Korean J Ophthalmol.
2004 Jun;18(1):70-78. 10.3341/kjo.2004.18.1.70.
Clinical Features of Ocular Trauma in Emergency Department
- Affiliations
-
- 1Department of Ophthalmology, College of Medicine, Pusan National University, Pusan, Korea.
- KMID: 1115787
- DOI: http://doi.org/10.3341/kjo.2004.18.1.70
Abstract
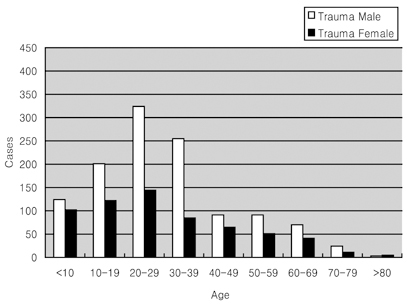
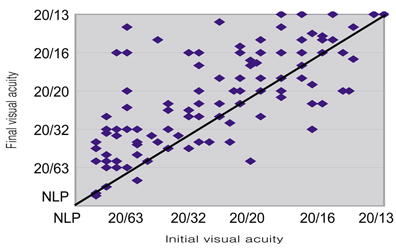
- This study analyzed a hospital-based study to investigate the incidence and clinical features of ocular traumatic emergencies in Korea. Over a 6-year period, 1809 patients with ocular traumatic emergency each individually underwent clinical study including subject characteristics, type of ocular emergency, disease severity, etiology of ocular trauma, injury location, cause of decreased visual acuity, management of ocular injury, and final visual acuity. The homogeneity of each finding of the clinical features of ocular traumatic emergency was tested by an X2 test at a 95% level of certainty. During follow-up periods ranging from 3 days to 23 months (mean 2.0 months), the 1809 patients with ocular traumatic emergency, 1183 males (65.4%) and 626 females (34.6%), were studied. The incidence of ocular emergencies peaked in the third decade of life, irrespective of gender (P< 0.05). Corneal abrasion was the most common etiology among 1, 552 (85.8%) closed injuries, and corneal laceration among 257 (14.2%) open injuries (P< 0.05). There were 542 cases (30%) of severe ocular injury, such as penetrating ocular injury, blow out fracture, and intraocular foreign body (IOF), and 1267 (70%) of less severe ocular injury, such as superficial ocular injury or contusion. The most common etiology of severe ocular injury was penetrating ocular injury, and that of less severe injury was corneal injury (P< 0.05). The main causative activity of ocular injuries was work in 631 cases (34.9%), assault in 398 (22.0%), play in 278 (15.4%), traffic accidents in 145 (8.0%) and sports in 128 (7.1%). Five hundred and fifty-four cases (32.5%) underwent surgical intervention. There was an improvement of visual acuity in 502 cases (70.1%), no change in 122 (17.0%), and worsening in 92 (12.9%). We suggest that preventive educational measures be instigated at workplaces to reduce the incidence of ocular traumatic emergency, especially severe ocular injury.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Comparison of Clinical Appearance of Pediatric Ocular Injury, According to Grade Level
Hyoung Sub Shim, Su Jeong Song, Chul Young Choi, Joon Mo Kim, Hae Ran Chang
J Korean Ophthalmol Soc. 2008;49(1):148-157. doi: 10.3341/jkos.2008.49.1.148.
Reference
-
1. Kuhn F, Morris R. A standardized classification of ocular trauma. Graefe's Arch Clin Exp Ophthalmol. 1996. 614:399–403.2. Canavan YM, O'Flaherty MJ, Archer DB, Elwood JH. A 10 year survey of injuries in northern Ireland 1967-76. Br J Ophthalmol. 1980. 64:618–625.3. Klopfer J, Tielsch JM. Ocular trauma in the United States Eye injuries resulting in hospitalization, 1984 through 1987. Arch Ophthalmol. 1992. 110:838–842.4. Tielsch JM, Parver L, Shankar B. Time trends in the incidence of hospitalized ocular trauma. Arch Ophthalmol. 1989. 107:519–523.5. Karlson TA, Klein BEK. The incidence of acute hospital-treated eye injuries. Arch Ophthalmol. 1986. 104:1473–1476.6. Tsai CC, Kau HC, Kao SC, Liu JH. A review of ocular emergencies in a Taiwanese medical center. Chung Hua I Hsueh Tsa Chih. 1998. 61:414–420.7. Morris RE, Witherspoon CD, Helms HA Jr, Feist RM, Byrne JB Jr. Eye injury registry of Alabama (preliminary report): Demographics and prognosis of severe eye injury. South Med J. 1987. 80:810–816.8. Thoradson U, Ragnarsson AT, Gudbrandsson B. Ocular trauma: Observation in 105 patients. Acta Ophthalmol. 1978. 57:922–928.9. Maltzman BA, Pruzon H, Mund ML. A survey of ocular trauma. Surv Ophthalmol. 1976. 2:285–290.10. Lee KJ, Oh JH. A statistical observation of the ocular injuries. J Korean Ophthalmol Soc. 1990. 31:229–239.11. Kim SS, Yoo JM. A clinical study of industrial ocular injuries. J Korean Ophthalmol Soc. 1988. 29:393–403.12. Patel BC, Morgan H. Work-related penetrating eye injuries. Acta Ophthalmol. 1991. 69:377–381.13. Chang Y, Oh S, Chi NC. A clinical observation of ocular injuries of inpatients. J Korean Ophthalmol Soc. 1993. 34:257–263.14. Nash EA, Margo CE. Patterns of emergency department visits for disorders of the eye and ocular adnexa. Arch Ophthalmol. 1998. 116:1222–1226.15. Dannenberg AL, Parver LM, Brechner RJ, Khoo L. Penetrating injuries in the workplace. Arch Ophthalmol. 1992. 110:843–849.16. Voon LW, See J, Wong TY. The epidemiology of ocular trauma in Singapore: perspective from the emergency service of a large tertiary hospital. Eye. 2001. 15:75–81.17. Desai P, MacEwen CJ, Baines P, Minassian DC. Incidence of cases of ocular trauma admitted to hospital and incidence of blinding outcome. Br J Ophthalmol. 1996. 80:592–596.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Clinical Features of Geriatric Ocular Trauma in a Regional Emergency Medical Center
- Clinical survey of the Ocular Trauma Patients visited Emergency Department
- Clinical Analysis of Ocular Trauma Induced by Lawn Trimmers
- The Changes in the Clinical Features of Pediatric Ocular Trauma
- Association of Alcohol Consumption with the Risk of Ocular Trauma