Korean J Radiol.
2000 Jun;1(2):98-103. 10.3348/kjr.2000.1.2.98.
Hypereosinophilic Syndrome : CT Findings in Patients with Hepatic Lobar or Segmental Involvement
- Affiliations
-
- 1Department of Radiology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. jhlim@smc.samsung.co.kr
- KMID: 966480
- DOI: http://doi.org/10.3348/kjr.2000.1.2.98
Abstract
OBJECTIVE
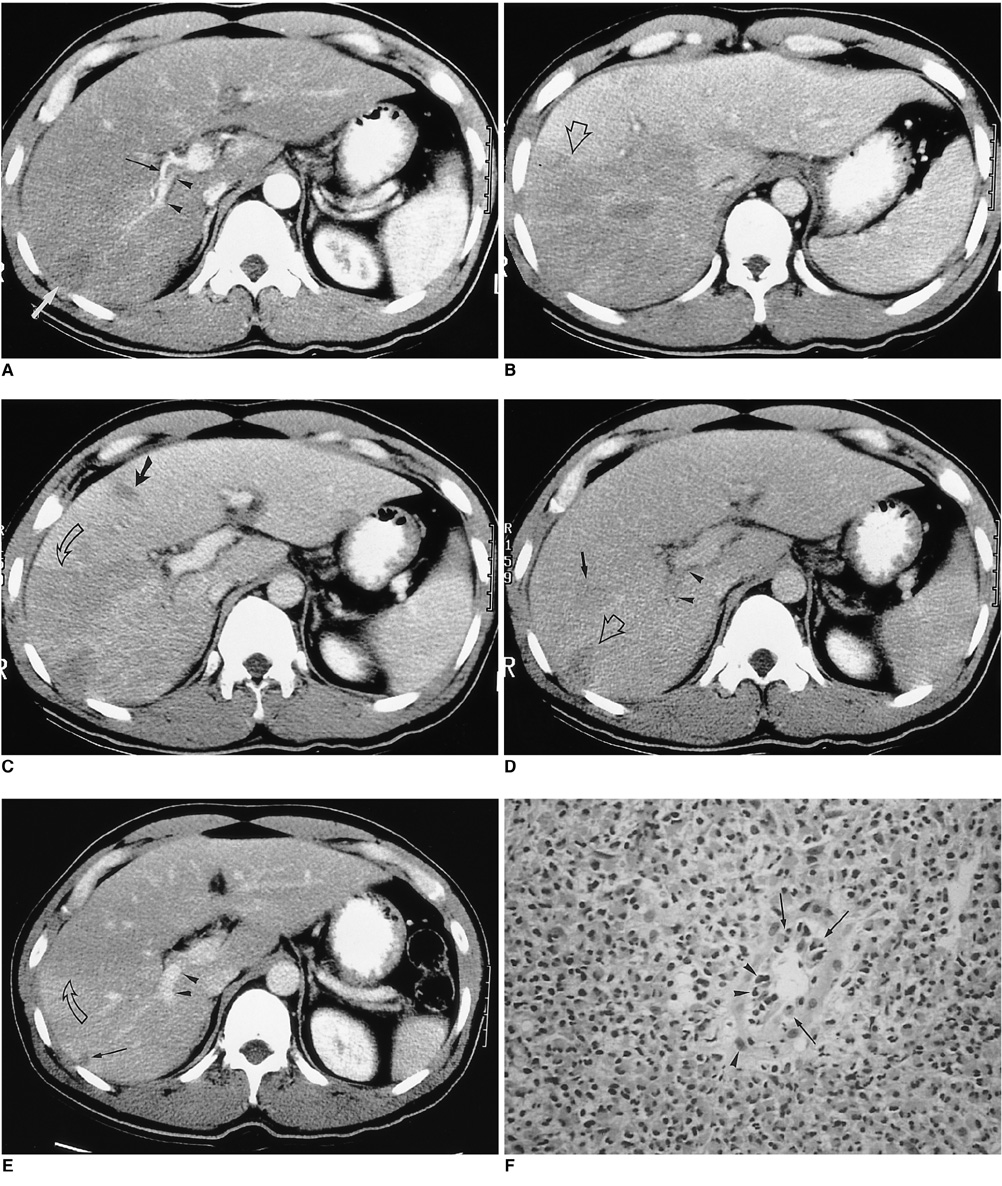
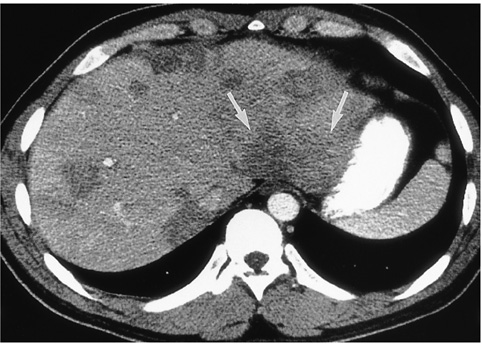
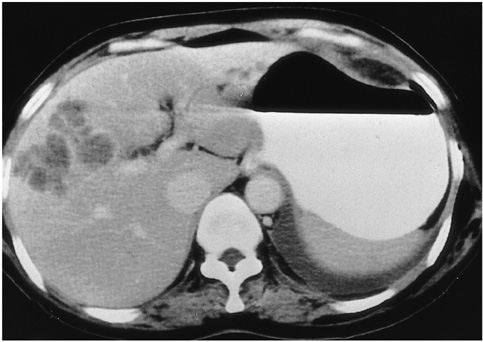
The purpose of this study was to describe the CT findings of hepatic hypereosinophilic syndrome in which hepatic lobes or segments were involved. MATERIALS AND METHODS: Seven patients with hypereosinophilic syndrome with hepatic lobar or segmental involvement were included in our study. In all seven, diagnosis was based on liver biopsy and the results of corticosteroid treatment. CT findings were retrospectively reviewed by three radiologists, who reached a consensus. Biopsy specimens were examined, with special reference to portal and periportal inflammation. RESULTS: CT demonstrated well-defined, homogeneous or heterogeneous low attenuation with a straight margin limited to a hepatic lobe (n = 2), segments (n = 3), or subsegments (n = 2), particularly during the portal phase. Where there was subsegmental involvement, lesions were multiple, ovoid or wedge-shaped, and showed low attenuation. In two patients with lobar or segmental involvement, segmental portal vein narrowing was observed. Histopathologic examination dis-closed eosinophilic infiltration in the periportal area, sinusoids and central veins, as well as portal phlebitis. CONCLUSION: Hypereosinophilic syndrome may involve the presence of hepatic lobar, segmental, or subsegmental low-attenuated lesions, as seen on CT images. Their presence may be related to damage of the liver parenchyma and to portal phlebitis.
