Korean J Ophthalmol.
2011 Feb;25(1):1-7. 10.3341/kjo.2011.25.1.1.
Comparison of Clinical Manifestations between Patients with Ocular Myasthenia Gravis and Generalized Myasthenia Gravis
- Affiliations
-
- 1Department of Ophthalmology, Institute of Vision Research, Yonsei University College of Medicine, Seoul, Korea. yoonjs@yuhs.ac
- KMID: 994404
- DOI: http://doi.org/10.3341/kjo.2011.25.1.1
Abstract
- PURPOSE
To compare the clinical manifestations between patients with ocular myasthenia gravis and those with generalized myasthenia gravis (MG).
METHODS
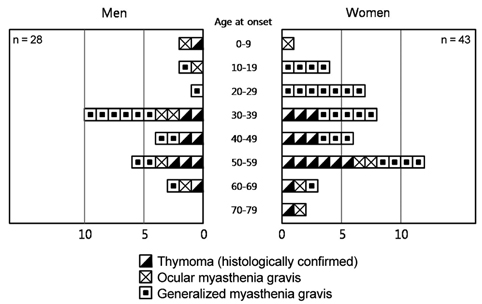
The medical records of 71 patients diagnosed with MG between January 1995 and December 2007 were reviewed. Demographics, sensitivities of diagnostic methods, the presence of systemic autoimmune diseases, ophthalmic complications caused by MG, and treatments were evaluated and compared.
RESULTS
Fourteen patients (20%) were diagnosed with ocular MG and 57 patients (80%) with generalized MG. Sensitivities of anti-acetylcholine receptor antibody and repetitive nerve stimulation tests were significantly higher in the generalized MG group (84%, 89%) compared to those in the ocular MG group (50%, 54%) (p = 0.011, p = 0.008). The sensitivity of the neostigmine test was the highest in both groups (98% of generalized MG, 79% of ocular MG), and the difference between the two groups was borderline significant (p = 0.058). The most common symptoms were ptosis and diplopia, and both groups presented with pain, blurred vision, and tearing. Systemic autoimmune disease was more prominent in the generalized MG group (21%) than in the ocular MG group (14%), and steroid therapy was used more frequently in the generalized MG group (82%) than in the ocular MG group (57%). Ophthalmic complications associated with long-term steroid treatment were more profound in the generalized MG (30%) compared to those of the ocular MG (21%).
CONCLUSIONS
The generalized MG group was associated with higher sensitivities to diagnostic tests, more systemic steroid use, higher ophthalmic complications caused by systemic autoimmune disease, and long-term steroid treatment compared to those of the ocular MG group.
Keyword
MeSH Terms
Figure
Reference
-
1. Kaminski HJ, Maas E, Spiegel P, Ruff RL. Why are eye muscles frequently involved in myasthenia gravis? Neurology. 1990. 40:1663–1669.2. Grob D, Arsura EL, Brunner NG, Namba T. The course of myasthenia gravis and therapies affecting outcome. Ann N Y Acad Sci. 1987. 505:472–499.3. Robertson NP, Deans J, Compston DA. Myasthenia gravis: a population based epidemiological study in Cambridgeshire, England. J Neurol Neurosurg Psychiatry. 1998. 65:492–496.4. Sommer N, Melms A, Weller M, Dichgans J. Ocular myasthenia gravis. A critical review of clinical and pathophysiological aspects. Doc Ophthalmol. 1993. 84:309–333.5. Bever CT Jr, Aquino AV, Penn AS, et al. Prognosis of ocular myasthenia. Ann Neurol. 1983. 14:516–519.6. Kupersmith MJ, Moster M, Bhuiyan S, et al. Beneficial effects of corticosteroids on ocular myasthenia gravis. Arch Neurol. 1996. 53:802–804.7. Sommer N, Sigg B, Melms A, et al. Ocular myasthenia gravis: response to long-term immunosuppressive treatment. J Neurol Neurosurg Psychiatry. 1997. 62:156–162.8. Kupersmith MJ, Latkany R, Homel P. Development of generalized disease at 2 years in patients with ocular myasthenia gravis. Arch Neurol. 2003. 60:243–248.9. Monsul NT, Patwa HS, Knorr AM, et al. The effect of prednisone on the progression from ocular to generalized myasthenia gravis. J Neurol Sci. 2004. 