Korean J Ophthalmol.
2011 Jun;25(3):206-209. 10.3341/kjo.2011.25.3.206.
Conventional Epi-LASIK and Lamellar Epithelial Debridement in Myopic Patients with Dermatologic Keloids
- Affiliations
-
- 1Department of Ophthalmology, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea. sashimi0@naver.com
- KMID: 1010030
- DOI: http://doi.org/10.3341/kjo.2011.25.3.206
Abstract
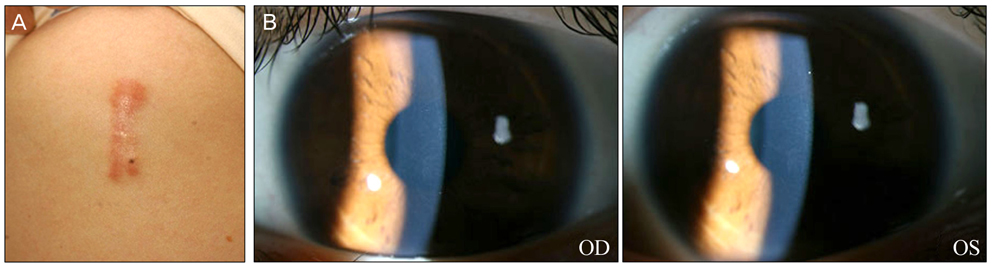
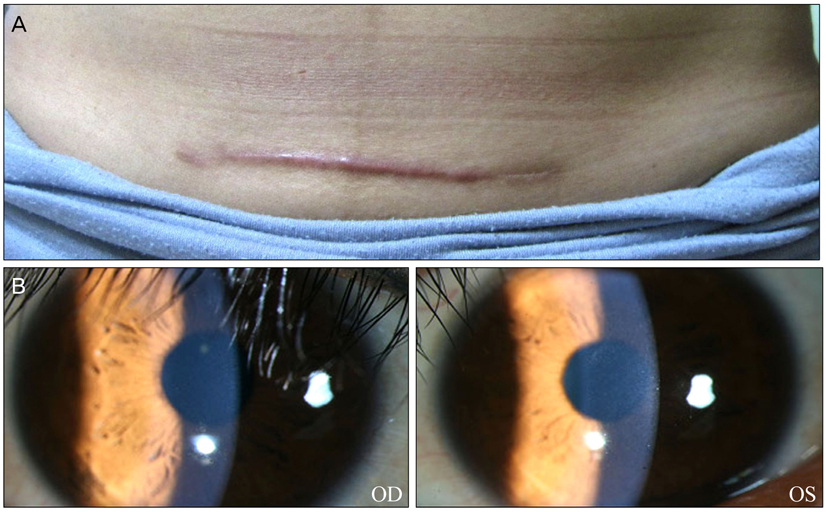
- We report the outcome of conventional epipolis laser in situ keratomileusis (Epi-LASIK, flap-on) and lamellar epithelial debridement (LED; Epi-LASIK, flap-off) in myopic patients with dermatologic keloids. Three patients, who were all noted to be susceptible to keloid scarring, received conventional Epi-LASIK in their right eyes and LED in their left eyes. The patients were followed-up for 6 to 21 months after their surgeries, and the outcomes were then evaluated. In case 1, the preoperative spherical equivalent (SE) was -6.5 diopters (D) in the right eye (OD) and -6.25 D in the left eye (OS). At 21 months postoperatively, the uncorrected visual acuity (UCVA) was 20 / 12.5 in both eyes. In case 2, the preoperative SE was -5.25 (OD) / -6.00 (OS). After six months, the postoperative UCVA was 20 / 12.5 in both eyes. In case 3, the preoperative SE was -4.5 (OD) / -2.0 (OS). The UCVA at the six-month follow-up was 20 / 12.5 in both eyes. No adverse events, including corneal haze, occurred in any of the patients. All three of our patients reported excellent visual outcomes following both conventional Epi-LASIK and LED, despite their histories of keloid formation. The present cases suggest that both Epi-LASIK and LED may be safe and effective techniques for myopic patients with dermatologic keloids.
MeSH Terms
Figure
Reference
-
1. Robles DT, Berg D. Abnormal wound healing: keloids. Clin Dermatol. 2007. 25:26–32.2. Tanzer DJ, Isfahani A, Schallhorn SC, et al. Photorefractive keratectomy in African Americans including those with known dermatologic keloid formation. Am J Ophthalmol. 1998. 126:625–629.3. Cobo-Soriano R, Beltran J, Baviera J. LASIK outcomes in patients with underlying systemic contraindications: a preliminary study. Ophthalmology. 2006. 113:1118.e1–1118.e8.4. Artola A, Gala A, Belda JI, et al. LASIK in myopic patients with dermatological keloids. J Refract Surg. 2006. 22:505–508.5. Girgis R, Morris DS, Kotagiri A, Ramaesh K. Bilateral corneal scarring after LASIK and PRK in a patient with propensity to keloid scar formation. Eye (Lond). 2007. 21:96–97.6. Pallikaris IG, Katsanevaki VJ, Kalyvianaki MI, Naoumidi II. Advances in subepithelial excimer refractive surgery techniques: Epi-LASIK. Curr Opin Ophthalmol. 2003. 14:207–212.7. Wang QM, Fu AC, Yu Y, et al. Clinical investigation of off-flap epi-LASIK for moderate to high myopia. Invest Ophthalmol Vis Sci. 2008. 49:2390–2394.8. Al-Attar A, Mess S, Thomassen JM, et al. Keloid pathogenesis and treatment. Plast Reconstr Surg. 2006. 117:286–300.9. Xia W, Phan TT, Lim IJ, et al. Complex epithelial-mesenchymal interactions modulate transforming growth factor-beta expression in keloid-derived cells. Wound Repair Regen. 2004. 12:546–556.10. Baldwin HC, Marshall J. Growth factors in corneal wound healing following refractive surgery: a review. Acta Ophthalmol Scand. 2002. 80:238–247.11. Kaji Y, Soya K, Amano S, et al. Relation between corneal haze and transforming growth factor-beta1 after photorefractive keratectomy and laser in situ keratomileusis. J Cataract Refract Surg. 2001. 27:1840–1846.12. Katsanevaki VJ, Naoumidi II, Kalyvianaki MI, Pallikaris G. Epi-LASIK: histological findings of separated epithelial sheets 24 hours after treatment. J Refract Surg. 2006. 22:151–154.13. Long Q, Chu R, Zhou X, et al. Correlation between TGF-beta1 in tears and corneal haze following LASEK and epi-LASIK. J Refract Surg. 2006. 22:708–712.14. Akaishi S, Akimoto M, Ogawa R, Hyakusoku H. The relationship between keloid growth pattern and stretching tension: visual analysis using the finite element method. Ann Plast Surg. 2008. 60:445–451.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Short Term Clinical Results of Laser Epithelial Keratomileusis and Epi-Laser in Situ Keratomileusis for Moderate and High Myopia
- Early Postoperative Pain and Visual Outcomes Following Epipolis-Laser In Situ Keratomileusis and Photorefractive Keratectomy
- Comparison of Laser Epithelial Keratomileusis Versus Epipolis-Laser in Situ Keratomileusis for Moderate to High Myopia
- Comparison of Short Term Clinical Results Between Epi-LASIK and Femtosecond LASIK
- Factors Associated with the Successful Separation of Corneal Epithelium in Epi-LASIK