J Korean Med Sci.
2011 Jul;26(7):938-944. 10.3346/jkms.2011.26.7.938.
Interleukin-17 in Various Ocular Surface Inflammatory Diseases
- Affiliations
-
- 1Department of Ophthalmology, Hanyang University Guri Hospital, Guri, Korea.
- 2Seoul Artificial Eye Center, Seoul National University Hospital Clinical Research Institute, Seoul, Korea. kmk9@snu.ac.kr
- 3Department of Ophthalmology, Seoul National University College of Medicine, Seoul, Korea.
- 4GM Eye Clinic, Seoul, Korea.
- KMID: 1094267
- DOI: http://doi.org/10.3346/jkms.2011.26.7.938
Abstract
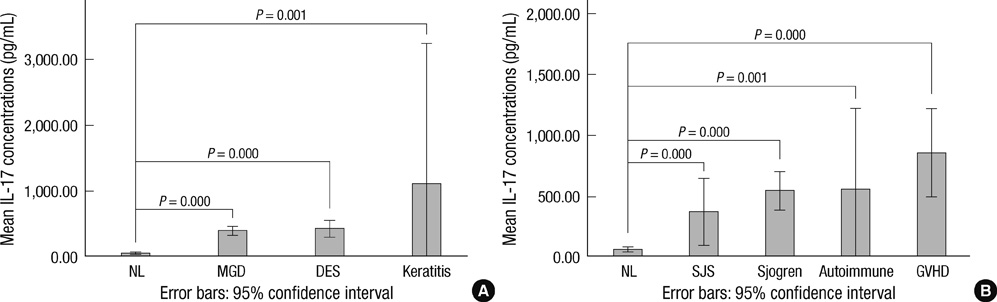
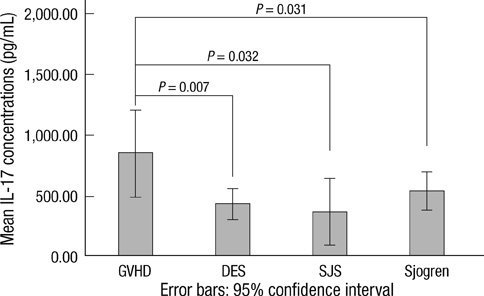
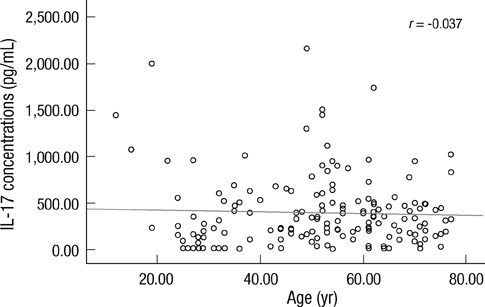
- Recently, the association of Th-17 cells or IL-17 with ocular inflammatory diseases such as uveitis, scleritis and dry eye syndrome was discovered. We assessed whether interleukin (IL)-17 was present in the tears of various ocular surface inflammatory diseases and the tear IL-17 concentrations were clinically correlated with various ocular surface inflammatory diseases. We measured concentrations of IL-17 in tears of normal subjects (n = 28) and patients (n = 141) with meibomian gland dysfunction (MGD), dry eye syndrome (DES), Sjogren syndrome (SS), Stevens-Johnson syndrome (SJS), graft-versus-host disease (GVHD), filamentary keratitis, and autoimmune keratitis associated with rheumatoid arthritis or systemic lupus erythematosus. Clinical epitheliopathy scores were based on the surface area of corneal and conjunctival fluorescein staining. The mean concentrations of IL-17 in tears of patients with filamentary keratitis, GVHD, autoimmune keratitis, SS, DES, MGD, SJS were significantly higher in order than that in normal subjects. Tear IL-17 concentration was significantly correlated with clinical epitheilopathy scores in the patients with systemic inflammatory disease, while tear IL-17 was not correlated with clinical severity of the cornea and conjunctiva in the dry eye patients without any systemic inflammatory disease. Tear IL-17 is likely to correlate clinically with corneal disease severity only in the patients with systemic inflammatory disease.
