Types and Prevalence of Coexisting Spine Lesions on Whole Spine Sagittal MR Images in Surgical Degenerative Spinal Diseases
- Affiliations
-
- 1Department of Neurosurgery, Pusan National University School of Medicine, Busan, Korea.
- 2Department of Radilogy, Spine and Spinal Cord Institute, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea.
- 3Department of Neurosurgery, Spine and Spinal Cord Institute, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea. spinekks@yuhs.ac
- KMID: 1074994
- DOI: http://doi.org/10.3349/ymj.2010.51.3.414
Abstract
- PURPOSE
We investigated types and prevalence of coexisting lesions found on whole spine sagittal T2-weighted images (WSST2I) acquired from magnetic resonance imaging (MRI) and evaluated their clinical significance in surgical degenerative spinal diseases.
MATERIALS AND METHODS
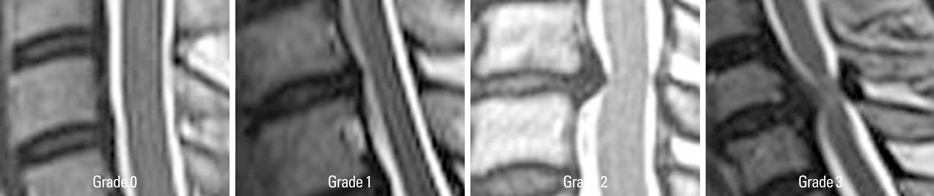
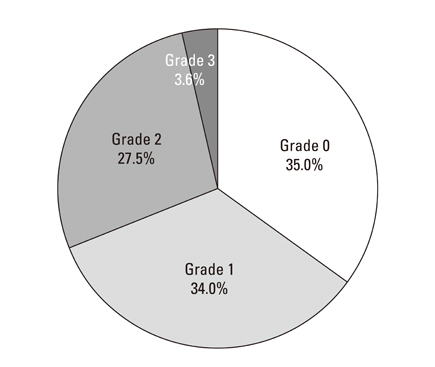
Coexisting spinal lesions were investigated using WSST2I from 306 consecutive patients with surgical degenerative spinal diseases. Severity of coexisting lesions was classified into four grades (0-3). Lesions of grade 2 and 3 were defined as "meaningful coexisting spine lesions" (MCSL). Degenerative spinal diseases were classified into three pathologies: simple disc herniation, degenerative spinal stenosis, and ligament ossification disease. The relationships between MCSL, gender, age, and primary spine lesions were analyzed.
RESULTS
MCSL were found in 95 patients: a prevalence of 31.1%. Five out of 95 MCSL were surgically managed. The most common types of MCSL were disc herniation with 13.1% prevalence, followed by degenerative stenosis (9.5%) and ligament ossification diseases (6.8%). Older patients (age > or = 40) showed a significantly higher prevalence of MCSL than younger patients. There was no significant difference between male and female patients. The prevalence of MCSL was significantly higher (52.4%) in ligament ossification diseases than in disc herniation or spinal stenosis.
CONCLUSION
Degenerative spinal diseases showed a high prevalence of MCSL, especially in old ages and ligament ossification diseases. WSST2I is useful for diagnosing coexisting spinal diseases and to avoid missing a significant cord-compressing lesion.
MeSH Terms
Figure
Cited by 4 articles
-
Coexisting Spine Lesions on Whole Spine T2 Sagittal MRI in Evaluating Spinal Degenerative Disease
Jae Hong Ha, Ji-Ho Lee, Jae Hyup Lee
J Korean Med Sci. 2021;36(7):e48. doi: 10.3346/jkms.2021.36.e48.Lumbar Epidural Steroid Injection for Painful Spasticity in Cervical Spinal Cord Injury: A Case Report
Hyun Bang, Seong Min Chun, Hee Won Park, Moon Suk Bang, Keewon Kim
Ann Rehabil Med. 2015;39(4):649-653. doi: 10.5535/arm.2015.39.4.649.Prevalence, Distribution, and Significance of Incidental Thoracic Ossification of the Ligamentum Flavum in Korean Patients with Back or Leg Pain : MR-Based Cross Sectional Study
Bong Ju Moon, Sung Uk Kuh, Sungjun Kim, Keun Su Kim, Yong Eun Cho, Dong Kyu Chin
J Korean Neurosurg Soc. 2015;58(2):112-118. doi: 10.3340/jkns.2015.58.2.112.Inter- and Intra-Observer Variability of the Volume of Cervical Ossification of the Posterior Longitudinal Ligament Using Medical Image Processing Software
Dong Ah Shin, Gyu Yeul Ji, Chang Hyun Oh, Keung Nyun Kim, Do Heum Yoon, Hyunchul Shin
J Korean Neurosurg Soc. 2017;60(4):441-447. doi: 10.3340/jkns.2015.0708.014.
