Korean J Radiol.
2011 Feb;12(1):59-65. 10.3348/kjr.2011.12.1.59.
CT Imaging Findings of Ruptured Ovarian Endometriotic Cysts: Emphasis on the Differential Diagnosis with Ruptured Ovarian Functional Cysts
- Affiliations
-
- 1Department of Radiology, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul 110-746, Korea. lesiles@chol.com
- KMID: 991683
- DOI: http://doi.org/10.3348/kjr.2011.12.1.59
Abstract
OBJECTIVE
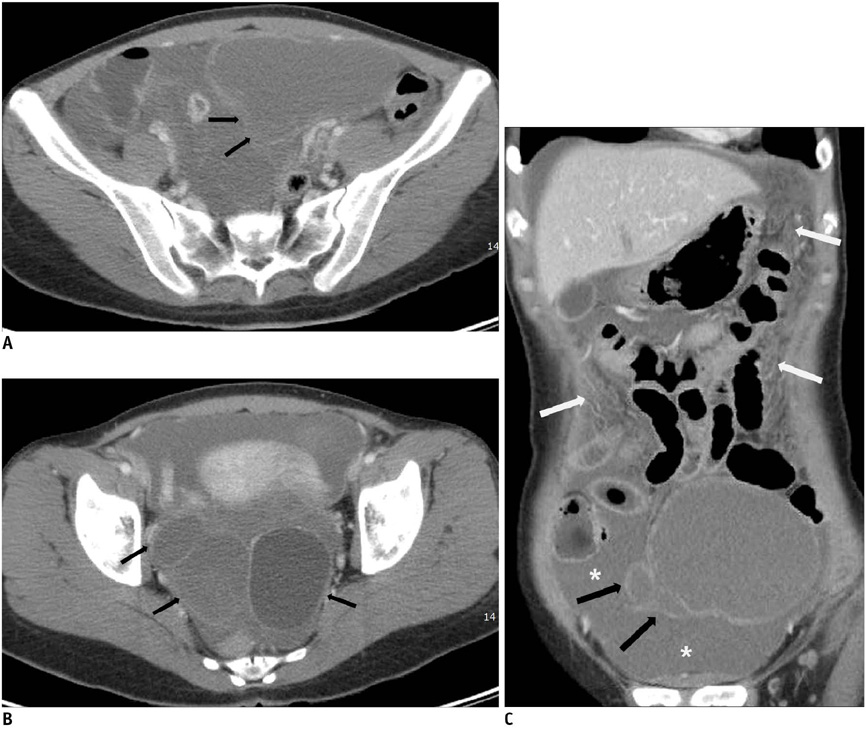
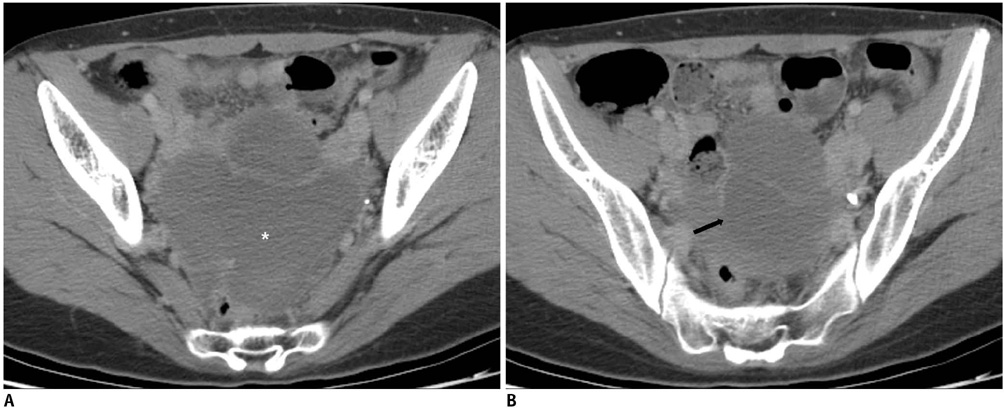
The purpose of this study is to assess the prevalence of abnormal CT findings in patients with surgically proven ruptured endometriotic cysts, as compared with those abnormal CT findings of ruptured ovarian functional cysts.
MATERIALS AND METHODS
This study included 13 retrospectively identified patients with surgically confirmed ruptured ovarian endometriotic cysts and who had also undergone preoperative CT scanning during the previous seven years. As a comparative group, 25 cases of surgically confirmed ruptured ovarian functional cysts were included. We assessed the morphologic features of the cysts and the ancillary findings based on CT.
RESULTS
For the endometriotic cysts, the mean maximum cyst diameter was significantly larger than that of the functional cysts (70.1 mm versus 36.4 mm, respectively, p < 0.05). The endometriotic cysts frequently had a multilocular shape and a thicker cyst wall, as compared to that of functional cysts, and these differences were statistically significant. Among the ancillary findings, endometriotic cysts showed a significantly higher prevalence of loculated ascites, ascites confined to the pelvic cavity without extension to the upper abdomen, and peritoneal strandings and infiltrations (p < 0.05). Although 11 of the 25 cases of functional cysts showed active extravasation of contrast material at the ovarian bleeding site, only one of 13 cases of endometriotic cysts showed active extravasation.
CONCLUSION
The diagnosis of ruptured endometriotic cyst should be suspected for a woman in whom CT reveals the presence of multilocular or bilateral ovarian cysts with a thick wall and loculated ascites confined to the pelvic cavity with pelvic fat infiltrations.
