Korean J Ophthalmol.
2009 Sep;23(3):153-158. 10.3341/kjo.2009.23.3.153.
Comparison of Photocoagulation With Combined Intravitreal Triamcinolone for Diabetic Macular Edema
- Affiliations
-
- 1Department of Ophthalmology, Eulji General Hospital, Eulji University School of Medicine, Seoul, Korea. pjs4106@eulji.ac.kr
- KMID: 1115745
- DOI: http://doi.org/10.3341/kjo.2009.23.3.153
Abstract
- PURPOSE
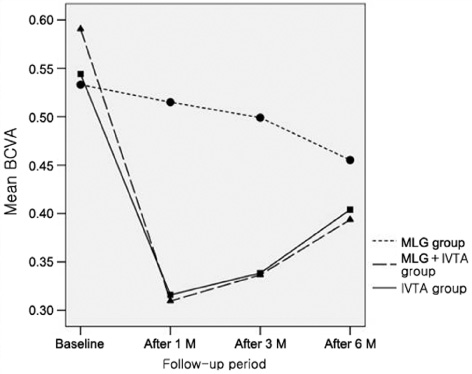
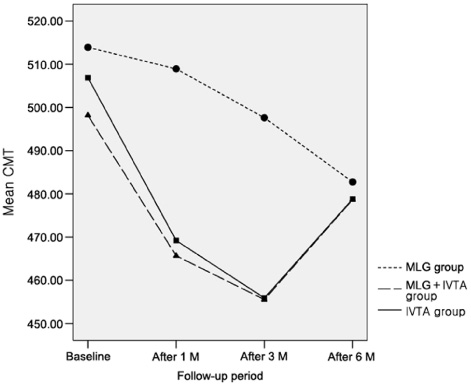
To compare the efficacy between macular laser grid (MLG) photocoagulation and MLG plus intravitreal triamcinolone acetonide (IVTA; MLG+IVTA) therapy in diabetic macular edema (DME) patients. METHODS: A prospective, randomized, clinical trial was conducted of DME patients. A total of 60 eyes (54 patients) affected by DME were observed for a minimum of 6 months. Thirty eyes of 28 patients who received MLG treatment and 30 eyes of 26 patients who received the combined MLG+IVTA treatment were included in the study. Main outcome measures were BCVA and central macular thickness (CMT) as measured by optical coherence tomography (OCT) at 1, 3, and 6 months after treatment. Additionally, the authors examined retrospectively 20 eyes of 20 patients who were treated with only IVTA and compared with the 2 groups (MLG group and MLG+IVTA group). RESULTS: Baseline BCVA was 0.53+/-0.32 and CMT was 513.9+/-55.1 microm in the MLG group. At 1 and 3 months after treatment, the MLG group showed no significant improvement of BCVA and CMT, although there was significant improvement after 6 months. In the MLG+IVTA group, the baseline BCVA was 0.59+/-0.29 and CMT was 498.2+/-19.8 microm. After treatment, significant improvement of BCVA and CMT was observed at all follow-up time periods. When comparing the MLG group with the MLG+IVTA group, the latter had better results after 1 and 3 months, although at 6 months, there was no significant difference of BCVA and CMT between the 2 groups. Additionally, the IVTA group showed more improvement than the MLG group at 1 and 3 months but showed no significant difference at 6 months. In addition, the IVTA group showed no significant difference with the MLG+IVTA group at all follow-up time periods. CONCLUSIONS: For DME patients, the combined MLG+IVTA treatment had a better therapeutic effect than the MLG treatment for improving BCVA and CMT at the early follow-up time periods. IVTA treatment alone could be an additional alternative therapeutic option to combined therapy.
Keyword
MeSH Terms
-
Aged
Diabetic Retinopathy/*drug therapy/pathology/physiopathology/*surgery
Follow-Up Studies
Glucocorticoids/*administration & dosage
Humans
Injections
*Laser Coagulation
Macular Edema/*drug therapy/pathology/physiopathology/*surgery
Middle Aged
Postoperative Period
Tomography, Optical Coherence
Triamcinolone Acetonide/*administration & dosage
Visual Acuity
Vitreous Body
Figure
Cited by 1 articles
-
Prevention and management of diabetic retinopathy
Ji Hun Song
J Korean Med Assoc. 2014;57(6):525-534. doi: 10.5124/jkma.2014.57.6.525.
