Korean J Radiol.
2007 Dec;8(6):475-483. 10.3348/kjr.2007.8.6.475.
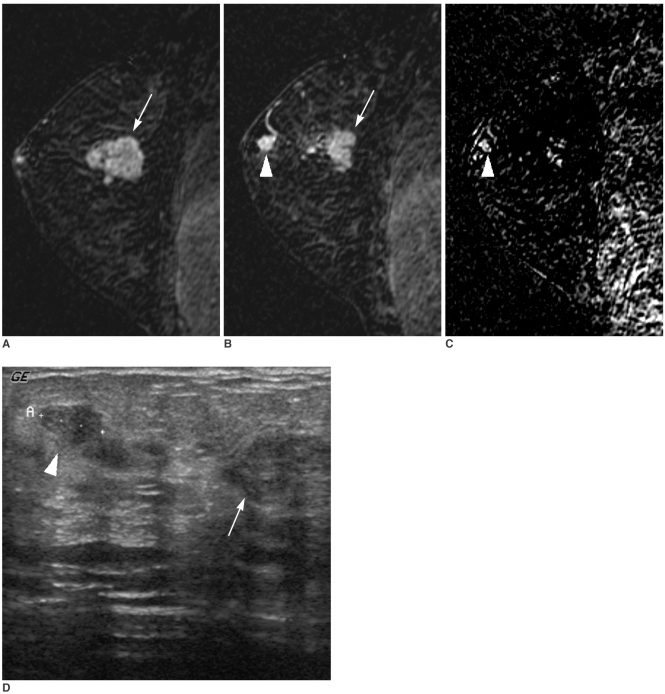
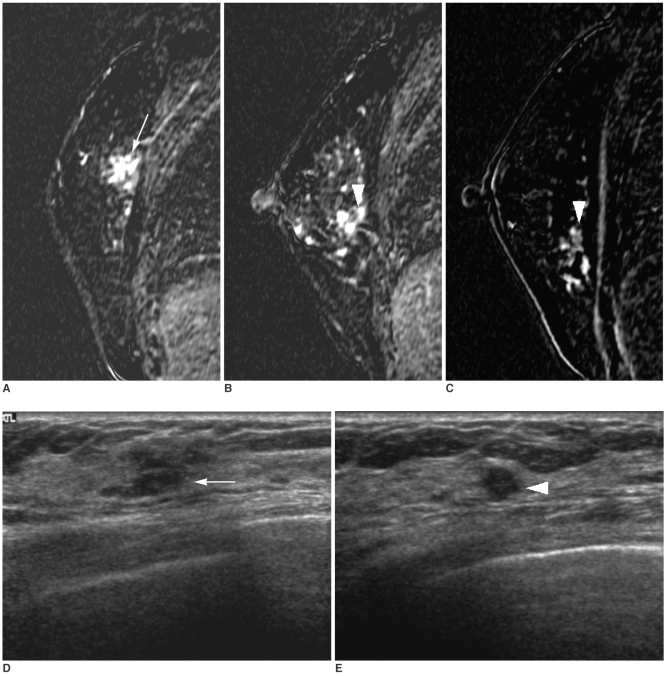
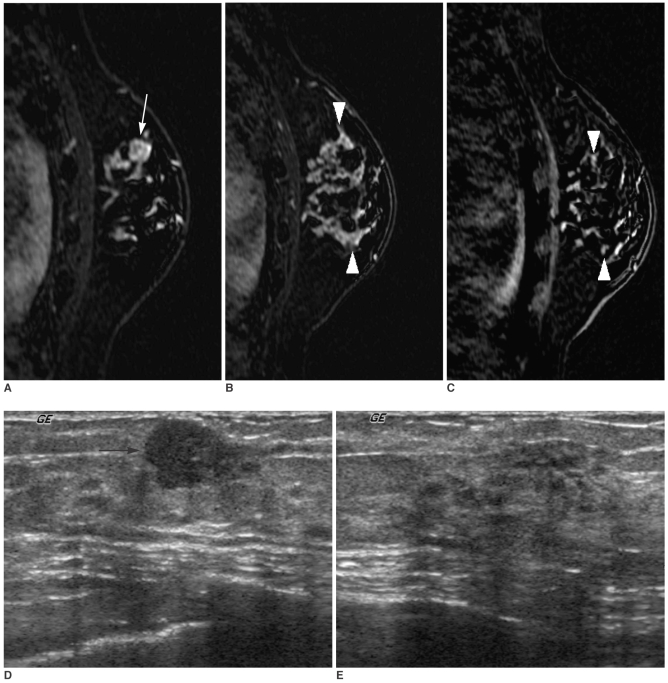
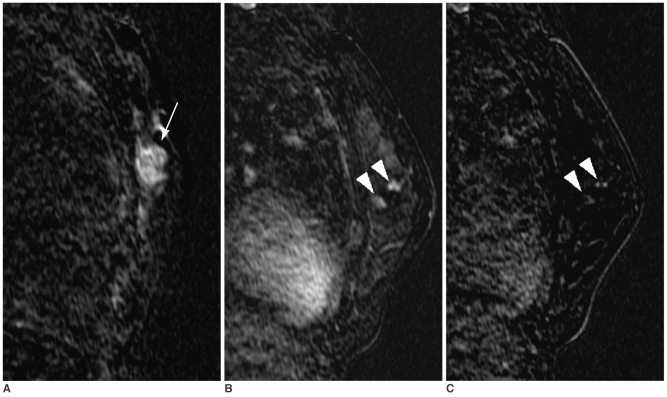
Targeted Ultrasound for MR-Detected Lesions in Breast Cancer Patients
- Affiliations
-
- 1Department of Radiology and Center for Imaging Science, Samsung Medical Center, Sunkyunkwan University School of Medicine, Seoul, Korea. bkhan@smc.samsung.co.kr
- KMID: 1089434
- DOI: http://doi.org/10.3348/kjr.2007.8.6.475
Abstract
- OBJECTIVE: To investigate the usefulness of targeted ultrasound (US) in the identification of additional suspicious lesions found by magnetic resonance (MR) imaging in breast cancer patients and the changes in treatment based on the identification of the lesions by the use of targeted US. MATERIALS AND METHODS: One-hundred forty nine patients who underwent breast MR imaging for a preoperative evaluation of breast cancer between January 2002 and July 2004 were included in the study. We searched all cases for any additional lesions that were found initially by MR imaging and investigated the performance of targeted US in identifying the lesions. We also investigated their pathological outcomes and changes in treatment as a result of lesion identification. RESULTS: Of the 149 patients with breast cancer, additional suspicious lesions were detected with MR imaging in 62 patients (42%). Of the 69 additional lesions found in those 62 patients, 26 (38%) were confirmed as cancers by histology. Thirty-eight lesions in 31 patients were examined with targeted US and were histologically revealed as cancers in 18 (47%), high risk lesions in two (5%), benign lesions