Korean J Lab Med.
2009 Jun;29(3):194-198. 10.3343/kjlm.2009.29.3.194.
A Case of Natural Killer Cell Leukemia Misdiagnosed as Tuberculous Lymphadenopathy
- Affiliations
-
- 1Department of Laboratory Medicine, Catholic University Hospital of Daegu, Daegu, Korea. sgkim@cu.ac.kr
- 2Department of Anatomical Pathology, Kyoungbuk National University Hospital, Daegu, Korea.
- KMID: 1096969
- DOI: http://doi.org/10.3343/kjlm.2009.29.3.194
Abstract
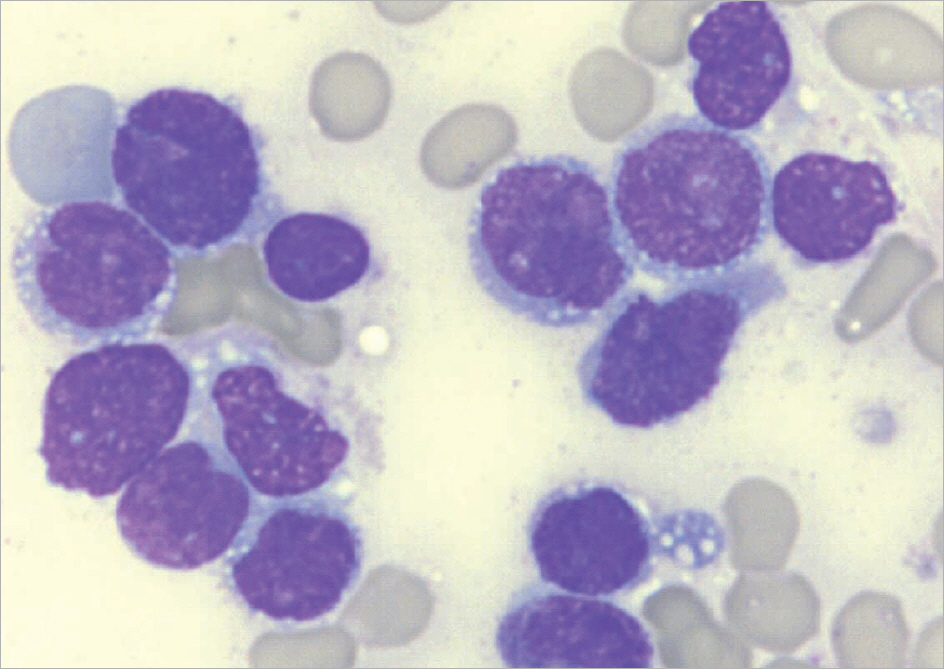
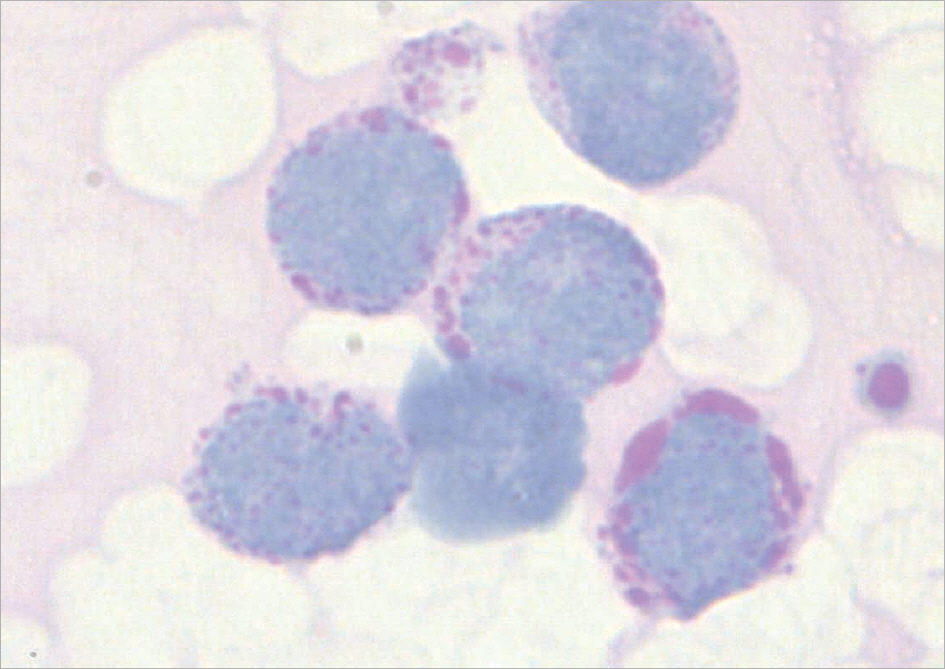
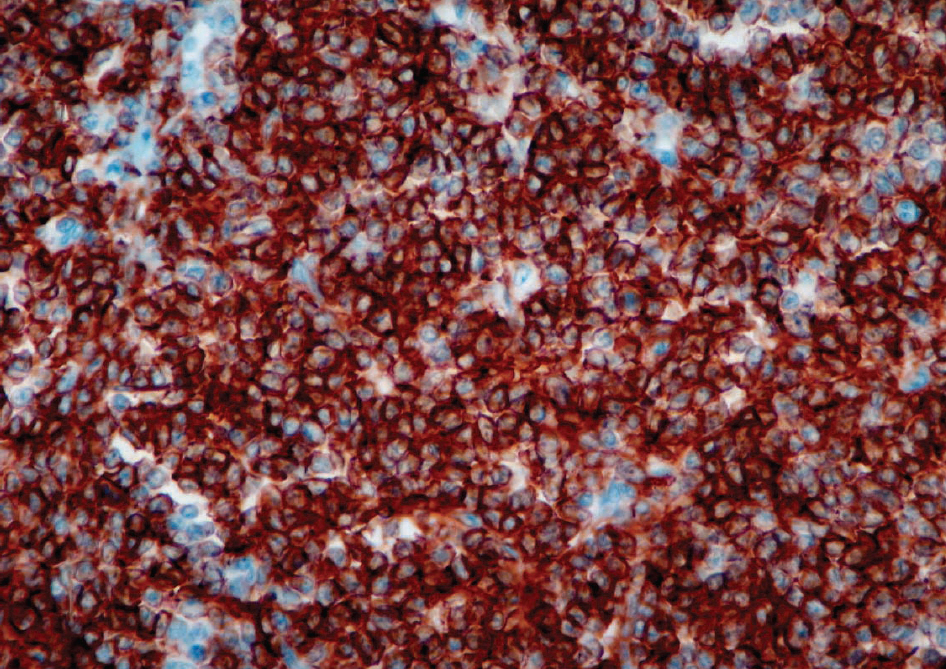
- Natural killer (NK) cell neoplasms are a group of rare but highly malignant tumors. We report here one case of NK cell leukemia. A 54-yr-old woman presented with a 2-month history of progressive left neck mass. Based on the positive result of tissue PCR for Mycobacterium tuberculosis, she was at first diagnosed with tuberculous lymphadenopathy. After two weeks, she developed generalized lymphadenopathy, hepatosplenomegaly, fever and anemia. Subsequent evaluation was performed including bone marrow aspiration and biopsy. Peripheral blood smear showed leukoerythroblastic features with 31% blasts. Bone marrow was packed with agranular blastoid cells, which were periodic acid-Schiff (PAS) positive and myeloperoxidase (MPO) negative. Immunophenotyping showed that these cells were positive for CD45 and HLA-DR, whereas negative for CD3, CD5, CD7, CD10, CD13, CD14, CD19, CD20, CD22, CD33, CD34, and CD61. Because of the absence of the markers of T-cell, B-cell, and myeloid lineage-specific antigens, we added CD16/56 for the immunophenotyping and the blasts were positive (94%). The tumor cells of biopsied lymph node were only positive for CD56, consistent with NK cell lymphoma. Epstein-Barr virus (EBV) was not detected by RNA in situ hybridization. Culture for M. tuberculosis was negative. Thus this patient was diagnosed with blastic NK cell lymphoma/leukemia involving bone marrow and lymph node.