Reference
-
1. Ryan Stephen J.. Chew Emily Y., Ferris Fredrick L., editors. Nonproliferative diabetic retinopathy. Retina. 2006. v. 2:4th ed. New York: Mosby, Elsevier Inc.;chap. 67.2. Early Treatment Diabetic Retinopathy Study Research Group. Photocoagulation for diabetic macular edema. Early Treatment Diabetic Retinopathy Study Report Number 1. Arch Ophthalmol. 1985. 103:1796–1806.3. Early Treatment Diabetic Retinopathy Study Research Group. Treatment techniques and clinical guidelines for photocoagulation of diabetic macular edema. Early Treatment Diabetic Retinopathy Study Report Number 2. Ophthalmology. 1987. 94:761–774.4. Early Treatment Diabetic Retinopathy Study Research Group. Focal photocoagulation treatment of diabetic macular edema. Relationship of treatment effect to fluorescein angiographic and other retinal characteristics at baseline: ETDRS report no. 19. Arch Ophthalmol. 1995. 113:1144–1155.5. Martidis A, Duker JS, Greenberg PB, et al. Intravitreal triamcinolone for refractory diabetic macular edema. Ophthalmology. 2002. 109:920–927.6. Jonas JB, Kreissig I, Sofker A, Degenring RF. Intravitreal injection of triamcinolone for diffuse diabetic macular edema. Arch Ophthalmol. 2003. 121:57–61.7. Massin P, Audren F, Haouchine B, et al. Intravitreal triamcinolone acetonide for diabetic diffuse macular edema: preliminary results of a prospective controlled trial. Ophthalmology. 2004. 111:218–224. discussion 224-5.8. Jonas JB, Akkoyun I, Kreissig I, Degenring RF. Diffuse diabetic macular oedema treated by intravitreal triamcinolone acetonide: a comparative, non-randomised study. Br J Ophthalmol. 2005. 89:321–326.9. Ozkiris A, Evereklioglu C, Erkilic K, et al. Intravitreal triamcinolone acetonide injection as primary treatment for diabetic macular edema. Eur J Ophthalmol. 2004. 14:543–549.10. Sutter FK, Simpson JM, Gillies MC. Intravitreal triamcinolone for diabetic macular edema that persists after laser treatment: three-month efficacy and safety results of a prospective, randomized, double-masked, placebo-controlled clinical trial. Ophthalmology. 2004. 111:2044–2049.11. Micelli Ferrari T, Sborgia L, Furino C, et al. Intravitreal triamcinolone acetonide: valuation of retinal thickness changes measured by optical coherence tomography in diffuse diabetic macular edema. Eur J Ophthalmol. 2004. 14:321–324.12. Floman N, Zor U. Mechanism of steroid action in ocular inflammation: inhibition of prostaglandin production. Invest Ophthalmol Vis Sci. 1977. 16:69–73.13. Wilson CA, Berkowitz BA, Sato Y, et al. Treatment with intravitreal steroid reduces blood-retinal barrier breakdown due to retinal photocoagulation. Arch Ophthalmol. 1992. 110:1155–1159.14. Antcliff RJ, Spalton DJ, Stanford MR, et al. Intravitreal triamcinolone for uveitic cystoid macular edema: An optical coherence tomography study. Ophthalmology. 2001. 108:765–772.15. Schindler RH, Chandler D, Thresher R, Machmer R. The clearance of intravitreal triamcinolone acetonide. Am J Ophthalmol. 1982. 93:415–417.16. Beer PM, Bakri SJ, Singh RJ, et al. Intraocular concentration and pharmacokinetics of triamcinolone acetonide after a single intravitreal injection. Ophthalmology. 2003. 110:681–686.17. Choi KS, Chung JK, Lim SH. Laser photocoagulation combined with intravitreal triamcinolone acetonide injection in proliferative diabetic retinopathy with macular edema. Korean J Ophthalmol. 2007. 21:11–17.18. Jeong YC, Bae SH, Kim JW. Comparison of effects of IVTA and photocoagulation, depending on types of diabetic macular edema. J Korean Ophthalmol Soc. 2007. 48:655–664.19. Wingate RJ, Beaumont PE. Intravitreal triamcinolone and elevated intraocular pressure. Aust N Z J Ophthalmol. 1999. 27:431–432.20. Moshfeghi DM, Kaiser PK, Scott IU, et al. Acute endophthalmitis following intravitreal triamcinolone acetonide injection. Am J Ophthalmol. 2003. 136:791–796.21. Nelson ML, Tennant MT, Sivalingam A, et al. Infectious and presumed noninfectious endophthalmitis after intravitreal triamcinolone acetonide injection. Retina. 2003. 23:686–691.22. Thomas ER, Wang J, Ege E, et al. Intravitreal triamcinolone acetonide concentration after subtenon injection. Am J Ophthalmol. 2006. 142:860–861.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intravitreal Injection of Triamcinolone for Refractory Diabetic Macular Edema
- The Effect of Intravitreal Triamcinolone Acetonide Injection according to the Diabetic Macular Edema Type
- Intravitreal and Additional Posterior Subtenon Triamcinolone Injection in Diabetic Macular Edema
- Comparison of Intravitreal Bevacizumab Alone Injection and Intravitreal Combination Low-Dose Bevacizumab-Triamcinolone Injection or Diabetic Macular Edema
- Grid Laser Photocoagulation After Intravitreal Triamcinolone for Macular Edema Associated With Branch Retinal Vein Occlusion