Korean J Radiol.
2007 Dec;8(6):531-540. 10.3348/kjr.2007.8.6.531.
Hydatid Disease Involving Some Rare Locations in the Body: a Pictorial Essay
- Affiliations
-
- 1KSU Medical School Department of Radiology 46050 Kahramanmaras-Turkey. myuksel@ksu.edu.tr
- 2Ege University Medical School Department of Radiology 35100 Izmir-Turkey.
- 3KSU Medical School Department of Pathology 46050 Kahramanmaras-Turkey.
- 4KSU Medical School Department of General Surgery 46050 Kahramanmaras-Turkey.
- KMID: 1089441
- DOI: http://doi.org/10.3348/kjr.2007.8.6.531
Abstract
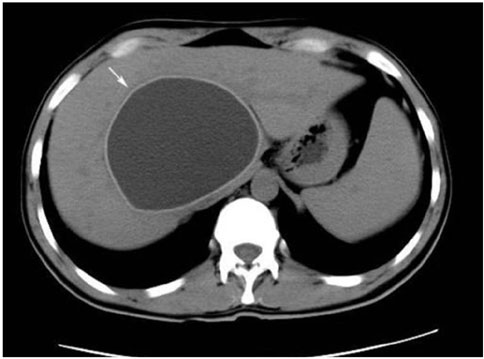
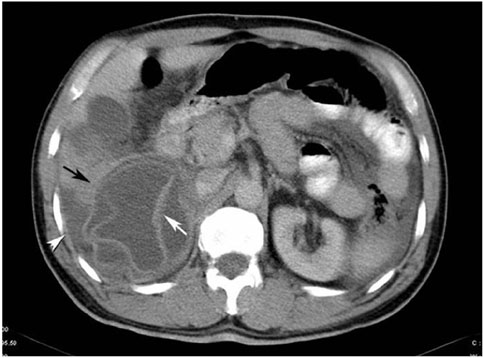
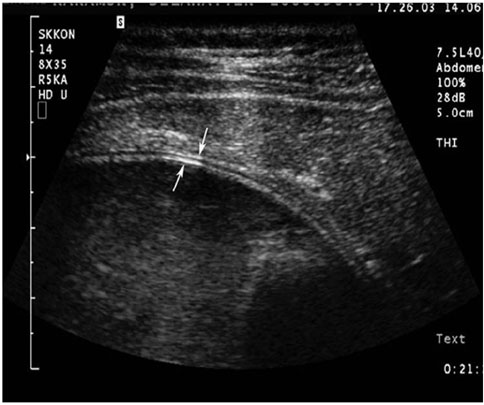