in 15 (39%), and unidentified lesions in three (8%). The cancer rate was statistically higher in lesions with a US correlate than in lesions without a US correlate (p = 0.028). Of 31 patients, the surgical plan was altered in 27 (87%). The use of targeted US justified a change in treatment for 22 patients (81%) and misled five patients (19%) into having an unnecessary surgical excision. CONCLUSION: Targeted US can play a useful role in the evaluation of additional suspicious lesions detected by MR imaging in breast cancer patients, but is limited in lesions without a US correlate.
MeSH Terms
-
Adult
Aged
Biopsy
Breast/pathology
Breast Diseases/diagnosis/surgery
Breast Neoplasms/*diagnosis/surgery
Carcinoma, Ductal, Breast/*diagnosis/surgery
Carcinoma, Intraductal, Noninfiltrating/*diagnosis/surgery
Carcinoma, Lobular/*diagnosis/surgery
Contrast Media/administration & dosage
Diagnosis, Differential
False Negative Reactions
False Positive Reactions
Female
Humans
Image Enhancement/methods
Imaging, Three-Dimensional/methods
Magnetic Resonance Imaging/*methods
Middle Aged
Predictive Value of Tests
Sensitivity and Specificity
Ultrasonography, Mammary/*methods
Figure
Cited by 1 articles
-
Clinical Outcome of Magnetic Resonance Imaging-Detected Additional Lesions in Breast Cancer Patients
Gi-Won Ha, Mi Suk Yi, Byoung Kil Lee, Hyun Jo Youn, Sung Hoo Jung
J Breast Cancer. 2011;14(3):213-218. doi: 10.4048/jbc.2011.14.3.213.
Reference
-
1. van den Bosch MA, Daniel BL. MR-guided interventions of the breast. Magn Reson Imaging Clin N Am. 2005; 13:505–517. PMID: 16084416.
Article2. Atalar E, Menard C. MR-guided interventions for prostate cancer. Magn Reson Imaging Clin N Am. 2005; 13:491–504. PMID: 16084415.