MeSH Terms
-
Adult
Aged
Dry Eye Syndromes/*metabolism
Eye Diseases/diagnosis/*metabolism
Eyelid Diseases/metabolism
Female
Graft vs Host Disease/metabolism
Humans
Interleukin-17/*analysis
Keratitis/metabolism
Male
Meibomian Glands/physiopathology
Middle Aged
Severity of Illness Index
Sjogren's Syndrome/metabolism
Stevens-Johnson Syndrome/metabolism
Tears/metabolism
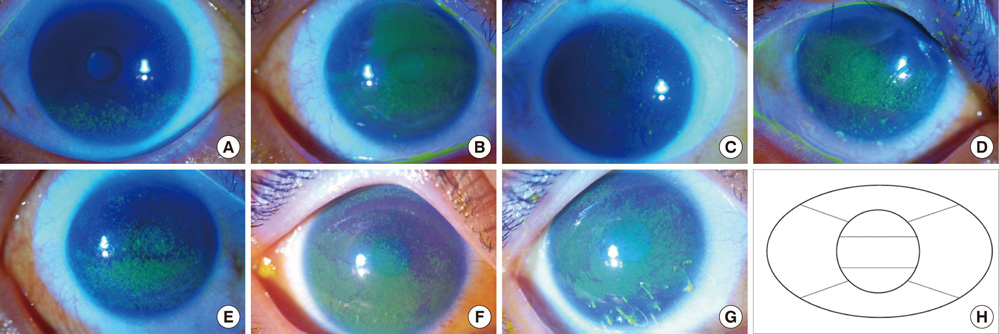
Figure
Reference
-
1. Aggarwal S, Ghilardi N, Xie MH, de Sauvage FJ, Gurney AL. Interleukin-23 promotes a distinct CD4 T cell activation state characterized by the production of interleukin-17. J Biol Chem. 2003. 278:1910–1914.2. Harrington LE, Hatton RD, Mangan PR, Turner H, Murphy TL, Murphy KM, Weaver CT. Interleukin 17-producing CD4+ effector T cells develop via a lineage distinct from the T helper type 1 and 2 lineages. Nat Immunol. 2005. 6:1123–1132.3. Zheng Y, Danilenko DM, Valdez P, Kasman I, Eastham-Anderson J, Wu J, Ouyang W. Interleukin-22, a T(H)17 cytokine, mediates IL-23-induced dermal inflammation and acanthosis. Nature. 2007. 445:648–651.4. Nakae S, Nambu A, Sudo K, Iwakura Y. Suppression of immune induction of collagen-induced arthritis in IL-17-deficient mice. J Immunol. 2003. 171:6173–6177.5. Kebir H, Kreymborg K, Ifergan I, Dodelet-Devillers A, Cayrol R, Bernard M, Giuliani F, Arbour N, Becher B, Prat A. Human TH17 lymphocytes promote blood-brain barrier disruption and central nervous system inflammation. Nat Med. 2007. 13:1173–1175.6. Yen D, Cheung J, Scheerens H, Poulet F, McClanahan T, McKenzie B, Kleinschek MA, Owyang A, Mattson J, Blumenschein W, Murphy E, Sathe M, Cua DJ, Kastelein RA, Rennick D. IL-23 is essential for T cell-mediated colitis and promotes inflammation via IL-17 and IL-6. J Clin Invest. 2006. 116:1310–1316.7. Singh R, Aggarwal A, Misra R. Th1/Th17 cytokine profiles in patients with reactive arthritis/undifferentiated spondyloarthropathy. J Rheumatol. 2007. 34:2285–2290.8. Tesmer LA, Lundy SK, Sarkar S, Fox DA. Th17 cells in human disease. Immunol Rev. 2008. 223:87–113.9. Hashimoto T, Akiyama K, Kobayashi N, Mori A. Comparison of IL-17 production by helper T cells among atopic and nonatopic asthmatics and control subjects. Int Arch Allergy Immunol. 2005. 137:Suppl 1. 51–54.10. Burlingham WJ, Love RB, Jankowska-Gan E, Haynes LD, Xu Q, Bobadilla JL, Meyer KC, Hayney MS, Braun RK, Greenspan DS, Gopalakrishnan B, Cai J, Brand DD, Yoshida S, Cummings OW, Wilkes DS. IL-17-dependent cellular immunity to collagen type V predisposes to obliterative bronchiolitis in human lung transplants. J Clin Invest. 2007. 117:3498–3506.11. Yoshimura T, Sonoda KH, Ohguro N, Ohsugi Y, Ishibashi T, Cua DJ, Kobayashi T, Yoshida H, Yoshimura A. Involvement of Th17 cells and the effect of anti-IL-6 therapy in autoimmune uveitis. Rheumatology (Oxford). 2009. 48:347–354.12. Amadi-Obi A, Yu CR, Liu X, Mahdi RM, Clarke GL, Nussenblatt RB, Gery I, Lee YS, Egwuagu CE. TH17 cells contribute to uveitis and scleritis and are expanded by IL-2 and inhibited by IL-27/STAT1. Nat Med. 2007. 13:711–718.13. Chauhan SK, El Annan J, Ecoiffier T, Goyal S, Zhang Q, Saban DR, Dana R. Autoimmunity in dry eye is due to resistance of Th17 to Treg suppression. J Immunol. 2009. 182:1247–1252.14. De Paiva CS, Chotikavanich S, Pangelinan SB, Pitcher JD 3rd, Fang B, Zheng X, Ma P, Farley WJ, Siemasko KF, Niederkorn JY, Stern ME, Li DQ, Pflugfelder SC. IL-17 disrupts corneal barrier following desiccating stress. Mucosal Immunol. 