J Korean Med Sci.
2007 Aug;22(4):735-739. 10.3346/jkms.2007.22.4.735.
Inflammatory Myofibroblastic Tumor on Intercostal Nerve Presenting as Paraneoplastic Pemphigus with Fatal Pulmonary Involvement
- Affiliations
-
- 1Department of Neurosurgery, School of Medicine, Kyungpook National University, Daegu, Korea. sobotta@dreamwiz.com
- KMID: 1127097
- DOI: http://doi.org/10.3346/jkms.2007.22.4.735
Abstract
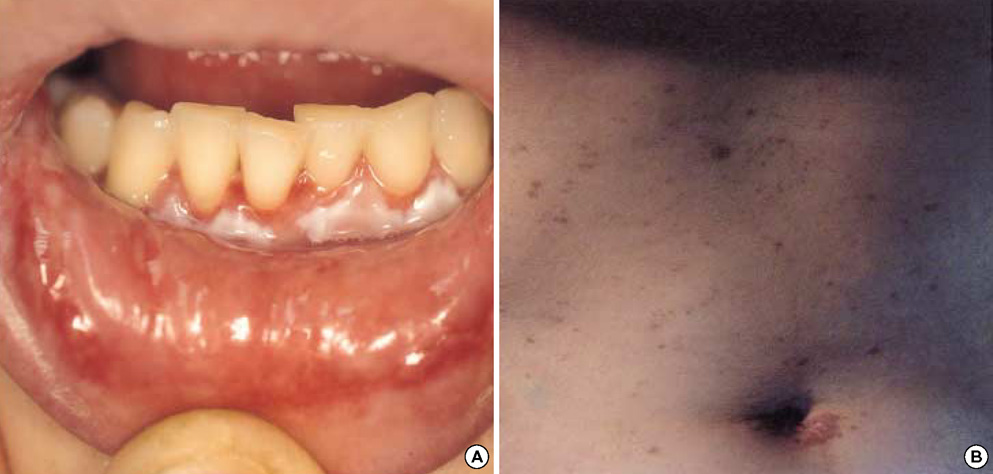
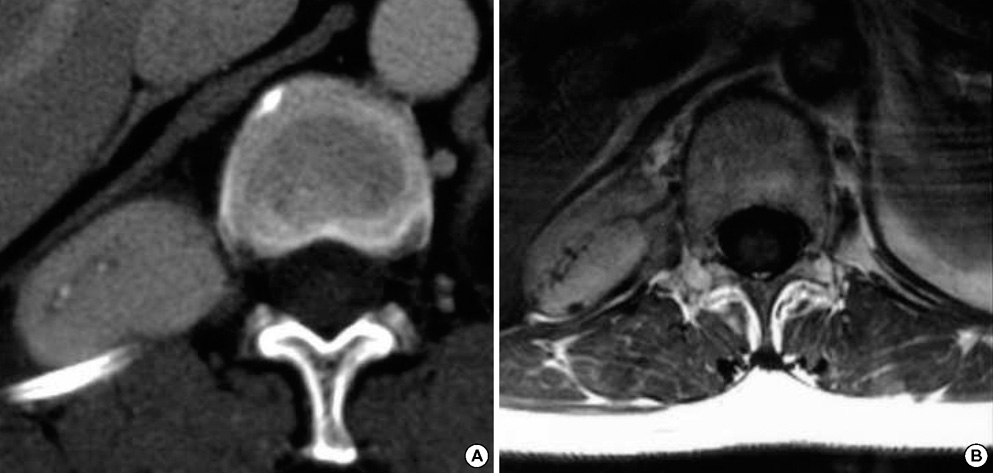
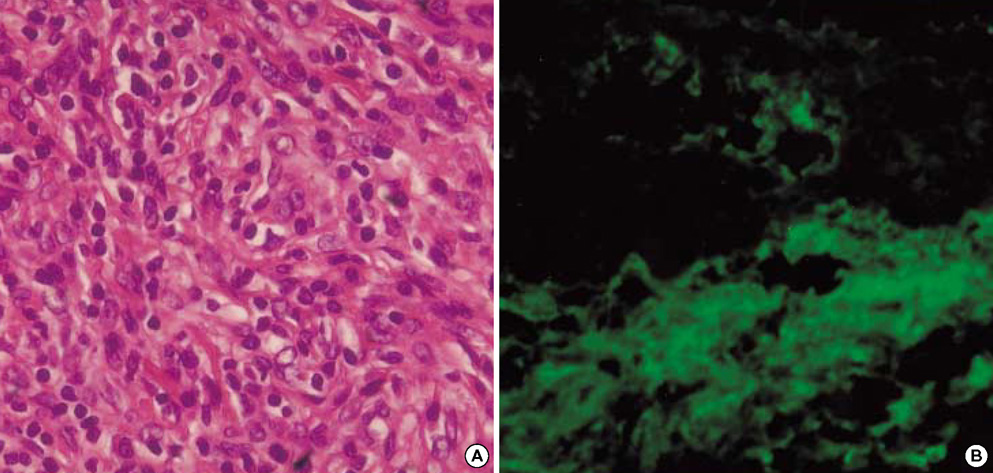
- Inflammatory myofibroblastic tumors (IMTs) are benign neoplasms that can occur at different anatomic sites with nonspecific clinical symptoms. A 48-yr-old woman presented with a 2-month history of a relapsed oral ulcer, progressive dyspnea, and a thoracic pain induced by breathing. A tumorous mass was noticed in the right costodiaphragmatic recess on chest computed tomography and magnetic resonance imaging, and the patient underwent a right costotransversectomy with excision of the tumor, which originated from the 12th intercostal nerve. Histology and immunohistochemistry showed that the tumor was an IMT of the intercostal nerve. The patient's postoperative course was not favorable; dyspnea persisted after surgery, and a progressive pulmonary compromise developed. The cause of the respiratory failure was found to be bronchiolitis obliterans, which in this case proved to be a fatal complication of paraneoplastic pemphigus associated with an IMT. This case of IMT of the spinal nerve in the paravertebral region is unique in terms of its location and presentation in combination with paraneoplastic pemphigus, which is rare. A brief review of the heterogeneous theories concerning the pathogenesis, clinicopathological features, and differential diagnosis of this disease entity is presented.