Keyword
MeSH Terms
Figure
Reference
-
1. Hardy WR, Anderson RE. The hypereosinophilic syndrome. Ann Intern Med. 1968. 68:1220–1229.2. Fauci AS, Harley JB, Robert WC, Ferrans VJ, Gralnick HR, Bjornson BH. The idiopathic hypereosinophilic syndrome: clinical, pathophysiologic, and therapeutic considerations. Ann Intern Med. 1982. 97:78–92.3. Chusid MJ, Dale DC, West BC, Wolff SM. The hypereosinophilic syndrome: analysis of fourteen cases with review of the literature. Medicine. 1975. 54:1–27.4. Shiomi S, Kuroki T, Ueda T, Ikeoka N, Kobayashi K, Ochi H. Hypereosinophilic syndrome appearing as a focal defect on liver scan. Ann Nucl Med. 1991. 5:171–173.5. White WL, Wahner HW, Brown ML, James EM. Sequential liver imaging in the hypereosinophilic syndrome: discordant images with scintigraphy, ultrasound, and computed tomography. Clin Nucl Med. 1981. 6:75–77.6. Kim GB, Kwon JH, Kang DS. Hypereosinophilic syndrome: imaging findings in patients with hepatic involvement. AJR. 1993. 161:577–580.7. Lee WJ, Lim HK, Lim JH, Kim SH, Choi SH, Lee SJ. Foci of eosinophil-related necrosis in the liver: imaging findings and correlation with eosinophilia. AJR. 1999. 172:1255–1261.8. Cha SH, Park CM, Cha IH, et al. Hepatic involvement in hypereosinophilic syndrome: value of portal venous phase imaging. Abdom Imaging. 1998. 23:154–157.9. Kim KS, Lee M-K, Won YC, et al. Idiopathic hypereosinophilic syndrome involving the liver: CT features vs eosinophilia. J Korean Radiol Soc. 1997. 37:673–677.10. Nam KJ, Jung WJ, Choi J-C, et al. Hepatic involvement in hypereosinophilia: sonographic findings. J Ultrasound Med. 1999. 18:475–479.11. Foong A, Scholes JV, Gleich GJ, Kephart G, Holt PR. Eosinophil-induced chronic active hepatitis in the idiopathic hypereosinophilic syndrome. Hepatology. 1991. 13:1090–1094.12. Croffy BC, Kopelman RK, Kaplan M. Hypereosinophilic syndrome: association with chronic active hepatitis. Dig Dis Sci. 1988. 33:233–239.13. Itai Y, Moss AA, Goldberg HI. Transient hepatic attenuation difference of lobar or segmental distribution detected by dynamic computed tomography. Radiology. 1982. 144:835–839.14. Itai Y, Ohtomo K, Kokubo T, et al. Segmental intensity differences of the liver on MR imaging: a sign of intrahepatic portal flow stoppage. Radiology. 1988. 167:17–19.15. Nishikawa J, Itai Y, Tasaka A. Lobar attenuation differences of the liver on computed tomography. Radiology. 1981. 141:725–728.16. Itai Y, Murata S, Kurosaki Y. Straight border sign of the liver: spectrum of CT appearances and causes. RadioGraphics. 1995. 15:1089–1102.17. Itai Y, Matsui O. Blood flow and liver imaging. Radiology. 1997. 202:306–314.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case of idiopathic hypereosinophilic syndrome presenting as only hepatic involvement
- Hypereosinophilic Syndrome with Hepatic Involvement in a Young Child
- A Case of Hypereosinophilic Syndrome with Hepatic and Gastrointestinal Involvement
- Pulmonary Involvement of Hypereosinophilic Syndrome: High-Resolution CT Findings in Three Patients
- Hypereosinophilic Syndrome with Hepatic Involvement: US, CT and MRI Findings