Korean J Radiol.
2005 Sep;6(3):143-152. 10.3348/kjr.2005.6.3.143.
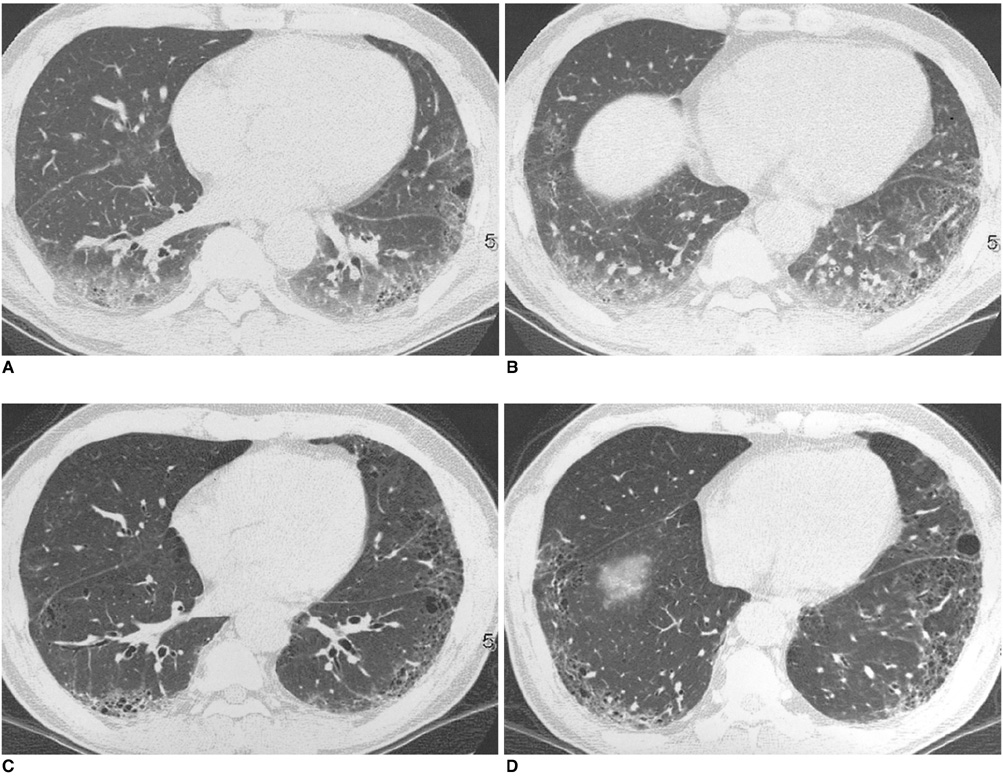
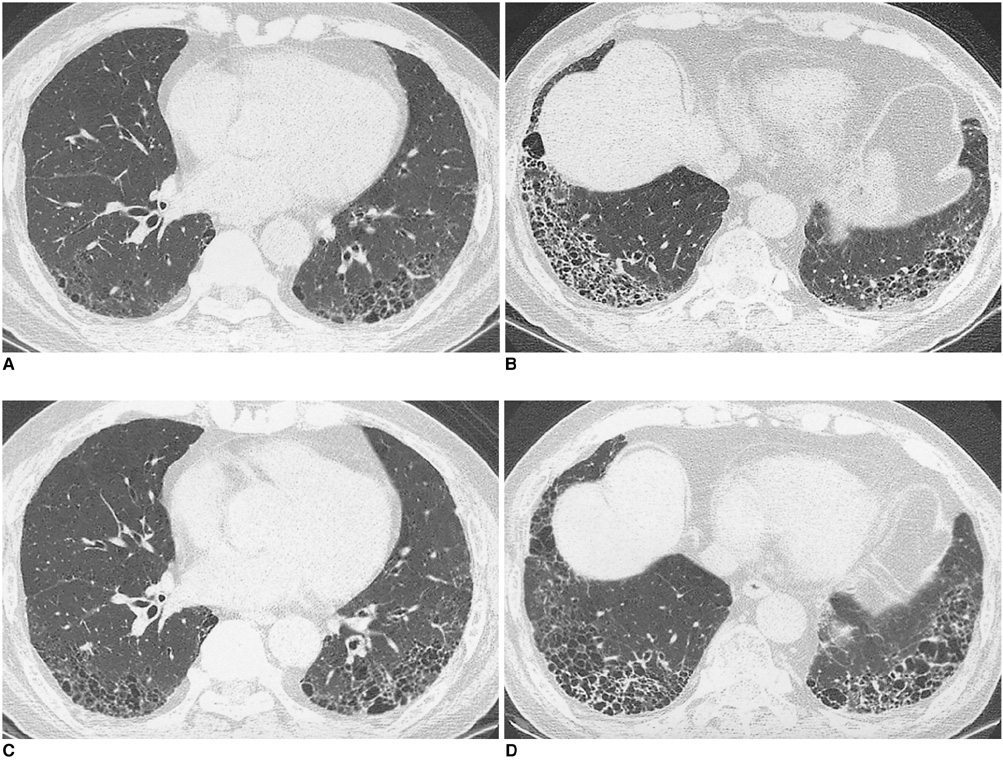
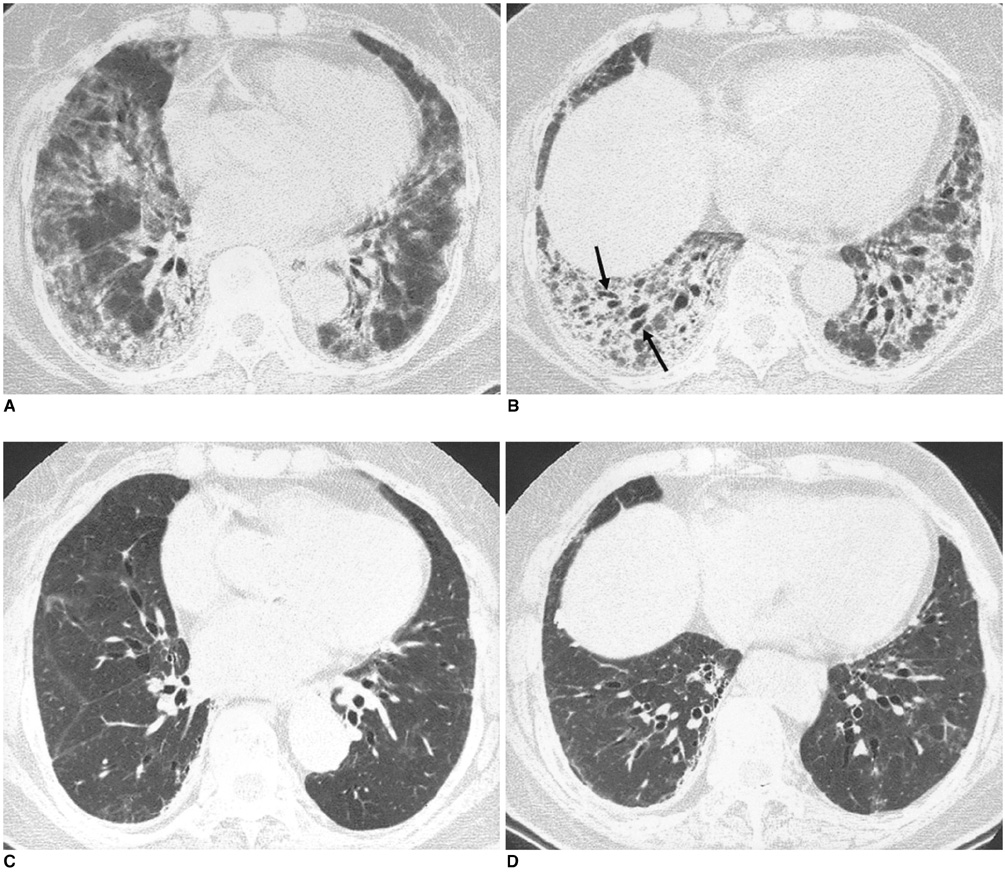
Usual Interstitial Pneumonia and Non-Specific Interstitial Pneumonia: Serial Thin-Section CT Findings Correlated with Pulmonary Function
- Affiliations
-
- 1Department of Radiology and the Center for Imaging Science, Samsung Medical Center, Sungkyunkwan University School of Medicine, Korea. kyungs.lee@samsung.com
- 2Department of Radiology, Pusan National University Hospital, Pusan National University School of Medicine, Korea.
- 3Department of Radiology, Vancouver Hospital and the Health Sciences Center, University of British Columbia, Vancouver, BC, Canada.