Reference
-
1. Rajeev K, Panikar D. Dural arteriovenous fistula coexisting with a lumbar lipomeningocele. Case report. J Neurosurg Spine. 2005. 3:386–389.2. Takeuchi A, Miyamoto K, Hosoe H, Shimizu K. Thoracic paraplegia due to missed thoracic compressive lesions after lumbar spinal decompression surgery. Report of three cases. J Neurosurg. 2004. 100:71–74.
Article3. Deem S, Shapiro HM, Marshall LF. Quadriplegia in a patient with cervical spondylosis after thoracolumbar surgery in the prone position. Anesthesiology. 1991. 75:527–528.
Article4. Jacobs B, Ghelman B, Marchisello P. Coexistence of cervical and lumbar disc disease. Spine (Phila Pa 1976). 1990. 15:1261–1264.5. LaBan MM, Green ML. Concurrent (tandem) cervical and lumbar spinal stenosis: a 10-yr review of 54 hospitalized patients. Am J Phys Med Rehabil. 2004. 83:187–190.6. Aydogan M, Ozturk C, Mirzanli C, Karatoprak O, Tezer M, Hamzaoglu A. Treatment approach in tandem (concurrent) cervical and lumbar spinal stenosis. Acta Orthop Belg. 2007. 73:234–237.7. Dagi TF, Tarkington MA, Leech JJ. Tandem lumbar and cervical spinal stenosis. Natural history, prognostic indices, and results after surgical decompression. J Neurosurg. 1987. 66:842–849.8. Epstein NE, Epstein JA, Carras R, Murthy VS, Hyman RA. Coexisting cervical and lumbar spinal stenosis: diagnosis and management. Neurosurgery. 1984. 15:489–496.
Article9. Nakanishi K, Kobayashi M, Nakaguchi K, Kyakuno M, Hashimoto N, Onishi H, et al. Whole-body MRI for detecting metastatic bone tumor: diagnostic value of diffusion-weighted images. Magn Reson Med Sci. 2007. 6:147–155.
Article10. Steinborn MM, Heuck AF, Tiling R, Bruegel M, Gauger L, Reiser MF. Whole-body bone marrow MRI in patients with metastatic disease to the skeletal system. J Comput Assist Tomogr. 1999. 23:123–129.
Article11. Takahashi M, Yamashita Y, Sakamoto Y, Kojima R. Chronic cervical cord compression: clinical significance of increased signal intensity on MR images. Radiology. 1989. 173:219–224.
Article12. Althoff CE, Appel H, Rudwaleit M, Sieper J, Eshed I, Hermann KG. Whole-body MRI as a new screening tool for detecting axial and peripheral manifestations of spondyloarthritis. Ann Rheum Dis. 2007. 66:983–985.
Article13. Green RA, Saifuddin A. Whole spine MRI in the assessment of acute vertebral body trauma. Skeletal Radiol. 2004. 33:129–135.
Article14. Kaila R, Malhi AM, Mahmood B, Saifuddin A. The incidence of multiple level noncontiguous vertebral tuberculosis detected using whole spine MRI. J Spinal Disord Tech. 2007. 20:78–81.15. Ramachandran M, Tsirikos AI, Lee J, Saifuddin A. Whole-spine magnetic resonance imaging in patients with neurofibromatosis type 1 and spinal deformity. J Spinal Disord Tech. 2004. 17:483–491.16. Schmitz A, Jaeger UE, Koenig R, Kandyba J, Wagner UA, Giesecke J, et al. A new MRI technique for imaging scoliosis in the sagittal plane. Eur Spine J. 2001. 10:114–117.
Article17. Schmitz A, Kandyba J, Koenig R, Jaeger UE, Gieseke J, Schmitt O. A new method of MR total spine imaging for showing the brace effect in scoliosis. J Orthop Sci. 2001. 6:316–319.
Article18. Bednarik J, Kadanka Z, Dusek L, Novotny O, Surelova D, Urbanek I, et al. Presymptomatic spondylotic cervical cord compression. Spine (Phila Pa 1976). 2004. 29:2260–2269.19. Teng P, Papatheodorou C. Combined Cervical and Lumbar Spondylosis. Arch Neurol. 1964. 10:298–307.
Article20. Boden SD, Davis DO, Dina TS, Patronas NJ, Wiesel SW. Abnormal magnetic-resonance scans of the lumbar spine in asymptomatic subjects. A prospective investigation. J Bone Joint Surg Am. 1990. 72:403–408.
Article21. Park JY, Chin DK, Kim KS, Cho YE. Thoracic ligament ossification in patients with cervical ossification of the posterior longitudinal ligaments: tandem ossification in the cervical and thoracic spine. Spine (Phila Pa 1976). 2008. 33:E407–E410.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Coexisting Spine Lesions on Whole Spine T2 Sagittal MRI in Evaluating Spinal Degenerative Disease
- Increased Detection Rate of Syringomyelia by Whole Spine Sagittal Magnetic Resonance Images: Based on the Data from Military Conscription of Korean Young Males
- Clinical Relationship of Degenerative Changes between the Cervical and Lumbar Spine
- Spino-Pelvic Parameters in Adult Spinal Deformities
- MR imaging of spondylolisthesis