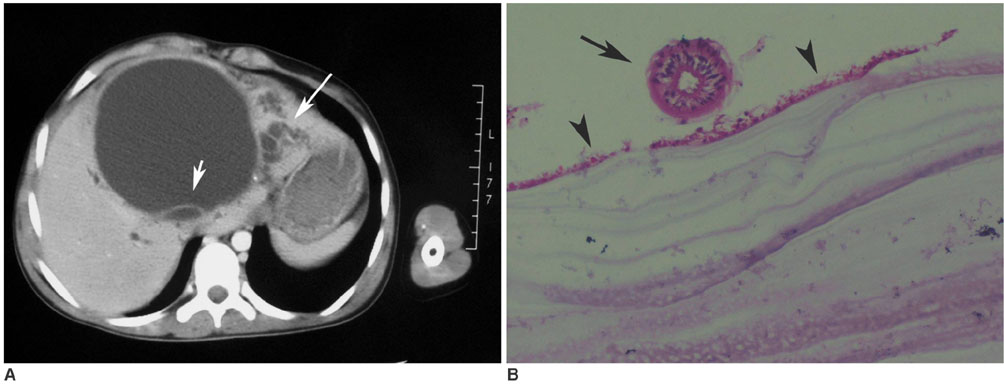
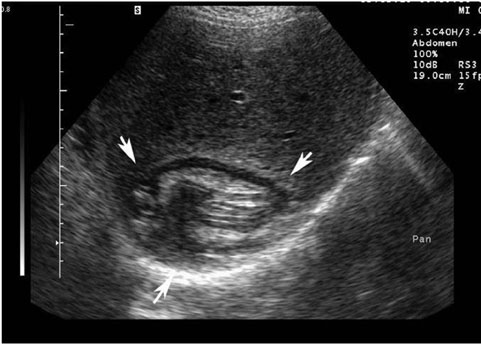
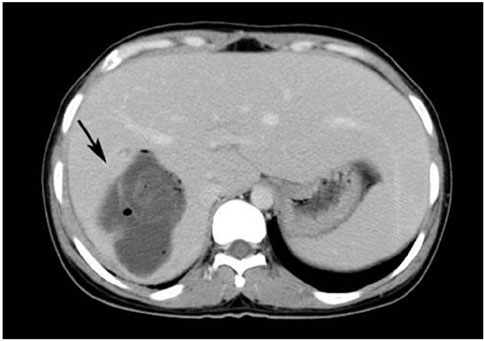
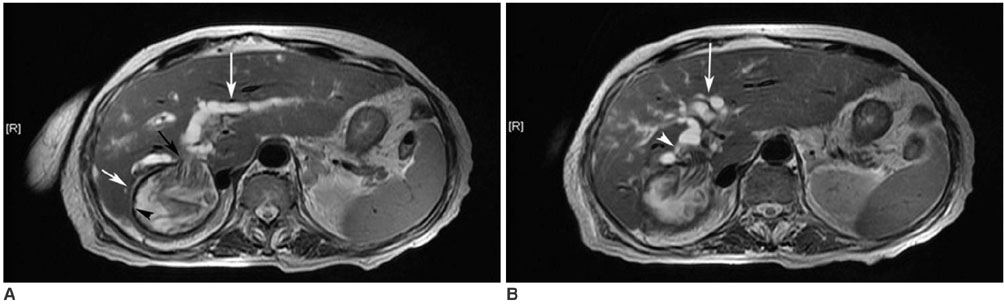
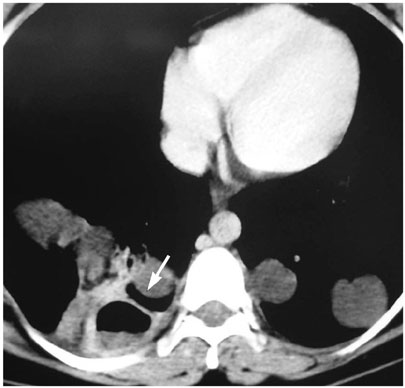
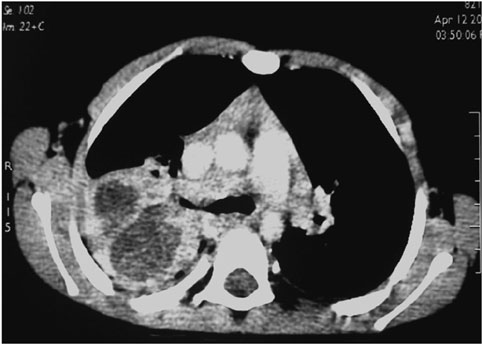
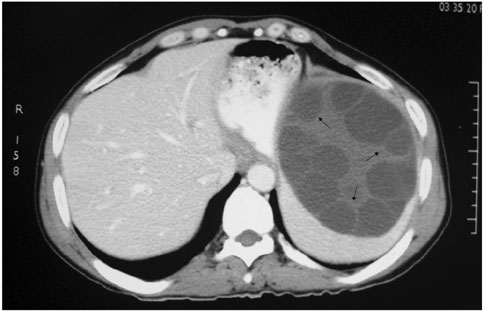
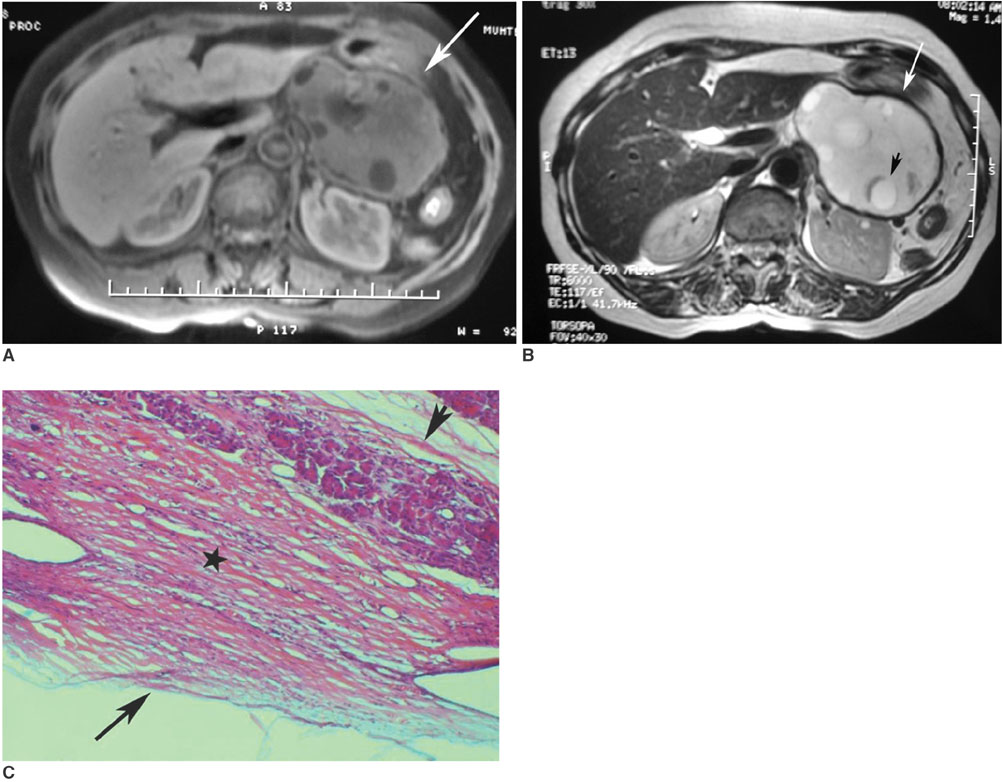
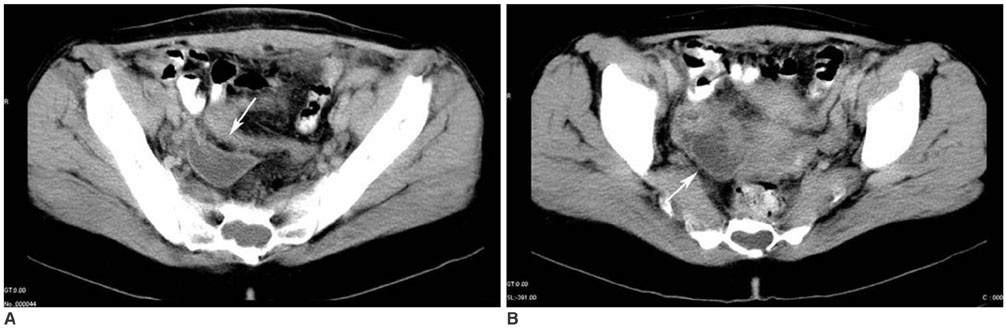
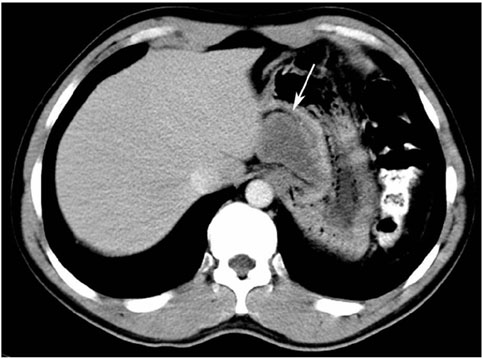
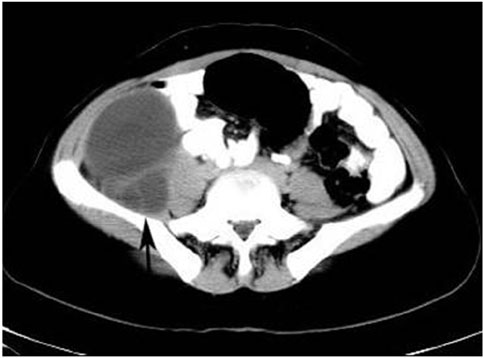
- Hydatid disease (HD) is an endemic illness in many countries, and it poses an important public health problem that's influenced by peoples' socioeconomic status and migration that spreads this disease. Although rare, it may occur in any organ or tissue. The most common site is the liver (59-75%), followed in frequency by lung (27%), kidney (3%), bone (1-4%) and brain (1-2%). Other sites such as the heart, spleen, pancreas and muscles are very rarely affected. Unusual sites for this disease can cause diagnostic problems. This pictorial essay illustrates various radiological findings of HD in the liver, spleen, kidney, pancreas, peritoneal cavity, omentum, adrenal, ovary, lung, mediastinum and retroperitoneum. Familiarity with the imaging findings of HD may be helpful in making an accurate diagnosis and preventing potential complications.
