Korean J Ophthalmol.
2010 Jun;24(3):143-147. 10.3341/kjo.2010.24.3.143.
Early Postoperative Pain and Visual Outcomes Following Epipolis-Laser In Situ Keratomileusis and Photorefractive Keratectomy
- Affiliations
-
- 1Department of Ophthalmology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. hwtchah@amc.seoul.kr
- KMID: 945983
- DOI: http://doi.org/10.3341/kjo.2010.24.3.143
Abstract
- PURPOSE
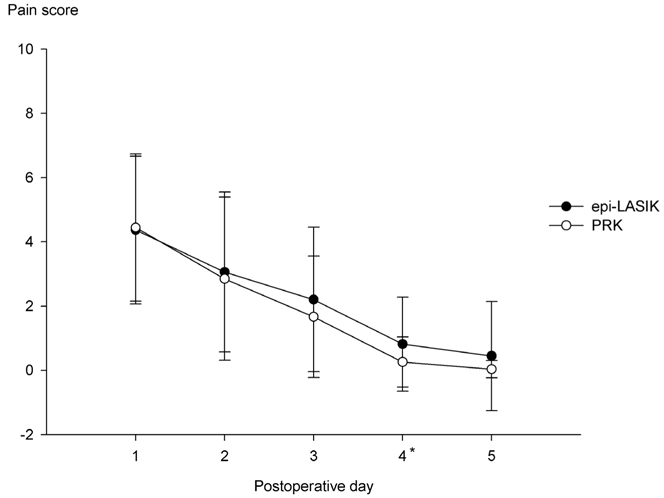
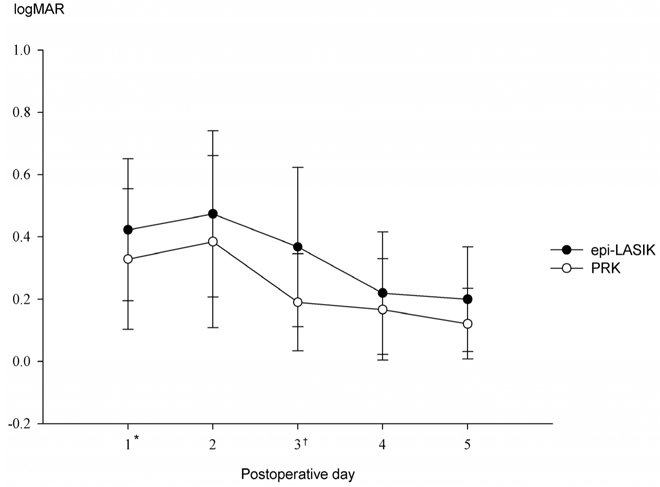
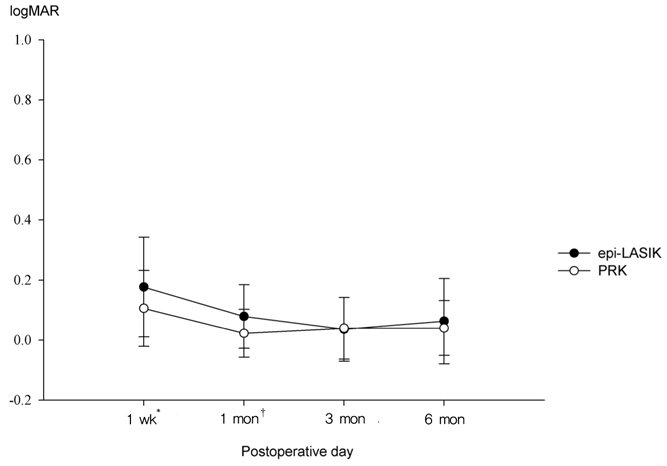
To compare early postoperative pain and visual outcomes after epipolis-laser in situ keratomileusis (epi-LASIK) and photorefractive keratectomy (PRK) in the treatment of myopia. METHODS: A retrospective chart review was designed and included 49 eyes in 30 patients who underwent epi-LASIK and 54 eyes in 29 patients who underwent PRK. During the early postoperative period (days 1 to 5), pain, uncorrected visual acuity (UCVA), and time to epithelial healing were recorded. Visual outcomes were followed for up to six months. RESULTS: Mean preoperative spherical equivalent refraction for the epi-LASIK group was -3.99+/-1.39 diopters (D) and that of the PRK group was -3.54+/-1.27 D. The pain scores on the fourth postoperative day were significantly higher in the epi-LASIK group than in the PRK group (p=0.017). Duration of pain in the epi-LASIK group was longer than in the PRK group (p=0.010). Mean healing time was significantly longer in the epi-LASIK group than in the PRK group (p<0.000). In addition, UCVA in the epi-LASIK group at postoperative days 1 and 3 were significantly lower than those in the PRK group (p=0.021 and p<0.000, respectively). Uncorrected visual acuity at one week and one month after epi-LASIK were lower than those after PRK (p=0.023 and p=0.004, respectively). CONCLUSIONS: In the epi-LASIK patients, pain relief, corneal healing, and visual recovery seemed to be slower during the early postoperative period compared to those of the PRK patients. With longer duration of follow-up, however, there were no significant differences in visual outcome between the two groups.
