Yonsei Med J.
2006 Apr;47(2):264-270. 10.3349/ymj.2006.47.2.264.
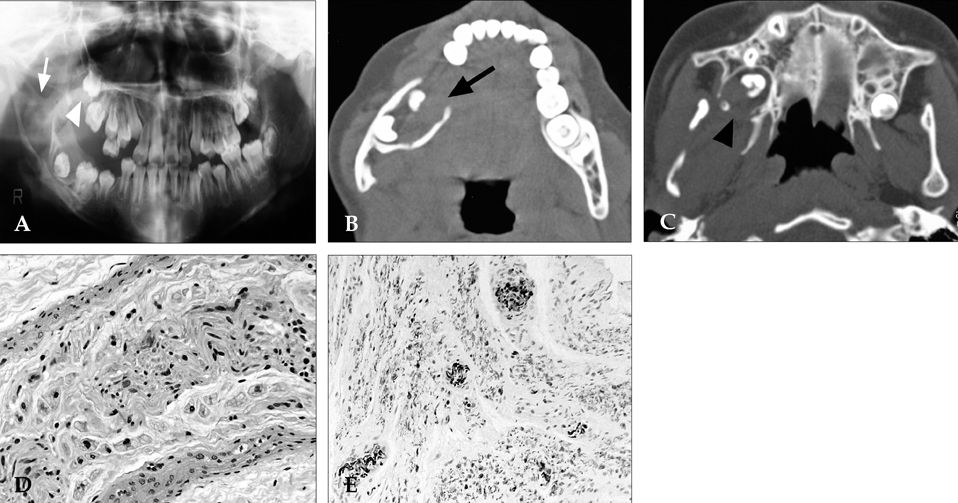
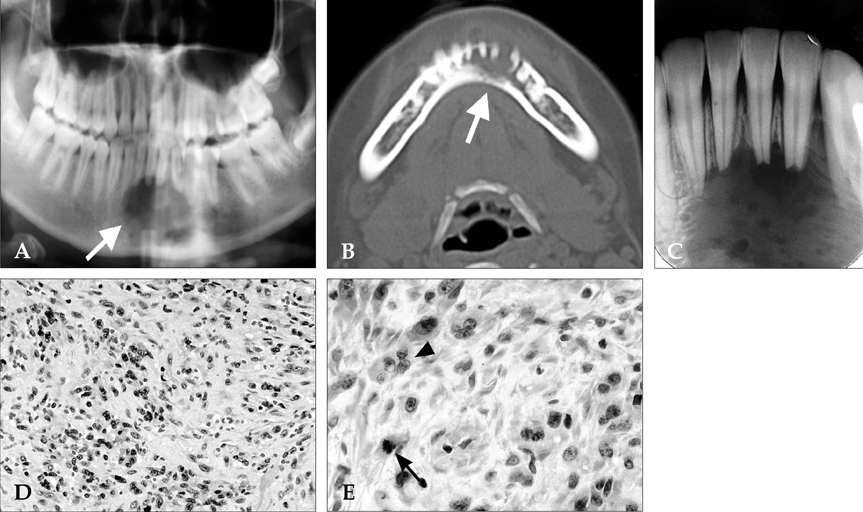
Intraosseous Nerve Sheath Tumors in the Jaws
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, College of Dentistry, Yonsei University, Seoul, Korea. sanghwy@yumc.yonsei.ac.kr
- 2Department of Oral Pathology, College of Dentistry, Yonsei University, Seoul, Korea.
- 3Oral Science Research Center, College of Dentistry, Yonsei University, Seoul, Korea.
- 4Oral Cancer Research Institute, College of Dentistry, Yonsei University, Seoul, Korea.
- 5Medical Research Center, College of Dentistry, Yonsei University, Seoul, Korea.
- KMID: 1110753
- DOI: http://doi.org/10.3349/ymj.2006.47.2.264
Abstract
- Although the head and neck region is recognized as the most common location for peripheral nerve sheath tumors, central involvement, particularly in the jaw bones, is quite unusual. Neurofibroma is one of the most common nerve sheath tumors occurring in the soft tissue and generally appears in neurofibromatosis 1 (NF1 or von Recklinghausen's disease). Malignant peripheral nerve sheath tumors (MPNSTs) are uncommon sarcomas that almost always arise in the soft tissue. Here, we report four cases of intraosseous peripheral nerve sheath tumors occurring in the jaw bones and compare the clinical, radiologic, and pathologic findings in order to make a differential diagnosis.