MeSH Terms
-
Abdominal Cavity/parasitology/radiography
Adolescent
Adult
Child
Child, Preschool
Contrast Media/administration & dosage
Digestive System/pathology/radiography/ultrasonography
Digestive System Diseases/diagnosis/parasitology
Echinococcosis/*diagnosis/parasitology/*radiography
Endocrine Glands/parasitology/radiography
Female
Humans
Kidney/parasitology/pathology
Liver/parasitology/radiography
Lung/parasitology/radiography
Magnetic Resonance Imaging/methods
Male
Mediastinum/parasitology/radiography
Middle Aged
Pancreas/parasitology/radiography
Radiographic Image Enhancement/methods
Spleen/parasitology/radiography
Tomography, X-Ray Computed/methods
Figure
Reference
-
1. Lewall DB. Hydatid disease: biology, pathology, imaging and classification. Clin Radiol. 1998. 53:863–874.2. Polat P, Kantarci M, Alper F, Suma S, Koruyucu MB, Okur A. Hydatid disease from head to toe. Radiographics. 2003. 23:475–494.3. Pedrosa I, Saiz A, Arrazola J, Ferreiros J, Pedrosa CS. Hydatid disease: radiologic and pathologic features and complications. Radiographics. 2000. 20:795–817.4. Czermak BV, Unsinn KM, Gotwald T, Niehoff AA, Freund MC, Waldenberger P, et al. Echinococcus granulosus revisited: radiologic patterns seen in pediatric and adult patients. AJR Am J Roentgenol. 2001. 177:1051–1056.5. Beggs I. The radiology of hydatid disease. AJR Am J Roentgenol. 1985. 145:639–648.6. Erdem LO, Erdem CZ, Karlioguz K, Uner C. Radiologic aspects of abdominal hydatidosis in children: a study of 31 cases in Turkey. Clin Imaging. 2004. 28:196–200.7. Papageorgiou KI, Kaniorou-Larai M, Mathew RG. An unusual presentation of hydatid cyst within the soft tissues of the back: re-investigation of the undiagnosed lung opacity. Respir Med. 2005. 99:1191–1194.8. Von Sinner W, te Strake L, Clark D, Sharif H. MR imaging in hydatid disease. AJR Am J Roentgenol. 1991. 157:741–745.9. Haddad MC, Birjawi GA, Khouzami RA, Khoury NJ, El-Zein YR, Al-Kutoubi AO. Unilocular hepatic echinococcal cysts: sonography and computed tomography findings. Clin Radiol. 2001. 56:746–750.10. Kiresi DA, Karabacakoglu A, Odev K, Karakose S. Uncommon locations of hydatid cysts. Acta Radiol. 2003. 44:622–636.11. Koul PA, Koul AN, Wahid A, Mir FA. CT in pulmonary hydatid disease: unusual appearances. Chest. 2000. 118:1645–1647.12. Escudero MD, Sabater L, Calvete J, Camps B, Labios M, Lledo S. Arterial hypertension due to primary adrenal hydatid cyst. Surgery. 2002. 132:894–895.13. Dahniya MH, Hanna RM, Ashebu S, Muhtaseb SA, el-Beltagi A, Badr S, et al. The imaging appearances of hydatid disease at some unusual sites. Br J Radiol. 2001. 74:283–289.14. Canda MS, Guray M, Canda T, Astarcioglu H. The pathology of echinococcosis and the current echinococcosis problem in western turkey (a report of pathologic features in 80 cases). Turk J Med Sci. 2003. 33:369–374.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Hepatic Hydatid Disease Causing Gastric Ulcer as a Rare Complication
- Double Retroperitoneal Hydatid Localization: A Case Report
- CT Findings of Central Airway Lesions Causing Airway Stenosis-Visualization and Quantification: A Pictorial Essay
- Systemic Manifestations of Immunoglobulin G4-Related Disease: A Pictorial Essay
- Multi-Detector CT Findings of Typical and Atypical Appendicitis: A Pictorial Essay