J Korean Med Sci.
2011 Nov;26(11):1522-1526. 10.3346/jkms.2011.26.11.1522.
Early Non-Invasive Diagnosis and Treatment of Acute Eosinophlic Myopericarditis by Cardiac Magnetic Resonance
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. elisabet.chang@gmail.com
- 2Department of Radiology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 3Cardiovascular Imaging Center, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 1123457
- DOI: http://doi.org/10.3346/jkms.2011.26.11.1522
Abstract
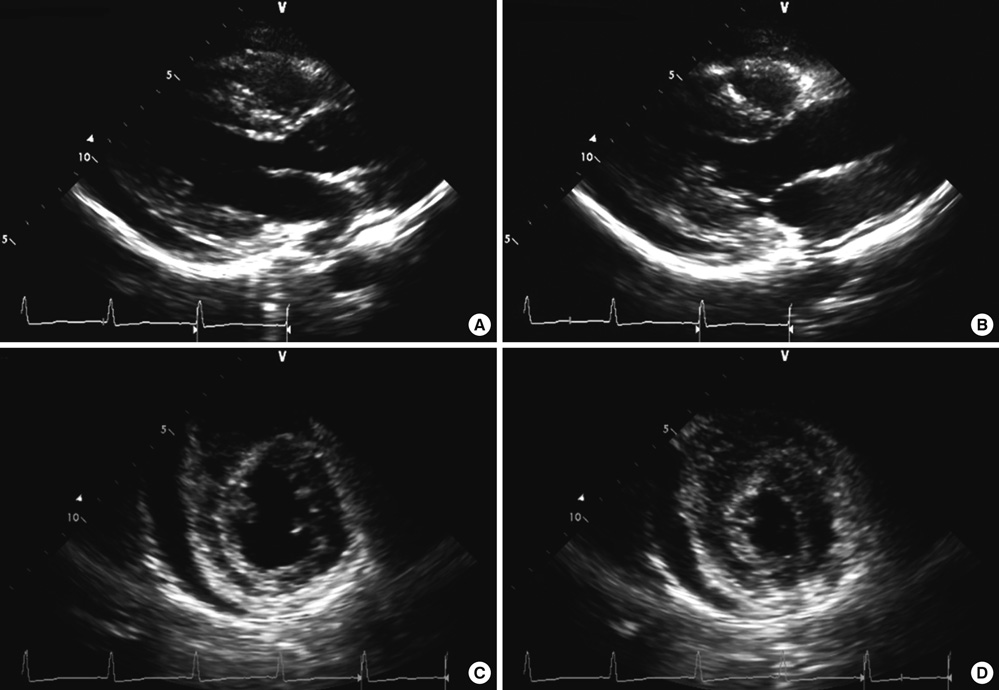
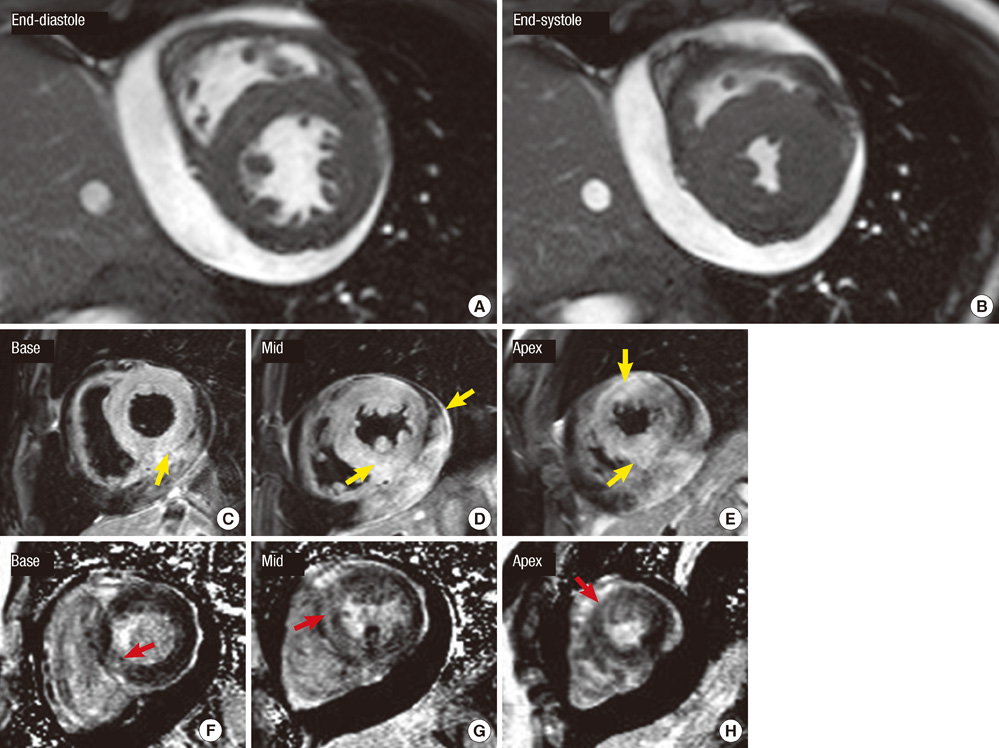
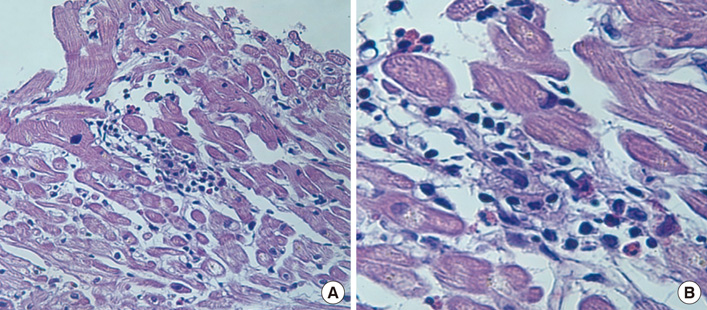
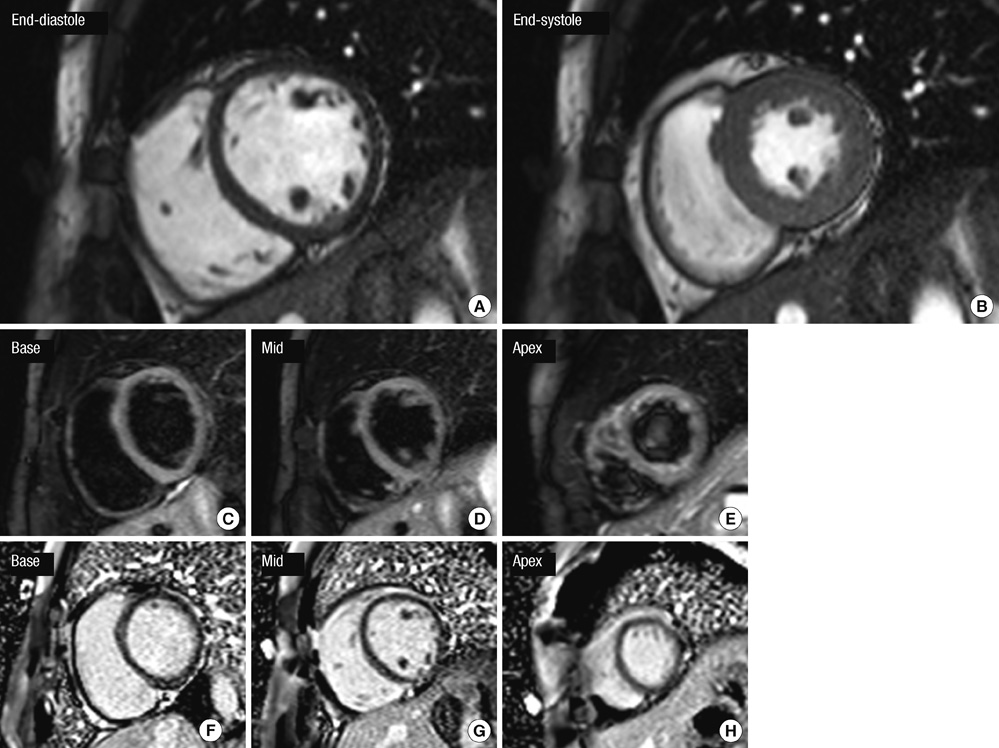
- We report a case of early non-invasive diagnosis of acute eosinophilic myopericarditis (AEM) by cardiovascular magnetic resonance (CMR) before cardiac biopsy. A 35-yr-old woman presented with a flu-like illness, followed by pleuritic chest pain and shortness of breath. Transthoracic echocardiography revealed mild left ventricular (LV) systolic dysfunction with borderline LV wall thickness and moderate pericardial effusion. The patient had peripheral eosinophilia and CMR was performed immediately at first day of visit before cardiac biopsy. CMR showed diffuse subepicardial high