- 4Division of Respiratory and Critical Care Medicine, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Korea.
- 5Department of Diagnostic Pathology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Korea.
- 6Department of Pathology, Mayo Clinic Scottsdale, Scottsdale AZ, USA.
- 7Biostatistics Unit, Samsung Medical Center, Korea.
- KMID: 1102710
- DOI: http://doi.org/10.3348/kjr.2005.6.3.143
Abstract
OBJECTIVE
We wanted to demonstrate and compare the serial high-resolution CTs (HRCT) and the pulmonary function test (PFT) findings of the usual interstitial pneumonia (UIP) and the non-specific interstitial pneumonia (NSIP). MATERIALS AND METHODS: The serial HRCT scans and the PFT results were retrospectively analysed and compared for 35 patients having UIP without significant honeycombing (UIP-w/o hc, < 5% of honeycombing at CT), 35 patients having UIP with honeycombing (UIP-w/i hc, > or = 5% of honeycombing), and 25 patients with NSIP. The mortality rates were also compared. Follow-up CT scans were available in 75 patients (29 UIP-w/o hc patients, 22 UIP-w/i hc patients and 24 NSIP patients) and the follow-up periods ranged from 150 to 2, 370 days. The initial and follow-up PFT data were available for 71 patients. RESULTS: On the initial CT, significant differences were present between the UIP-w/i hc patients and both the UIP-w/o hc patients and the NSIP patients in the overall extent, ground-glass opacity (GGO) away from the reticulation, reticulation and honeycombing (all p < 0.05). Improvement was noticed in five (17%) of 29 UIP-w/o hc patients, none of 22 UIP-w/i hc patients, and 9 (37%) of 24 NSIP patients; deterioration was noted in six (21%) UIP-w/o hc patients, two (9%) UIP-w/i hc patients and three (13%) NSIP patients (p = 0.044 between UIP-w/o and UIP-w/i hc; p = 0.637 between UIP-w/o hc and NSIP; p = 0.007 between UIP-w/i hc and NSIP). The serial changes of the pulmonary function in the NSIP patients were different from those noted for the UIP-w/i hc and UIP-w/o hc patients (p = 0.440 between UIP-w/o and UIP-w/i hc; p = 0.022 between UIP-w/o hc and NSIP; p = 0.003 between UIP-w/i hc and NSIP). Five (14%) of the 35 patients with UIP-w/o hc, 16 (46%) of the 35 patients with UIP-w/i hc and three (12%) of the 25 patients with NSIP died (p = 0.002, comparison for the three groups). CONCLUSION: On CT, NSIP and UIP-w/o hc patients have similar patterns of parenchymal abnormalities and a similar likelihood of change in the extent of disease on follow-up. Patients with UIP-w/i hc have distinctive features and a worst prognosis.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
HRCT Findings and Clinical Features in Non-specific and Usual Interstitial Pneumonia with Connective Tissue Diseases
Joong Kyong Ahn, Eun-Mi Koh, You Sun Lee, Hoon-Suk Cha, Man Pyo Chung, Jungho Han, Dae Kun Oh, Kyung Soo Lee
J Korean Rheum Assoc. 2007;14(3):208-218. doi: 10.4078/jkra.2007.14.3.208.