Keyword
MeSH Terms
Figure
Reference
-
1. Weiss L. Cell and tissue biology; A textbook of histology. 1988. 6th ed. Munchen: Urban and Schwarzenberg;233.2. Polak M, Polak G, Brocheriou C, Vigneul J. Solitary neurofibroma of the mandible: case report and review of the literature. J Oral Maxillofac Surg. 1989. 47:65–68.3. Weaver BD, Graves RW, Keyes GG, Lattanzi DA. Central neurofibroma of the mandible: report of a case. J Oral Maxillofac Surg. 1991. 49:1243–1246.4. Raghuveer HP. Solitary, central neurofibroma of the mandible: a case report. J Pierre Fauchard Acad. 1994. 8:107–109.5. Papageorge MB, Doku HC, Lis R. Solitary neurofibroma of the mandible and infratemporal fossa in a young child. Report of a case. Oral Surg Oral Med Oral Pathol. 1992. 73:407–411.6. Papadopoulos H, Zachariades N, Angelopoulos AP. Neurofibroma of the mandible. Review of the literature and report of a case. Int J Oral Surg. 1981. 10:293–297.7. Griffin JE Jr, Gray CM, Schow CE Jr. Infected central neurofibroma of the mandible. Report of a case. J Oral Med. 1983. 38:94–96.8. Langford RJ, Rippin JW. Bilateral intra-osseous neurofibromata of the mandible. Br J Oral Maxillofac Surg. 1990. 28:344–346.9. Weiss SW, Goldblum JR. Enzinger and Weiss's soft tissue tumors. 2001. 4th ed. St. Louis: Mosby;1209–1263.10. Hirose T, Scheithauer BW, Sano T. Perineural malignant peripheral nerve sheath tumors (MPNST): a clinicopathologic, immunohistochemical, and ultrastuctural study of seven cases. Am J Surg Pathol. 1998. 22:1368–1378.11. Bullock MJ, Bedard YC, Bell RS, Kandel R. Intraosseous malignant peripheral nerve sheath tumor. Report of a case and review of the literature. Arch Pathol Lab Med. 1995. 119:367–370.12. Ellis GL, Abrams AM, Melrose RJ. Intraosseous benign neural sheath neoplasms of the jaws. Report of seven new cases and review of the literature. Oral Surg Oral Med Oral Pathol. 1977. 44:731–743.13. Chung IH, Kim NH, Choi IY. Macrodactylism associated with neurofibroma of the median nerve. A case report. Yonsei Med J. 1973. 14:49–52.14. Ahn JY, Kwon SO, Shin MS, Shim JY, Kim OJ. A case of multiple schwannomas of the trigeminal nerves, acoustic nerves, lower cranial nerves, brachial plexuses and spinal canal: schwannomatosis or neurofibromatosis? Yonsei Med J. 2002. 43:109–113.15. Lorson EL, DeLong PE, Osbon DB, Dolan KD. Neurofibromatosis with central neurofibroma of the mandible: review of the literature and report of case. J Oral Surg. 1977. 35:733–738.16. Fawcett KJ, Dahlin DC. Neurilemmoma of bone. Am J Clin Pathol. 1967. 47:759–766.17. Hunt JC, Pugh DG. Skeletal lesions in neurofibromatosis. Radiology. 1961. 76:1–20.18. Vincent SD, Williams TP. Mandibular abnormalities in neurofibromatosis. Case report and literature review. Oral Surg Oral Med Oral Pathol. 1983. 55:253–258.19. Thornton JB, Tomaselli CE, Rodu B, Creath CJ. Neurofibroma of the mandible in an adolescent with von Recklinghausen's disease. Pediatr Dent. 1992. 14:347–350.20. Lee L, Yan YH, Pharoah MJ. Radiographic features of the mandible in neurofibromatosis. Oral Surg Oral Med Oral Pathol. 1996. 81:361–367.21. Gnepp DR, Keyes GG. Central neurofibromas of the mandible: report of two cases. J Oral Surg. 1981. 39:125–127.22. Prescott GH, White RE. Solitary, central neurofibroma of the mandible: report of case and review of the literature. J Oral Surg. 1970. 28:305–309.23. Ellis GL, Abrams AM, Melrose RJ. Intraosseous benign neural sheath neoplasms of the jaws. Report of seven new cases and review of the literature. Oral Surg Oral Med Oral Pathol. 1977. 44:731–743.24. Oberman HA, Sullenger G. Neurogenous tumors of the head and neck. Cancer. 1967. 20:1992–2001.25. Bullock MJ, Bedard YC, Bell RS, Kandel R. Intraosseous malignant peripheral nerve sheath tumor. Report of a case and review of the literature. Arch Pathol Lab Med. 1995. 119:367–370.26. Terry DG, Sauser DD, Gordon MD. Intraosseous malignant peripheral nerve sheath tumor in a patient with neurofibromatosis. Skeletal Radiol. 1998. 27:346–349.27. Colmenero C, Rivers T, Patron M, Sierra I, Gamallo C. Maxillofacial malignant peripheral nerve sheath tumours. J Craniomaxillofac Surg. 1991. 19:40–46.28. Dorfman HD, Czerniak B. Bone cancers. Cancer. 1995. 75:203–210.29. Bojsen-Moller M, Myrhe-Jensen O. A consecutive series of 30 malignant schwannomas: survival in relation to clinicopathological parameters and treatment. Acta Pathol Microbiol Scand. 1977. 92A:147–158.30. Weiss SW, Langloss JM, Enzinger FM. The role of S-100 protein in the diagnosis of soft tissue tumors with particular reference to benign and malignant Schwann cell tumors. Lab Invest. 1983. 49:299–308.31. Dorfman HD, Czerniak B. Bone tumors. 1998. St Louis: Mosby;839–841.32. Conley J, Janecka IP. Neurilemmoma of the head and neck. Trans Sect Otolaryngol Am Acad Opthamol Otolaryngol. 1975. 80:459–464.33. Batsakis JG. Tumors of the head and neck; clinocopathological considerations. 1979. Baltimore: Williams and Wilkins;313–323.34. Shafer WG, Hine MK, Levy BM. A textbook of oral pathology. 1983. Philadelphia: WB Saunders;206–208.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intraosseous Malignant Peripheral Nerve Sheath Tumor of Multiple Bones of the Midfoot: A Case Report
- Extracranial Nerve Sheath Tumors of the Head and Neck
- Malignant Peripheral Nerve Sheath Tumor of the Larynx
- Intraosseous Neurilemmoma of the First Lumbar Vertebra: A Case Report
- Malignant Peripheral Nerve Sheath Tumor of the Breast in a Patient without Neurofibromatosis: A Case Report