Korean J Radiol.
2008 Apr;9(2):111-118. 10.3348/kjr.2008.9.2.111.
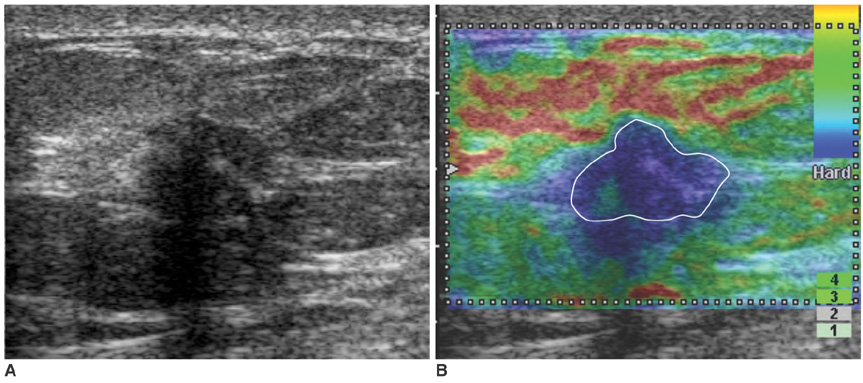
Nonpalpable Breast Masses: Evaluation by US Elastography
- Affiliations
-
- 1Department of Radiology and Clinical Research Institute, Seoul National University Hospital and the Institute of Radiation Medicine, Seoul National University Medical Research Center, Seoul, Korea. moonwk@radcom.snu.ac.kr
- 2Department of Radiology, Boramae Municipal Hospital, Seoul, Korea.
- KMID: 1098189
- DOI: http://doi.org/10.3348/kjr.2008.9.2.111
Abstract
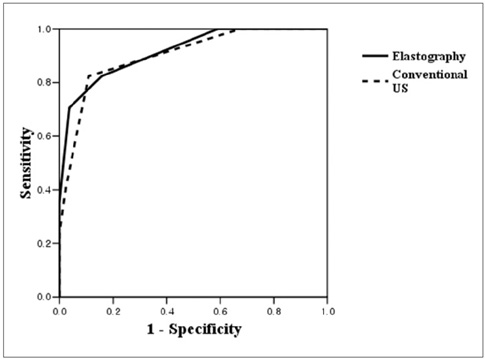
OBJECTIVE
To compare the diagnostic performances of conventional ultrasound (US) and US elastography for the differentiation of nonpalpable breast masses, and to evaluate whether elastography is helpful at reducing the number of benign biopsies, using histological analysis as a reference standard. MATERIALS AND METHODS: Conventional US and real-time elastographic images were obtained for 100 women who had been scheduled for a US-guided core biopsy of 100 nonpalpable breast masses (83 benign, 17 malignant). Two experienced radiologists unaware of the biopsy and clinical findings analyzed conventional US and elastographic images by consensus, and classified lesions based on degree of suspicion regarding the probability of malignancy. Results were evaluated by receiver operating characteristic curve analysis. In addition, the authors investigated whether a subset of lesions was categorized as suspicious by conventional US, but as benign by elastography. RESULTS: Areas under the ROC curves (Az values) were 0.901 for conventional US and 0.916 for elastography (p = 0.808). For BI-RADS category 4a lesions, 44% (22 of 50) had an elasticity score of 1 and all were found to be benign. CONCLUSION: Elastography was found to have a diagnostic performance comparable to that of conventional US for the differentiation of nonpalpable breast masses. The authors conclude that BI-RADS category 4a lesions with an elasticity score of 1 probably do not require biopsy.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Clinical Role of Breast Ultrasound
Nariya Cho, Woo Kyung Moon
J Korean Med Assoc. 2008;51(6):545-552. doi: 10.5124/jkma.2008.51.6.545.Ex Vivo Shear-Wave Elastography of Axillary Lymph Nodes to Predict Nodal Metastasis in Patients with Primary Breast Cancer
Soong June Bae, Jong Tae Park, Ah Young Park, Ji Hyun Youk, Jong Won Lim, Hak Woo Lee, Hak Min Lee, Sung Gwe Ahn, Eun Ju Son, Joon Jeong
J Breast Cancer. 2018;21(2):190-196. doi: 10.4048/jbc.2018.21.2.190.
Reference
-
1. Stavros AT, Thickman D, Rapp CL, Dennis MA, Parker SH, Sisney GA. Solid breast nodules: use of sonography to distinguish between benign and malignant lesions. Radiology. 1995. 196:123–134.2. Rahbar G, Sie AC, Hansen GC, Prince JS, Melany ML, Reynolds HE, et al. Benign versus malignant solid breast masses: US differentiation. Radiology. 1999. 213:889–894.3. Shin HJ, Kim HH, Kim SM, Kim DB, Lee YR, Kim MJ, et al. Pure and mixed tubular carcinoma of the breast: mammographic and sonographic differential features. Korean J Radiol. 2007. 8:103–110.4. Park SY, Oh KK, Kim EK, Son EJ, Chung WH. Sonographic findings of breast hamartoma: emphasis on compressibility. Yonsei Med J. 2003. 44:847–854.5. Steinberg BD, Sullivan DC, Carlson DL. Disparity mapping applied to sonography of the breast: technical note. Radiology. 1998. 207:545–550.6. Krouskop TA, Wheeler TM, Kallel F, Garra BS, Hall T. Elastic moduli of breast and prostate tissues under compression. Ultrason Imaging. 1998. 20:260–274.7. Wilson LS, Robinson DE. Ultrasonic measurement of small displacements and deformations of tissue. Ultrason Imaging. 1982. 4:71–82.8. Lerner RM, Huang SR, Parker KJ. Sonoelasticity images derived from ultrasound signals in mechanically vibrated tissues. Ultrasound Med Biol. 1990. 16:231–239.9. Ophir J, Cespedes I, Ponnekanti H, Yazdi Y, Li X. Elastography: a quantitative method for imaging the elasticity of biological tissues. Ultrason Imaging. 1991. 13:111–134.10. Garra BS, Cespedes EI, Ophir J, Spratt SR, Zuurbier RA, Magnant CM, et al. Elastography of breast lesions: initial clinical results. Radiology. 1997. 202:79–86.11. Hall TJ, Zhu Y, Spalding CS. In vivo real-time freehand palpation imaging. Ultrasound Med Biol. 2003. 29:427–435.12. Itoh A, Ueno E, Tohno E, Kamma H, Takahashi H, Shiina T, et al. Breast disease: clinical application of US elastography for diagnosis. Radiology. 2006. 239:341–350.13. American College of Radiology. Breast imaging reporting and data system (BI-RADS™) ultrasound. 2003. Reston, Va: American College of Radiology.14. Hall TJ. AAPM/RSNA physics tutorial for residents: topics in US: beyond the basics: elasticity imaging with US. Radiographics. 2003. 23:1657–1671.15. Insana MF, Pellot-Barakat C, Sridhar M, Lindfors KK. Viscoelastic imaging of breast tumor microenvironment with ultrasound. J Mammary Gland Biol Neoplasia. 2004. 9:393–404.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Future of breast elastography
- Localization of Nonpalpable Breast lesion with Ultrasonoguided Dye Injection
- Values of US-Guided Localization and Specimen US in Nonpalpable Breast Masses
- Usefulness of Ultrasound-Guided Automated Core Biopsy of Nonpalpable Breast Lesions
- Elastography of the Breast: Imaging Techniques and Pitfalls in Interpretation