217:131–133.10. Agius MA. Treatment of ocular myasthenia with corticosteroids: yes. Arch Neurol. 2000. 57:750–751.11. Kupersmith MJ. Does early treatment of ocular myasthenia gravis with prednisone reduce progression to generalized disease? J Neurol Sci. 2004. 217:123–124.12. Kupersmith MJ, Ying G. Ocular motor dysfunction and ptosis in ocular myasthenia gravis: effects of treatment. Br J Ophthalmol. 2005. 89:1330–1334.13. Busch C, Machens A, Pichlmeier U, et al. Long-term outcome and quality of life after thymectomy for myasthenia gravis. Ann Surg. 1996. 224:225–232.14. Beekman R, Kuks JB, Oosterhuis HJ. Myasthenia gravis: diagnosis and follow-up of 100 consecutive patients. J Neurol. 1997. 244:112–118.15. Donaldson DH, Ansher M, Horan S, et al. The relationship of age to outcome in myasthenia gravis. Neurology. 1990. 40:786–790.16. Oh SJ, Kim DE, Kuruoglu R, et al. Diagnostic sensitivity of the laboratory tests in myasthenia gravis. Muscle Nerve. 1992. 15:720–724.17. Benatar M. A systematic review of diagnostic studies in myasthenia gravis. Neuromuscul Disord. 2006. 16:459–467.18. Golnik KC, Pena R, Lee AG, Eggenberger ER. An ice test for the diagnosis of myasthenia gravis. Ophthalmology. 1999. 106:1282–1286.19. Hwang SJ, Lee TS, Park BW. The usefulness of ice test for diagnosis of myasthenia gravis in patients with ptosis. J Korean Ophthalmol Soc. 2005. 46:1611–1617.20. Allen JA, Scala S, Jones HR. Ocular myasthenia gravis in a senior population: diagnosis, therapy and prognosis. Muscle Nerve. 2010. 41:379–384.21. Carr AS, Cardwell CR, McCarron PO, McConville J. A systematic review of population based epidemiological studies in myasthenia gravis. BMC Neurol. 2010. 10:46.22. Koves IH, Cameron FJ, Kornberg AJ. Ocular myasthenia gravis and Graves disease in a 10-year-old child. J Child Neurol. 2009. 24:615–617.23. Christensen PB, Jensen TS, Tsiropoulos I, et al. Associated autoimmune diseases in myasthenia gravis. A population-based study. Acta Neurol Scand. 1995. 91:192–195.24. Antonio-Santos AA, Eggenberger ER. Medical treatment options for ocular myasthenia gravis. Curr Opin Ophthalmol. 2008. 19:468–478.25. Díaz-Manera J, Rojas-García R, Illa I. Treatment strategies for myasthenia gravis. Expert Opin Pharmacother. 2009. 10:1329–1342.26. Chirapapaisan N, Tanormrod S, Chuenkongkaew W. Factors associated with insensitivity to pyridostigmine therapy in Thai patients with ocular myasthenia gravis. Asian Pac J Allergy Immunol. 2007. 25:13–16.27. Conti-Fine BM, Milani M, Kaminski HJ. Myasthenia gravis: past, present, and future. J Clin Invest. 2006. 116:2843–2854.28. Mee J, Paine M, Byrne E, et al. Immunotherapy of ocular myasthenia gravis reduces conversion to generalized myasthenia gravis. J Neuroophthalmol. 2003. 23:251–255.29. Tripathi RC, Parapuram SK, Tripathi BJ, et al. Corticosteroids and glaucoma risk. Drugs Aging. 1999. 15:439–450.30. Jobling AI, Augusteyn RC. What causes steroid cataracts? A review of steroid-induced posterior subcapsular cataracts. Clin Exp Optom. 2002. 85:61–75.31. Carvalho-Recchia CA, Yannuzzi LA, Negrão S, et al. Corticosteroids and central serous chorioretinopathy. Ophthalmology. 2002. 109:1834–1837.32. Richman DP, Agius MA. Myasthenia gravis: pathogenesis and treatment. Semin Neurol. 1994. 14:106–110.33. Roberts PF, Venuta F, Rendina E, et al. Thymectomy in the treatment of ocular myasthenia gravis. J Thorac Cardiovasc Surg. 2001. 122:562–568.