Reference
-
1. Müller NL. Clinical value of high resolution CT in chronic diffuse lung disease. AJR Am J Roentgenol. 1991. 157:1163–1170.2. Nishimura K, Izumi T, Kitaichi M, Nagai S, Itoh H. The diagnostic accuracy of high-resolution computed tomography in diffuse infiltrative lung diseases. Chest. 1993. 104:1149–1155.3. Johkoh T, Müller NL, Cartier Y, Kavanagh PV, Hartman TE, Akira M, et al. Idiopathic interstitial pneumonias: diagnostic accuracy of thin-section CT in 129 patients. Radiology. 1999. 211:555–560.4. American Thoracic Society/European Respiratory Society. American Thoracic Society/European Respiratory Society international multidisciplinary consensus classification of the idiopathic interstitial pneumonias. Am J Respir Crit Care Med. 2002. 165:277–304.5. Hartman TE, Swensen SJ, Hansell DM, Colby TV, Myers JL, Tazelaar HD, et al. Nonspecific interstitial pneumonia: variable appearance at high-resolution chest CT. Radiology. 2000. 217:701–705.6. MacDonald SL, Rubens MB, Hansell DM, Copley SJ, Desai SR, du Bois RM, et al. Nonspecific interstitial pneumonia and usual interstitial pneumonia: comparative appearances and diagnostic accuracy of thin-section CT. Radiology. 2001. 221:600–605.7. Travis WD, Matsui K, Moss J, Ferrans VJ. Idiopathic nonspecific interstitial pneumonia: prognostic significance of cellular and fibrosing patterns. Am J Surg Pathol. 2000. 24:19–33.8. Rhu J, Myers J, Mu'adhdhin D, Douglas W. Non-specific interstitial pneumonia. Clin Pulm Med. 1998. 5:104–108.9. Bjoraker JA, Ryu JH, Edwin MK, Myers JL, Tazelaar HD, Schroeder DR, et al. Prognostic significance of histopathologic subsets in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 1998. 157:199–203.10. Flaherty KR, Thwaite EL, Kazerooni EA, Gross BH, Toews GB, Colby TV, et al. Radiological versus histological diagnosis in UIP and NSIP: survival implications. Thorax. 2003. 58:143–148.11. Nagao T, Nagai S, Hiramoto Y, Hamada K, Shigematsu M, Hayashi M, et al. Serial evaluation of high-resolution computed tomography findings in patients with idiopathic pulmonary fibrosis in usual interstitial pneumonia. Respiration. 2002. 69:413–419.12. Hunninghake GW, Lynch DA, Galvin JR, Gross BH, Müller N, Schwartz DA, et al. Radiologic findings are strongly associated with a pathologic diagnosis of usual interstitial pneumonia. Chest. 2003. 124:1215–1223.13. Akira M, Sakatani M, Ueda E. Idiopathic pulmonary fibrosis: progression of honeycombing at thin-section CT. Radiology. 1993. 189:687–691.14. Park JS, Lee KS, Kim JS, Park CS, Suh YL, Choi DL, et al. Nonspecific interstitial pneumonia with fibrosis: radiographic and CT findings in seven patients. Radiology. 1995. 195:645–648.15. Kim TS, Lee KS, Chung MP, Han J, Park JS, Hwang JH, et al. Nonspecific interstitial pneumonia with fibrosis: high-resolution CT and pathologic findings. AJR Am J Roentgenol. 1998. 171:1645–1650.16. Terriff BA, Kwan SY, Chan-Yeung MM, Müller NL. Fibrosing alveolitis: chest radiography and CT as predictors of clinical and functional impairment at follow-up in 26 patients. Radiology. 1992. 184:445–449.17. Kim EY, Lee KS, Chung MP, Kwon OJ, Kim TS, Hwang JH. Nonspecific interstitial pneumonia with fibrosis: serial high-resolution CT findings with functional correlation. AJR Am J Roentgenol. 1999. 173:949–953.18. Flaherty KR, Travis WD, Colby TV, Toews GB, Kazerooni EA, Gross BH, et al. Histopathologic variability in usual and nonspecific interstitial pneumonias. Am J Respir Crit Care Med. 2001. 164:1722–1727.19. Lee JS, Im J-G, Ahn JM, Kim YM, Han MC. Fibrosing alveolitis: prognostic implication of ground-glass attenuation at high-resolution CT. Radiology. 1992. 184:451–454.20. Screaton NJ, Hiorns MP, Lee KS, Franquet T, Johkoh T, Fujimoto K, et al. Serial high resolution CT in non-specific interstitial pneumonia: prognostic value of the initial pattern. Clin Radiol. 2005. 60:96–104.21. Nishiyama O, Kondoh Y, Taniguchi H, Yamaki K, Suzuki R, Yokoi T, et al. Serial high resolution CT findings in nonspecific interstitial pneumonia/fibrosis. J Comput Assist Tomogr. 2000. 24:41–46.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Idiopathic Interstitial Pneumonias: Radiologic Findings
- A Case of Nonspecific Interstitial Pneumonia with Clinical Course of Rapid Aggravation
- Idiopathic interstitial pneumonias: clinical findings, pathogenesis, pathology and radiologic findings
- Clinical Year in Review of Interstitial Lung Diseases: Focused on Idiopathic Interstitial Pneumonia
- A Case Report of Usual Interstitial Pneumonia after Treatment of Bronchopneumonia