Korean J Ophthalmol.
2005 Sep;19(3):179-182. 10.3341/kjo.2005.19.3.179.
The Clinical Significance of Venous Filling Time through Panretinal Photocoagulation in Proliferative Diabetic Retinopathy
- Affiliations
-
- 1Department of Ophthalmology, Wonkwang University College of Medicine, Iksan, Jeonbuk, Korea. ysyang@wonkwang.ac.kr
- 2Department of Genome Research Center for Immune Disorders, Wonkwang University College of Medicine, Iksan, Jeonbuk, Korea.
- KMID: 754421
- DOI: http://doi.org/10.3341/kjo.2005.19.3.179
Abstract
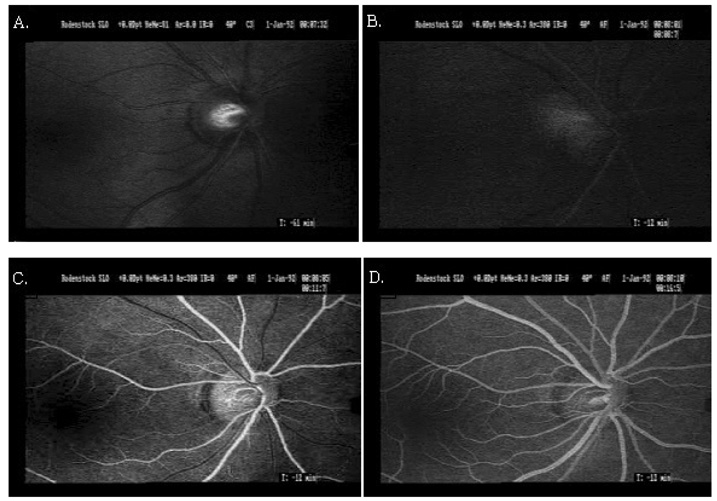
- PURPOSE
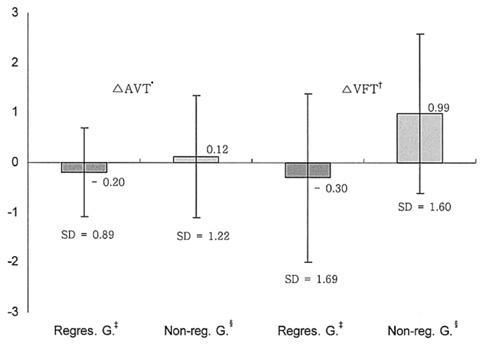
To verify the clinical correlation between retinopathy progression and the change of venous filling time (VFT), measured before and after panretinal photocoagulation (PRP), in proliferative diabetic retinopathy (PDR) patients. METHODS: We conducted this study on 32 patients (32 eyes) who received PRP for PDR. These patients were subdivided into two groups in accordance with the clinical course of PRP: the stabilized group in which retinal neovascularization was regressed and the progressed group in which retinal neovascularization was continued and a complication, such as vitreous hemorrhage or tractional retinal detachment, was developed within 12 months of laser treatment. Arteriovenous passage time (AVP) and VFT were measured by video fluorescein angiogram (FAG) using scanning laser ophthalmoscope (SLO) before and after PRP. VFT values were assigned by measuring by the time duration from start of venous lamina flow to the fullness of fluorescence on the vascular arch. RESULTS: In the stabilized group, AVP was decreased by 0.20+/-0.89sec and VFT was decreased by 0.30+/-1.69 sec through PRP. In the progressed group, AVP was increased in 0.12+/-1.22 sec and VFT was increased by 0.99+/-1.60 sec through PRP. In both groups, the VFT changes were significant (P=0.04) but the AVP changes were not (P=0.34). CONCLUSIONS: VFT was significantly decreased in the stabilized group and significantly increased in the progressed group after PRP. Accordingly, we suggest that VFT changes after PRP can be utilized as a prognostic indicator for evaluating clinical course of diabetic retinopathy after performing PRP and for monitoring the clinical effect of PRP.