MeSH Terms
-
Diagnosis, Differential
Fatal Outcome
Female
Granuloma, Plasma Cell/complications/*pathology
Humans
Intercostal Nerves/*pathology
Lung Diseases/etiology/pathology
Middle Aged
Paraneoplastic Syndromes/etiology/*pathology
Pemphigus/etiology/*pathology
Peripheral Nervous System Neoplasms/complications/*pathology
Figure
Reference
-
1. Narla LD, Newman B, Spottswood SS, Narla S, Kolli R. Inflammatory pseudotumor. Radiographics. 2003. 23:719–729.
Article2. Anthony PP. Inflammatory pseudotumour (plasma cell granuloma) of lung, liver and other organs. Histopathology. 1993. 23:501–503.
Article3. Dehner LP. The enigmatic inflammatory pseudotumors: the current state of our understanding, or misunderstanding (editorial). J Pathol. 2000. 192:277–279.4. Despeyroux-Ewers M, Catalaa I, Collin L, Cognard C, Loubes-Lacroix F, Manelfe C. Inflammatory myofibroblastic tumour of the spinal cord: case report and review of the literature. Neuroradiology. 2003. 45:812–817.
Article5. Kim YO, Cho YJ, Ahn SK, Hwang JH, Ahn MS, Choi YH. Inflammatory pseudotumor of the thoracic spinal cord meninges: A case report. J Korean Neurosurg Soc. 1998. 27:1419–1423.6. Perez-Lopez C, Gutierrez M, Isla A. Inflammatory pseudotumor of the median nerve: case report and review of the literature. J Neurosurg. 2001. 95:124–128.7. Weiland TL, Scheithauer BW, Rock MG, Sargent JM. Inflammatory pseudotumor of nerve. Am J Surg Pathol. 1996. 20:1212–1218.