T2 signals and diffuse late gadolinium enhancement in LV. Steroid therapy was immediately initiated and patient's symptom was rapidly improved. Endomyocardial biopsy at hospital day 3 reported multifocal mild infiltration of eosinophils and lymphocytes. The patient was finally confirmed as acute eosinophilic myopericarditis. This presentation emphasizes on the role of CMR which enables early non-invasive diagnosis of AEM and visualize the extent of the myocarditis.
Keyword
MeSH Terms
Figure
Reference
-
1. Al Ali AM, Straatman LP, Allard MF, Ignaszewski AP. Eosinophilic myocarditis: case series and review of literature. Can J Cardiol. 2006. 22:1233–1237.2. Sohn IS, Park JC, Chung JH, Kim KH, Ahn Y, Jeong MH, Cho JG. A case of acute eosinophilic myopericarditis presenting with cardiogenic shock and normal peripheral eosinophil count. Korean J Intern Med. 2006. 21:136–140.3. Burke AP, Saenger J, Mullick F, Virmani R. Hypersensitivity myocarditis. Arch Pathol Lab Med. 1991. 115:764–769.4. Debl K, Djavidani B, Buchner S, Poschenrieder F, Heinicke N, Feuerbach S, Riegger G, Luchner A. Time course of eosinophilic myocarditis visualized by CMR. J Cardiovasc Magn Reson. 2008. 