Keyword
MeSH Terms
Figure
Reference
-
1. Kohner EM, Oakley NW. Diabetic retinopathy. Metabolism. 1975. 24:1085–1088.2. Frank RW. Ryan ST, Ogden TE, Hinton DR, editors. Etiologic Mechanisms in diabetic retinopathy. Retina. 2001. v. 2:3rd ed. St. Louis: Mosby;chap. 71.3. Harris A, Bingaman DP, Ciulla TA, Martin BJ. Ryan SJ, Ogden TE, Hinton DR, editors. Retina and choroidal blood flow in health and disease. Retina. 2001. v. 1:3rd ed. St. Louis: Mosby;chap. 5.4. Yang YS, Kang PS, Hwang JY, Kim JD. A Study on Microcirculation Time Including Retinal Periphery in Diabetic Retinopathy using the Fluorescein Angiography. J Korean Ophthalmol Soc. 2000. 41:931–937.5. Wolf S, Jung F, Kiesewetter H, et al. Videofluorescein angiography; methods and application. Graefes Arch Clin Exp Ophthalmol. 1989. 227:145–151.6. Kang HR, Yang YS. Comparison of Venous Filling Times and SLO Findings at Each Quadrant Region in Diabetic Retinopathy. Korean J Ophthalmol. 2003. 17:133–139.7. Pae CH, Kim SD, Yang YS. The Comparison of Venous Filling Time Before and After Panretinal Photocoagulation in Proliferative Diabetic Retinopathy. J Korean Ophthalmol Soc. 2003. 44:338–343.8. Jang SS, Yang YS. The Clinical Usefulness of the Venous Filling Time in Proliferative Diabetic retinopathy. J Korean Ophthalmol Soc. 2004. 45:976–981.9. Diabetic Retinopathy Study Research Group. Indications for photocoagulation treatment of diabetic retinopathy: diabetic retinopathy study report No.14. Int Ophthalmol Clin. 1987. 27:239–253.10. Diabetic Retinopathy Study Group. Preliminary report on effects of photocoagulation therapy. Am J Ophthalmol. 1976. 81:383–396.11. Early Treatment Diabetic Retinopathy Study Research Group. Photocoagulation for diabetic macular edema. Arch Ophthalmol. 1985. 193:1796–1806.12. Ferris FL III. How effective is treatment for diabetic retinopathy? JAMA. 1993. 269:1290–1291.13. Wolbarsth ML, Landers MB. The rationale of photocoagulation therapy for proliferative diabetic retinopathy: a review of a model. Ophthalmic Surg. 1980. 11:235–240.14. Galsser BM, Campchiaro PA, Davis JL Jr. Retinal pigment epithelial cells release an inhibitor of neovascularization. Arch Ophthalmol. 1985. 103:1870–1875.15. Woo JH, Heo JW, Yoon HS. The Effect of Panretinal Photocoagulation on Macular Microcirculation in Diabetic Retinopathy(Short term follow up). J Korean Ophthalmol Soc. 1999. 40:1276–1280.16. Blair NP, Feke GT, Morales-Stoppello J, et al. Prolongation of the Retinal Mean Circulation Time in Diabetes. Arch Ophthalmol. 1982. 100:764–768.17. Niki T, Muraoka K, Shimizu K. Distribution of capillary nonperfusion in early stage diabetic retinopathy. Ophthalmology. 1984. 91:1431–1439.18. Lim KH, Lee JH. Study on retinal circulation by Scanning Laser Ophthalmoscope. I. Evaluation of retinal circulation times in Non-proliferative Diabetic Retinopathy. J Korean Ophthalmol Soc. 1995. 36:1133–1136.19. Bertram B, Arend O, Moritz A, et al. Retinal hemodynamics in diabetic retinopathy before and after laser coagulation. Klin Monatsbl Augenheilkd. 1996. 208:152–156.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Comparision of Venous Filling Time Before and After Panretinal Photocoagulation in Proliferative Diabetic Retinopathy
- Changes in Retinal Circulation Time after Panretinal Photocoagulation in Patients with Nonproliferative and Proliferative Diabetic Retinopathy
- The Clinical Usefulness of the Venous Filling Time in Proliferative Diabetic Retinopathy
- The Comparison of Retinal Blood Flow and Foveal Avascular Zone between the Eyes with Panretinal Photocoagulation and the Eyes without PRP using Scanning Laser Ophthalmoscope[SLO] in Diabetic Retinopathy
- Macular Thickness and Visual Acuity Before and After Panretinal Photocoagulation in Severe Diabetic Retinopathy