2009. 2:243–253.15. Molesworth-Kenyon SJ, Yin R, Oakes JE, Lausch RN. IL-17 receptor signaling influences virus-induced corneal inflammation. J Leukoc Biol. 2008. 83:401–408.16. Shoji J, Kawaguchi A, Gotoh A, Inada N, Sawa M. Concentration of soluble interleukin-6 receptors in tears of allergic conjunctival disease patients. Jpn J Ophthalmol. 2007. 51:332–337.17. Kaido M, Goto E, Dogru M, Tsubota K. Punctal occlusion in the management of chronic Stevens-Johnson syndrome. Ophthalmology. 2004. 111:895–900.18. Nichols KK, Mitchell GL, Zadnik K. The repeatability of clinical measurements of dry eye. Cornea. 2004. 23:272–285.19. Zheng X, Bian F, Ma P, De Paiva CS, Stern M, Pflugfelder SC, Li DQ. Induction of Th17 differentiation by corneal epithelial-derived cytokines. J Cell Physiol. 2010. 222:95–102.20. Heo YJ, Park MK, Ju JH, Park KS, Cho ML, Kim HY. The effect of inflammatory cytokines on the differentiation of Th17 cells in human peripheral blood. J Korean Rheum Assoc. 2009. 16:133–143.21. McGeachy MJ, Cua DJ. Th17 cell differentiation: the long and winding road. Immunity. 2008. 28:445–453.22. Ziolkowska M, Koc A, Luszczykiewicz G, Ksiezopolska-Pietrzak K, Klimczak E, Chwalinska-Sadowska H, Maslinski W. High levels of IL-17 in rheumatoid arthritis patients: IL-15 triggers in vitro IL-17 production via cyclosporin A-sensitive mechanism. J Immunol. 2000. 164:2832–2838.23. Katsifis GE, Rekka S, Moutsopoulos NM, Pillemer S, Wahl SM. Systemic and local interleukin-17 and linked cytokines associated with Sjögren's syndrome immunopathogenesis. Am J Pathol. 2009. 175:1167–1177.24. Oh JY, Kim MK, Choi HJ, Ko JH, Kang EJ, Lee HJ, Wee WR, Lee JH. Investigating the relationship between serum interleukin-17 levels and systemic immune-mediated disease in patients with dry eye syndrome. Korean J Ophthalmol. 2011. 25:73–76.25. Carlson MJ, West ML, Coghill JM, Panoskaltsis-Mortari A, Blazar BR, Serody JS. In vitro-differentiated TH17 cells mediate lethal acute graft-versus-host disease with severe cutaneous and pulmonary pathologic manifestations. Blood. 2009. 113:1365–1374.26. Kappel LW, Goldberg GL, King CG, Suh DY, Smith OM, Ligh C, Holland AM, Grubin J, Mark NM, Liu C, Iwakura Y, Heller G, van den Brink MR. IL-17 contributes to CD4-mediated graft-versus-host disease. Blood. 2009. 113:945–952.27. Iclozan C, Yu Y, Liu C, Liang Y, Yi T, Anasetti C, Yu XZ. T helper17 cells are sufficient but not necessary to induce acute graft-versus-host disease. Biol Blood Marrow Transplant. 2010. 16:170–178.28. Rao DA, Tracey KJ, Pober JS. IL-1alpha and IL-1beta are endogenous mediators linking cell injury to the adaptive alloimmune response. J Immunol. 2007. 179:6536–6546.29. Gu Y, Yang J, Ouyang X, Liu W, Li H, Yang J, Bromberg J, Chen SH, Mayer L, Unkeless JC, Xiong H. Interleukin 10 suppresses Th17 cytokines secreted by macrophages and T cells. Eur J Immunol. 2008. 38:1807–1813.30. O'Brien RL, Roark CL, Born WK. IL-17-producing gammadelta T cells. Eur J Immunol. 2009. 39:662–666.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical and Immunological Responses in Ocular Demodecosis
- Targeting Interleukin-17 and Th17 in Immune Inflammatory Diseases
- Interleukin-17 in the Inflammatory Bowel Disease
- Elevated interleukin-10 levels in patients with ocular toxoplasmosis
- Effects of Platelet-rich Plasma on Ocular Surface in Patients with Dry Eye Syndrome: Clinico-experimental Analysis