Article8. Mountney J, Suvarna SK, Brown PW, Thorpe JA. Inflammatory pseudotumour of the lung mimicking thymoma. Eur J Cardiothorac Surg. 1997. 12:801–803.
Article9. Maves CK, Johnson JF, Bove K, Malott RL. Gastric inflammatory pseudotumor in children. Radiology. 1989. 173:381–383.
Article10. Sanders BM, West KW, Gingalewski C, Engum S, Davis M, Grosfeld JL. Inflammatory pseudotumor of the alimentary tract: clinical and surgical experience. J Pediatr Surg. 2001. 36:169–173.
Article11. Hytiroglou P, Brandwein MS, Stauchen JA, Mirante JP, Urken ML, Biller HF. Inflammatory pseudotumor of the parapharyngeal space: case report and review of the literature. Head Neck. 1992. 14:230–234.
Article12. Coffin CM, Watterson J, Priest JR, Dechner LP. Extrapulmonary inflammatory myofibroblastic tumor (inflammatory pseudotumor): a clinicopathologic and immunohistochemical study of 84 cases. Am J Surg Pathol. 1995. 19:859–872.
Article13. Jenkins PC, Dickison AE, Flanagan MF. Cardiac inflammatory pseudotumor: rapid appearance in an infant with congenital heart disease. Pediatr Cardiol. 1996. 17:399–401.
Article14. Martin CJ. Orbital pseudotumor: case report and overview. J Am Optom Assoc. 1997. 68:775–781.15. Rose AG, McCormick S, Cooper K, Titus JL. Inflammatory pseudotumor (plasma cell granuloma) of the heart. Arch Pathol Lab Med. 1996. 120:549–554.16. Scott L, Blair G, Taylor G, Dimmick J, Fraser G. Inflammatory pseudotumors in children. J Pediatr Surg. 1988. 23:755–758.
Article17. Maier HC, Sommers SC. Recurrent and metastatic pulmonary fibrous histiocytoma/plasma cell granuloma in a child. Cancer. 1987. 60:1073–1076.
Article18. Pearson PJ, Smithson WA, Driscoll DJ, Banks PM, Ehman RL. Inoperable plasma cell granuloma of the heart: spontaneous decrease in size during an 11-month period. Mayo Clin Proc. 1998. 63:1022–1025.
Article19. Mar WA, Glaesser R, Struble K, Stephens-Groff S, Bangert J, Hansen RC. Paraneoplastic pemphigus with bronchiolitis obliterans in a child. Pediatr Dermatol. 2003. 20:238–242.
Article20. Takahashi M, Shimatsu Y, Kazama T, Kimura K, Otsuka T, Hashimoto T. paraneoplastic pemphigus associated with bronchiolitis obliterans. Chest. 2000. 117:603–607.
Article21. Anhalt GJ, Kim SC, Stanley JR, Korman NJ, Jabs DA, Kory M. Paraneoplastic pemphigus. An autoimmune mucocutaneous disease associated with neoplasia. N Engl J Med. 1990. 323:1729–1735.
Article22. Camisa C, Helm TN. Paraneoplastic pemphigus is a distinct neoplasia-induced autoimmune disease. Arch Dermatol. 1993. 129:883–886.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Paraneoplastic Pemphigus as a Preceding Manifestation of Underlying Follicular Lymphoma Treated with R-CHOP
- Inflammatory Myofibroblastic Tumor of Nasal Septum after Septoplasty: A Case Report
- Inflammatory Myofibroblastic Tumor of the Nasal Cavity
- Inflammatory Myofibroblastic Tumor (InflammatoryFibrosarcoma) of the Lung: A Case Report
- Inflammatory Myofibroblastic Tumor of Kidney