Article3. LaTrenta LR, Menell JH, Morris EA, Abramson AF, Dershaw DD, Liberman L. Breast lesions detected with MR imaging: utility and histopathologic importance of identification with US. Radiology. 2003; 227:856–861. PMID: 12773685.
Article4. Sim LS, Hendriks JH, Bult P, Fook-Chong SM. US correlation for MRI-detected breast lesions in women with familial risk of breast cancer. Clin Radiol. 2005; 60:801–806. PMID: 15978891.
Article5. Londero V, Bazzocchi M, Del Frate C, Puglisi F, Di Loreto C, Francescutti G, et al. Locally advanced breast cancer: comparison of mammography, sonography and MR imaging in evaluation of residual disease in women receiving neoadjuvant chemotherapy. Eur Radiol. 2004; 14:1371–1379. PMID: 14986052.
Article6. Liberman L, Morris EA, Dershaw DD, Abramson AF, Tan LK. MR imaging of the ipsilateral breast in women with percutaneously proven breast cancer. AJR Am J Roentgenol. 2003; 180:901–910. PMID: 12646427.
Article7. Choi N, Han BK, Choe YH, Kim HS. Three-phase dynamic breast magnetic resonance imaging with two-way subtraction. J Comput Assist Tomogr. 2005; 29:834–841. PMID: 16272861.
Article8. Kuhl CK, Mielcareck P, Klaschik S, Leutner C, Wardelmann E, Gieseke J, et al. Dynamic breast MR imaging: are signal intensity time course data useful for differential diagnosis of enhancing lesions? Radiology. 1999; 211:101–110. PMID: 10189459.
Article9. Mullen DJ, Eisen RN, Newman RD, Perrone PM, Wilsey JC. The use of carbon marking after stereotactic large-core-needle breast biopsy. Radiology. 2001; 218:255–260. PMID: 11152811.
Article10. Gilles R, Guinebretiere JM, Lucidarme O, Cluzel P, Janaud G, Finet JF, et al. Nonpalpable breast tumors: diagnosis with contrast-enhanced subtraction dynamic MR imaging. Radiology. 1994; 191:625–631. PMID: 8184038.
Article11. Harms SE, Flamig DP, Hesley KL, Meiches MD, Jensen RA, Evans WP, et al. MR imaging of the breast with rotating delivery of excitation off resonance: clinical experience with pathologic correlation. Radiology. 1993; 187:493–501. PMID: 8475297.
Article12. Orel SG, Schnall MD. MR imaging of the breast for the detection, diagnosis, and staging of breast cancer. Radiology. 2001; 220:13–30. PMID: 11425968.
Article13. Beran L, Liang W, Nims T, Paquelet J, Sickle-Santanello B. Correlation of targeted ultrasound with magnetic resonance imaging abnormalities of the breast. Am J Surg. 2005; 190:592–594. PMID: 16164928.
Article14. Obdeijn IM, Brouwers-Kuyper EM, Tilanus-Linthorst MM, Wiggers T, Oudkerk M. MR imaging-guided sonography followed by fine-needle aspiration cytology in occult carcinoma of the breast. AJR Am J Roentgenol. 2000; 174:1079–1084. PMID: 10749254.
Article15. Panizza P, De Gaspari A, Vanzulli A, Rodighiero M, Camalori M, Del Maschio A. Accuracy of post-MR imaging second-looksonography in previously undetected breast lesions. Radiology. 1997; 205(Suppl):489. (Abstract).16. Bedrosian I, Mick R, Orel SG, Schnall M, Reynolds C, Spitz FR, et al. Changes in the surgical management of patients with breast carcinoma based on preoperative magnetic resonance imaging. Cancer. 2003; 98:468–473. PMID: 12879462.
Article17. Heywang-Kobrunner SH, Heinig A, Schaumloffel U, Viehweg P, Buchmann J, Lampe D, et al. MR-guided percutaneous excisional and incisional biopsy of breast lesions. Eur Radiol. 1999; 9:1656–1665. PMID: 10525886.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Fusion Imaging of MRI and US for Evaluating Breast Lesions
- Tips for finding magnetic resonance imaging-detected suspicious breast lesions using second-look ultrasonography: a pictorial essay
- Usefulness of Second-look Ultrasound for Preoperative Breast MRI-detected Suspicious Lesions in Breast Cancer Patients
- Clinical Outcome of Magnetic Resonance Imaging-Detected Additional Lesions in Breast Cancer Patients
- Usefulness of Ultrasound-Guided Automated Core Biopsy of Nonpalpable Breast Lesions