10:21.5. Abdel-Aty H, Boyé P, Zagrosek A, Wassmuth R, Kumar A, Messroghli D, Bock P, Dietz R, Friedrich MG, Schulz-Menger J. Diagnostic performance of cardiovascular magnetic resonance in patients with suspected acute myocarditis: comparison of different approaches. J Am Coll Cardiol. 2005. 45:1815–1822.6. Gagliardi MG, Bevilacqua M, Di Renzi P, Picardo S, Passariello R, Marcelletti C. Usefulness of magnetic resonance imaging for diagnosis of acute myocarditis in infants and children, and comparison with endomyocardial biopsy. Am J Cardiol. 1991. 68:1089–1091.7. Mahrholdt H, Wagner A, Judd RM, Sechtem U, Kim RJ. Delayed enhancement cardiovascular magnetic resonance assessment of non-ischaemic cardiomyopathies. Eur Heart J. 2005. 26:1461–1474.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Infectious Mononucleosis Complicated by Myopericarditis
- A Case of Acute Myopericarditis with Localized ST Elevation Mimicking Myocardial Infarction
- A Case of Acute Myopericarditis Associated with Mycoplasma pneumoniae Infection in a Korean Adult
- Acute Viral Myopericarditis Presenting as a Transient Effusive-Constrictive Pericarditis Caused by Coinfection with Coxsackieviruses A4 and B3
- A Rare Presentation of Probable Training-Related Chronic Myopericarditis in an Endurance Cyclist: A Case Report