Keyword
MeSH Terms
Figure
Reference
-
1. Pallikaris IG, Naoumidi II, Kalyvianaki MI, Katsanevaki VJ. Epi-LASIK: comparative histological evaluation of mechanical and alcohol-assisted epithelial separation. J Cataract Refract Surg. 2003. 29:1496–1501.2. Pallikaris IG, Katsanevaki VJ, Kalyvianaki MI, Naoumidi II. Advances in subepithelial excimer refractive surgery techniques: Epi-LASIK. Curr Opin Ophthalmol. 2003. 14:207–212.3. Netto MV, Mohan RR, Ambrosio R Jr, et al. Wound healing in the cornea: a review of refractive surgery complications and new prospects for therapy. Cornea. 2005. 24:509–522.4. Pallikaris IG, Kalyvianaki MI, Katsanevaki VJ, Ginis HS. Epi-LASIK: preliminary clinical results of an alternative surface ablation procedure. J Cataract Refract Surg. 2005. 31:879–885.5. Dai J, Chu R, Zhou X, et al. One-year outcomes of epi-LASIK for myopia. J Refract Surg. 2006. 22:589–595.6. Katsanevaki VJ, Kalyvianaki MI, Kavroulaki DS, Pallikaris IG. One-year clinical results after epi-LASIK for myopia. Ophthalmology. 2007. 114:1111–1117.7. O'Doherty M, Kirwan C, O'Keeffe M, O'Doherty J. Postoperative pain following epi-LASIK, LASEK, and PRK for myopia. J Refract Surg. 2007. 23:133–138.8. Tanioka H, Hieda O, Kawasaki S, et al. Assessment of epithelial integrity and cell viability in epithelial flaps prepared with the epi-LASIK procedure. J Cataract Refract Surg. 2007. 33:1195–1200.9. Nishi Y, Nishi O, Nishi K, Auffarth G. Pain reduction after epi-LASIK with a simple surgical procedure. J Cataract Refract Surg. 2007. 33:555–557.10. Torres LF, Sancho C, Tan B, et al. Early postoperative pain following Epi-LASIK and photorefractive keratectomy: a prospective, comparative, bilateral study. J Refract Surg. 2007. 23:126–132.11. Blake CR, Cervantes-Castaneda RA, Macias-Rodriguez Y, et al. Comparison of postoperative pain in patients following photorefractive keratectomy versus advanced surface ablation. J Cataract Refract Surg. 2005. 31:1314–1319.12. Matsumoto JC, Chu YS. Epi-LASIK update: overview of techniques and patient management. Int Ophthalmol Clin. 2006. 46:105–115.13. Shin SJ, Kim MJ, Park SH, Joo CK. Clinical outcomes of wavefront-guided Epi-LASIK: 6-months follow-up. J Korean Ophthalmol Soc. 2007. 48:642–648.14. Gamaly TO, El Danasoury A, El Maghraby A. A prospective, randomized, contralateral eye comparison of epithelial laser in situ keratomileusis and photorefractive keratectomy in eyes prone to haze. J Refract Surg. 2007. 23:S1015–S1020.15. Hondur A, Bilgihan K, Hasanreisoglu B. A prospective bilateral comparison of epi-LASIK and LASEK for myopia. J Refract Surg. 2008. 24:928–934.16. Katsanevaki VJ, Naoumidi II, Kalyvianaki MI, Pallikaris G. Epi-LASIK: histological findings of separated epithelial sheets 24 hours after treatment. J Refract Surg. 2006. 22:151–154.17. Kollias A, Ulbig MW, Spitzlberger GM, et al. Epi-LASIK using the Amadeus II microkeratome: evaluation of cut quality using light and electron microscopy. J Cataract Refract Surg. 2007. 33:2118–2121.18. Shah S, Sebai Sarhan AR, Doyle SJ, et al. The epithelial flap for photorefractive keratectomy. Br J Ophthalmol. 2001. 85:393–396.19. Alio JL, Rodriguez AE, Mendez MC, Kanellopoulos J. Histopathology of epi-LASIK in eyes with virgin corneas and eyes with previously altered corneas. J Cataract Refract Surg. 2007. 33:1871–1876.20. Camellin M, Wyler D. Epi-LASIK versus epi-LASEK. J Refract Surg. 2008. 24:S57–S63.21. Choi CY, Kim JY, Kim MJ, Tchah H. Transmission electron microscopy study of corneal epithelial flaps following removal using mechanical scraping, alcohol, and epikeratome techniques. J Refract Surg. 2008. 24:667–670.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Photorefractive Keratectomy and Laser Epithelial Keratomileusis for Low to Moderate Myopia
- Comparison in Pain between Photorefractive Keratectomy and Laser In Situ Epithelial Keratomileusis during Intraoperative and Postoperative Period
- The Effect of PRK and LASIK for the Correction of Postkeratoplasty Astigmatism
- Comparision of the Clinical Results in Photorefractive Keratectomy with that in Laser In Situ Keratomileusis for Correction of Moderate Myopia
- Comparison of Laser Epithelial Keratomileusis Versus Epipolis-Laser in Situ Keratomileusis for Moderate to High Myopia