MeSH Terms
Figure
Reference
-
1.Jaffe ES., Ralfkiaer E. Mature T-cell and NK-cell neoplasms: introduction. Jaffe ES, Harris NL, editors. World Health Organization Classification of Tumours: Pathology and genetics of tumours of hematopoietic and lymphoid tissue. Lyon, France: IARC Press;2001. p. 191–4.2.Chan JK., Jaffe ES, et al. Extranodal NK/T-cell lymphoma, nasal type. Jaffe ES, Harris NL, editors. World Health Organization Classification of Tumours: Pathology and genetics of tumours of hematopoietic and lymphoid tissue. Lyon, France: IARC Press;2001. p. 204–7.3.Trinchieri G. Biology of natural killer cells. Adv Immunol. 1989. 47:187–376.
Article4.Spits H., Lanier LL., Phillips JH. Development of human T and natural killer cells. Blood. 1995. 85:2654–70.
Article5.Robertson MJ., Ritz J. Biology and clinical relevance of human natural killer cells. Blood. 1990. 76:2421–38.
Article6.Chan JK., Wong KF, et al. Aggressive NK-cell leukemia. Jaffe ES, Harris NL, editors. World Health Organization Classification of Tumours: Pathology and genetics of tumours of hematopoietic and lymphoid tissue. Lyon, France: IARC Press;2001. p. 198–200.7.Kwong YL. Natural killer-cell malignancies: diagnosis and treatment. Leukemia. 2005. 19:2186–94.
Article8.Lau SK., Wei WI., Hsu C., Engzell UC. Efficacy of fine needle aspiration cytology in the diagnosis of tuberculous cervical lymphadenopathy. J Laryngol Otol. 1990. 104:24–7.
Article9.Yang HY., Lee HJ., Park SY., Lee KK., Suh JT. Comparison of in-house polymerase chain reaction assay with conventional techniques forthe detection of Mycobacterium tuberculosis. Korean J Lab Med. 2006. 26:174–8. (양희영, 이희주, 박수연, 이광길, 서진태. 결핵 진단에 있어서 In-house 중합효소연쇄반응법과 전통적인 진단 방법간의 비교검토. 대한진단검사의학회지 2006;26:174-8.).10.Singh KK., Muralidhar M., Kumar A., Chattopadhyaya TK., Kapila K., Singh MK, et al. Comparison of in house polymerase chain reaction with conventional techniques for the detection of Mycobacterium tuberculosis DNA in granulomatous lymphadenopathy. J Clin Pathol. 2000. 53:355–61.
Article11.Goel MM., Ranjan V., Dhole TN., Srivastava AN., Mehrotra A., Kushwaha MR, et al. Polymerase chain reaction vs. conventional diagnosis in fine needle aspirates of tuberculous lymph nodes. Acta Cytol. 2001. 45:333–40.
Article12.Vago L., Barberis M., Gori A., Scarpellini P., Sala E., Nebuloni M, et al. Nested polymerase chain reaction for Mycobacterium tuberculosis IS6110 sequence on formalin-fixed paraffin-embedded tissues with granulomatous diseases for rapid diagnosis of tuberculosis. Am J Clin Pathol. 1998. 109:411–5.13.Oshimi K. Leukemia and lymphoma of natural killer lineage cells. Int J Hematol. 2003. 78:18–23.
Article14.Sheibani K., Winberg CD., Burke JS., Nathwani BN., Blayney DW., Van de Velde S, et al. Lymphoblastic lymphoma expressing natural killer cell-associated antigens: a clinicopathologic study of 6 cases. Leuk Res. 1987. 11:371–7.15.Freud AG., Caligiuri MA. Human natural killer cell development. Immunol Rev. 2006. 214:56–72.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Quantifing the Circulating Epstein-Barr Virus (EBV) DNA to Monitor a Case of Aggressive Natural Killer Cell Leukemia
- A Case of Natural Killer Like T Cell Lymphoma Misdiagnosed as Behcet's Enteritis of the Terminal Ileum
- A Study of Natural Killer Cell Activities , T Cells and T Cell Subsets in Vitiligo
- Clinical significance of cell-mediated immunity and natural killer cell activity related with septic complication in panperitonitis patients
- A Case of Natural Killer T-cell Lymphoma of the Tongue