. ortho@hananet.net
- 2Department of Orthopaedic Surgery, Ulsan University College of Medicine, Seoul, Korea.
- KMID: 1127912
- DOI: http://doi.org/10.4055/cios.2009.1.1.34
Abstract
-
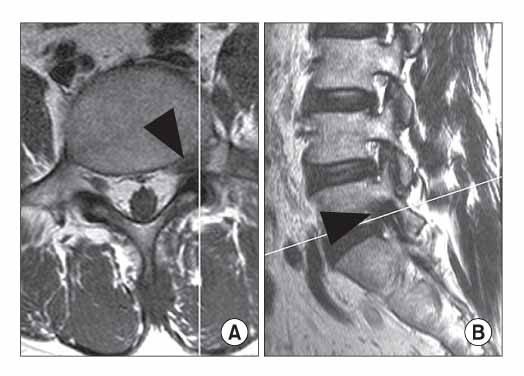
BACKGROUND: The authors analyzed inter- and intra-observer agreement with respect to interpretation of simple magnetic resonance T1- and T2-weighted axial and sagittal images for the diagnosis of lumbar lateral disc herniation, including foraminal and extraforaminal disc herniations.
METHODS
Forty-two patients in whom lumbar lateral disc herniation was suspected or confirmed by simple magnetic resonance imaging at one institute between May 2003 and December 2004 were included. The magnetic resonance images consisting of T1- and T2-weighted axial and sagittal images, and these were reviewed blindly and independently by three orthopaedic spine surgeons in a random manner. The images were interpreted as positive or negative for lateral disc herniation on 2 different occasions 3 months apart. Results were analyzed using Cohen's kappa statistic, and strengths of agreements were determined using the Landis and Koch criteria.
RESULTS
The kappa values for inter-observer agreement averaged 0.234 (0.282, 0.111, and 0.308 respectively) on the first occasion, and 0.166 (0.249, 0.111, and 0.137 respectively) on the second occasion, with an overall mean value of 0.200. Thus, the strength of agreement was only slight-to-fair according to the Landis and Koch criteria. Kappa values for intra-observer agreement averaged 0.479 (0.488, 0.491, and 0.459 respectively), indicating moderate agreement.
CONCLUSIONS
The present study indicates that simple magnetic resonance imaging is not a reliable imaging modality for diagnosing lumbar lateral disc herniation. Another imaging study with improved diagnostic values should be developed to diagnose this pathologic finding.
Keyword
MeSH Terms
Figure
Reference
-
1. Maroon JC, Kopitnik TA, Schulhof LA, Abla A, Wilberger JE. Diagnosis and microsurgical approach to far-lateral disc herniation in the lumbar spine. J Neurosurg. 1990. 72(3):378–382.
Article2. Schlesinger SM, Fankhauser H, de Tribolet N. Microsurgical anatomy and operative technique for extreme lateral lumbar disc herniations. Acta Neurochir (Wien). 1992. 118(3-4):117–129.
Article3. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977. 33(1):159–174.
Article4. Abdullah AF, Ditto EW 3rd, Byrd EB, Williams R. Extremelateral lumbar disc herniations Clinical syndrome and special problems of diagnosis. J Neurosurg. 1974. 41(2):229–234.5. Kornberg M. Extreme lateral lumbar disc herniations. Clinical syndrome and computed tomography recognition. Spine. 1987. 12(6):586–589.6. O'Hara LJ, Marshall RW. Far lateral lumbar disc herniation. The key to the intertransverse approach. J Bone Joint Surg Br. 1997. 79(6):943–947.7. Osborn AG, Hood RS, Sherry RG, Smoker WR, Harnsberger HR. CT/MR spectrum of far lateral and anterior lumbosacral disk herniations. AJNR Am J Neuroradiol. 1988. 9(4):775–778.8. Williams AL, Haughton VM, Daniels DL, Thornton RS. CT recognition of lateral lumbar disk herniation. AJR Am J Roentgenol. 1982. 139(2):345–347.
Article9. Segnarbieux F, Van de Kelft E, Candon E, Bitoun J, Frèrebeau P. Disco-computed tomography in extraforaminal and foraminal lumbar disc herniation: influence on surgical approaches. Neurosurgery. 1994. 34(4):643–647.
Article10. Angtuaco EJ, Holder JC, Boop WC, Binet EF. Computed tomographic discography in the evaluation of extreme lateral disc herniation. Neurosurgery. 1984. 14(3):350–351.
Article11. Jackson RP, Glah JJ. Foraminal and extraforaminal lumbar disc herniation: diagnosis and treatment. Spine. 1987. 12(6):577–585.
Article12. Park SK, Yeom JS, Lee CK, et al. Diagnosis of lumbar lateral disc herniation: value of magnetic resonance imaging revisited. J Korean Soc Spine Surg. 2005. 12(1):28–38.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Evaluating Paraspinal Back Muscles Using Computed Tomography (CT) and Magnetic Resonance Imaging (MRI): Reliability Analysis and Correlation with Intervertebral Disc Pathology
- A Case of Cervical Far Lateral Disc Herniation-Case Report-
- Inter-observer and intra-observer reliability between manual segmentation and semi-automated segmentation for carotid vessel wall volume measurements on three-dimensional ultrasonography
- Reliability of MRI findings for Symptomatic Extraforaminal Disc Herniation in Lumbar Spine
- Inter- and Intra-observer Variability of a Cervical OPLL Classification Using Reconstructed CT Images