Keyword
MeSH Terms
Figure
Reference
-
1. Lubner M, Menias C, Rucker C, Bhalla S, Peterson CM, Wang L, et al. Blood in the belly: CT findings of hemoperitoneum. Radiographics. 2007. 27:109–125.2. Hertzberg BS, Kliewer MA, Paulson EK. Ovarian cyst rupture causing hemoperitoneum: imaging features and the potential for misdiagnosis. Abdom Imaging. 1999. 24:304–308.3. Hertzberg BS, Kliewer MA, Bowie JD. Adnexal ring sign and hemoperitoneum caused by hemorrhagic ovarian cyst: pitfall in the sonographic diagnosis of ectopic pregnancy. AJR Am J Roentgenol. 1999. 173:1301–1302.4. Bottomley C, Bourne T. Diagnosis and management of ovarian cyst accidents. Best Pract Res Clin Obstet Gynaecol. 2009. 23:711–724.5. Coulier B, Malbecq S, Brinon PE, Ramboux A. MDCT diagnosis of ruptured tubal pregnancy with massive hemoperitoneum. Emerg Radiol. 2008. 15:179–182.6. Swart JE, Fishman EK. Gynecologic pathology on multidetector CT: a pictorial review. Emerg Radiol. 2008. 15:383–389.7. Kinkel K, Frei KA, Balleyguier C, Chapron C. Diagnosis of endometriosis with imaging: a review. Eur Radiol. 2006. 16:285–298.8. Woodward PJ, Sohaey R, Mezzetti TP Jr. Endometriosis: radiologic-pathologic correlation. Radiographics. 2001. 21:193–216.9. Johansson J, Santala M, Kauppila A. Explosive rise of serum CA 125 following the rupture of ovarian endometrioma. Hum Reprod. 1998. 13:3503–3504.10. Evangelinakis N, Grammatikakis I, Salamalekis G, Tziortzioti V, Samaras C, Chrelias C, et al. Prevalence of acute hemoperitoneum in patients with endometriotic ovarian cysts: a 7-year retrospective study. Clin Exp Obstet Gynecol. 2009. 36:254–255.11. Bernstein JP, Perlow V, Brenner JJ. Massive ascites due to endometriosis. Am J Dig Dis. 1961. 6:1–7.12. el-Newihi HM, Antaki JP, Rajan S, Reynolds TB. Large bloody ascites in association with pelvic endometriosis: case report and literature review. Am J Gastroenterol. 1995. 90:632–634.13. Göçmen A, Karaca M, Tarakçioğlu M. A ruptured ovarian endometrioma mimicking ovarian malignancy: case report. Eur J Gynaecol Oncol. 2003. 24:445–446.14. Carbognin G, Guarise A, Minelli L, Vitale I, Malagó R, Zamboni G, et al. Pelvic endometriosis: US and MRI features. Abdom Imaging. 2004. 29:609–618.15. Togashi K, Nishimura K, Kimura I, Tsuda Y, Yamashita K, Shibata T, et al. Endometrial cysts: diagnosis with MR imaging. Radiology. 1991. 180:73–78.16. Kupfer MC, Schwimer SR, Lebovic J. Transvaginal sonographic appearance of endometriomata: spectrum of findings. J Ultrasound Med. 1992. 11:129–133.17. Fishman EK, Scatarige JC, Saksouk FA, Rosenshein NB, Siegelman SS. Computed tomography of endometriosis. J Comput Assist Tomogr. 1983. 7:257–264.18. Umaria N, Olliff JF. Imaging features of pelvic endometriosis. Br J Radiol. 2001. 74:556–562.19. Buy JN, Ghossain MA, Mark AS, Deligne L, Hugol D, Truc JB, et al. Focal hyperdense areas in endometriomas: a characteristic finding on CT. AJR Am J Roentgenol. 1992. 159:769–771.20. Bennett GL, Harvey WB, Slywotzky CM, Birnbaum BA. CT of the acute abdomen: gynecologic etiologies. Abdom Imaging. 2003. 28:416–432.21. Yamashita Y, Torashima M, Hatanaka Y, Harada M, Sakamoto Y, Takahashi M, et al. Value of phase-shift gradient-echo MR imaging in the differentiation of pelvic lesions with high signal intensity at T1-weighted imaging. Radiology. 1994. 191:759–764.22. Ghezzi F, Raio L, Cromi A, Duwe DG, Beretta P, Buttarelli M, et al. "Kissing ovaries": a sonographic sign of moderate to severe endometriosis. Fertil Steril. 2005. 83:143–147.23. Patel MD, Feldstein VA, Chen DC, Lipson SD, Filly RA. Endometriomas: diagnostic performance of US. Radiology. 1999. 210:739–745.24. Borders RJ, Breiman RS, Yeh BM, Qayyum A, Coakley FV. Computed tomography of corpus luteal cysts. J Comput Assist Tomogr. 2004. 28:340–342.25. Ascher SM, Agrawal R, Bis KG, Brown ED, Maximovich A, Markham SM, et al. Endometriosis: appearance and detection with conventional and contrast-enhanced fat-suppressed spin-echo techniques. J Magn Reson Imaging. 1995. 5:251–257.26. Lucey BC, Varghese JC, Anderson SW, Soto JA. Spontaneous hemoperitoneum: a bloody mess. Emerg Radiol. 2007. 14:65–75.