Korean J Ophthalmol.
2006 Mar;20(1):76-78. 10.3341/kjo.2006.20.1.76.
A Case of Multiple Cranial Nerve Palsies as the Initial Ophthalmic Presentation of Antiphospholipid Syndrome
- Affiliations
-
- 1Department of Ophthalmology, Hanyang University Guri Hospital, College of Medicine, Hanyang University, Guri City, Goyang, Korea. eyeshin@hanyang.ac.kr
- KMID: 1099077
- DOI: http://doi.org/10.3341/kjo.2006.20.1.76
Abstract
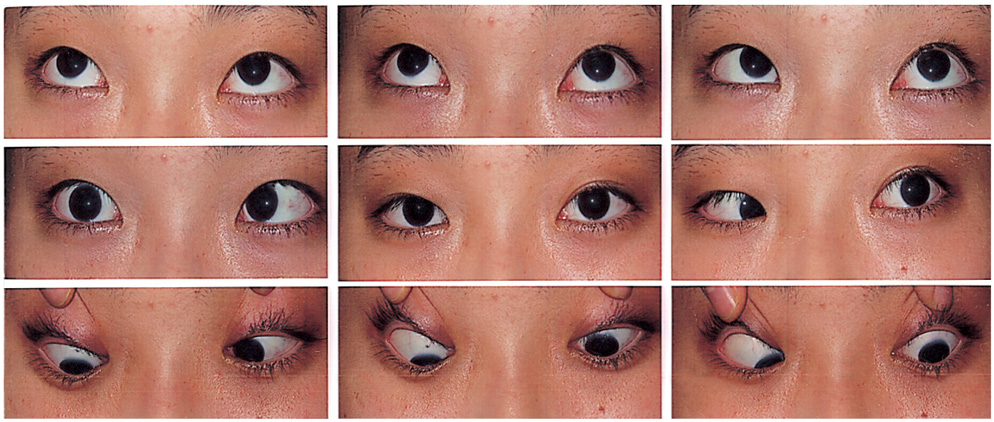
- PURPOSE: To report a case of third, fourth, and six cranial nerve palsies with antiphospholipid syndrome (APS). METHODS: Medical records of a 16 year old female diagnosed with idiopathic intracranial hypertension (IIH) in primary APS were reviewed. RESULTS: A 16 year old female presented with headache and diplopia. Ocular examinations revealed marked bilateral disc edema. She was unable to depress, adduct, and abduct in left eye and had limited abduction in the right eye. Cerebrospinal fluid had a normal composition and a pressure of 400 mmH2O. Lupus anticoagulant and IgG anticardiolipin antibody were positive. There was no clinical evidence of other autoimmune disease. Brain magnetic resonance (MR) imaging, MR angiography, and conventional angiogram with venous phase were normal. She was diagnosed with bilateral sixth, and left third and fourth cranial nerve palsies secondary to idiopathic intracranial hypertension in primary APS. CONCLUSIONS: To our knowledge this is the first reported case of concurrent third, fourth, and sixth cranial nerve palsies in a patient with primary APS.
MeSH Terms
Figure
Cited by 2 articles
-
Retinopathy Associated With Systemic Lupus Erythematosus
Chang Ki Yoon, Jung Hyun Park, Hyeong Gon Yu
J Korean Ophthalmol Soc. 2009;50(8):1215-1220. doi: 10.3341/jkos.2009.50.8.1215.Systemic Lupus Erythematosus Presenting as Monocular Elevation Deficiency
Seung Woo Kim, Yong Hyun Kim, Seung Ah Chung
J Korean Ophthalmol Soc. 2016;57(1):161-166. doi: 10.3341/jkos.2016.57.1.161.
Reference
-
1. Champion BL, Choy F, Schrieber L, et al. Isolated fascicular oculomoter nerve palsy as the initial presentation of the antiphospholipid syndrome. J Clin Neurosci. 2002. 9:691–694.2. Johnston I, Paterson A. Benign intracranial hypertension. Brain. 1974. 97:289–312.3. Weisberg LA. Benign intracranial hypertension. Medicine (Baltimore). 1975. 54:197–207.4. Boddie HG, Banna M, Bradley WG. "Benign" intracranial hypertension. A survey of the clinical and radiological features, and long-term prognosis. Brain. 1974. 97:313–326.5. McCammon A, Kaufman HH, Sears ES. Transient oculomotor paralysis in pseudotumor cerebri. Neurology. 1981. 31:182–184.6. Patton N, Beatty S, Lloyd IC. Bilateral sixth and fourth cranial nerve palsies in idiopathic intracranial hypertension. J R Soc Med. 2000. 93:80–81.7. Orefice G, De Joanna G, Coppola M, et al. Benign intracranial hypertension: a non-thrombotic complication of the primary APS? Lupus. 1995. 4:324–326.8. Falcini F, Taccetti G, Trapani S, et al. Primary APS: a report of two pediatric cases. J Rheumatol. 1991. 18:1085–1087.9. Kesler A, Ellis MH, Reshef T, et al. Idiopathic Intracranial hypertension and anticardiolipin antibodies. J Neurol Neurosurg Psychiatry. 2000. 68:379–380.10. Sussman J, Leach M, Greaves M, et al. Potentially prothrombotic abnormalities of coagulation in benign intacranial hypertension. J Neurol Neurosurg Psychiatry. 1997. 62:229–233.11. Leker RR, Steiner I. Anticardiolipin Antibodies are frequently present in patients with idiopathic intracranial hypertension. Arch Neurol. 1998. 55:817–820.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case of Ophthalmic Zoster Presenting as Multiple Cranial Nerve Palsies, Ultimately Leading to Death
- 1 case of relapsed leprosy accompanied by multiple cranial nerve palsies
- Cranial Nerve Palsies in Adult Tuberculous Meningitis
- Cryptococcal Meningoencephalitis Presenting as Cerebral Infarction and Multiple Cranial Nerve Palsies
- Two Cases of Ramsay Hunt Syndrome Complicated with Multiple Cranial Nerve Palsy and Aseptic Meningitis