Korean J Radiol.
2002 Sep;3(3):199-210. 10.3348/kjr.2002.3.3.199.
The Spectrum of Benign Esophageal Lesions: Imaging Findings
- Affiliations
-
- 1Department of Radiology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. kslee@smc.samsung.co.kr
- 2Department of Thoracic Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 754063
- DOI: http://doi.org/10.3348/kjr.2002.3.3.199
Abstract
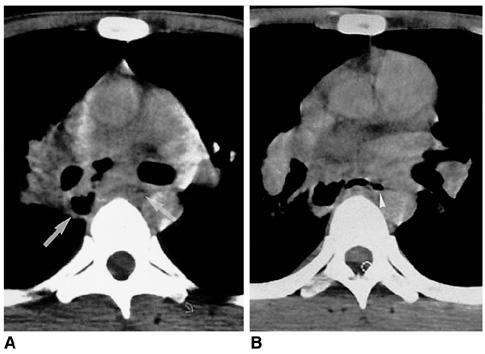
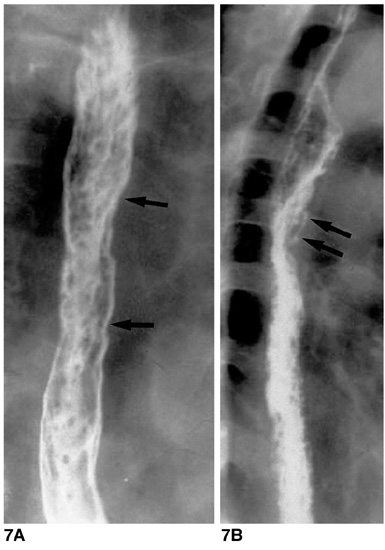
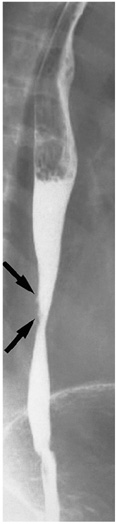
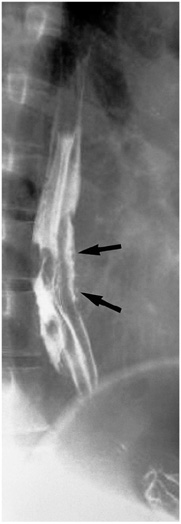
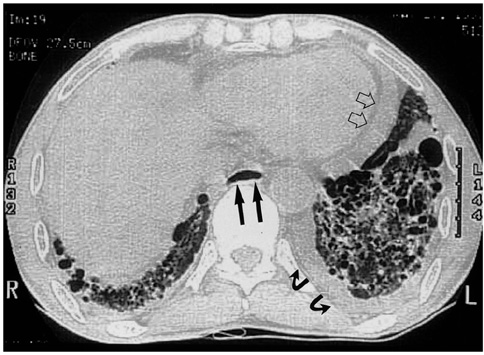
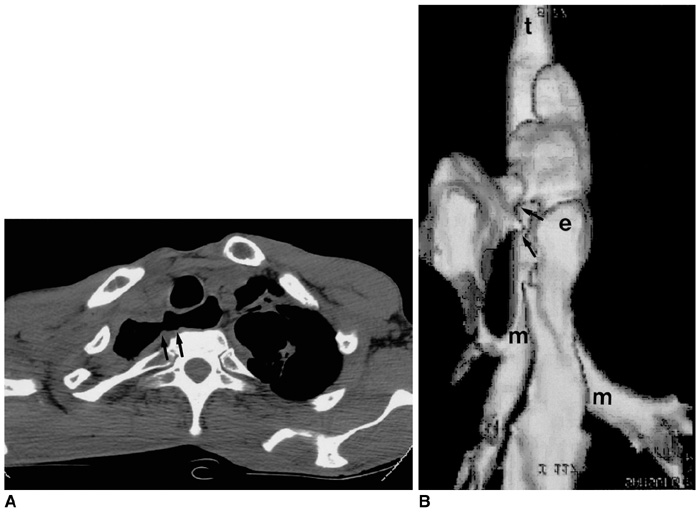
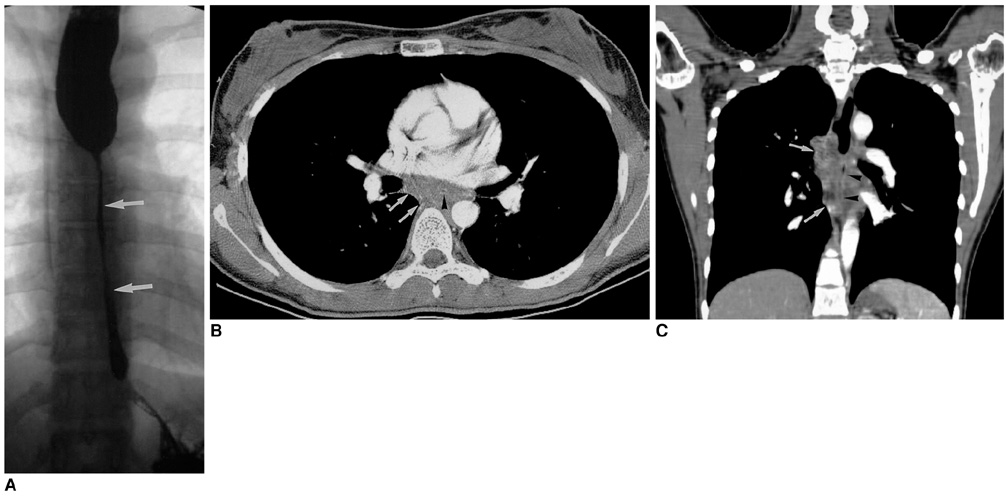
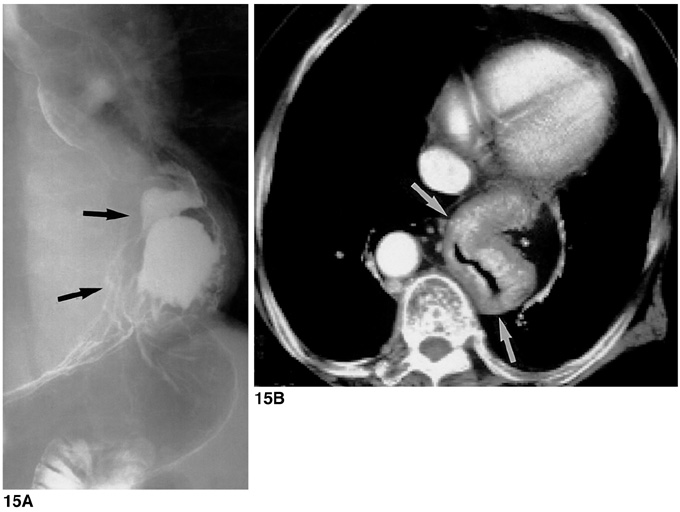
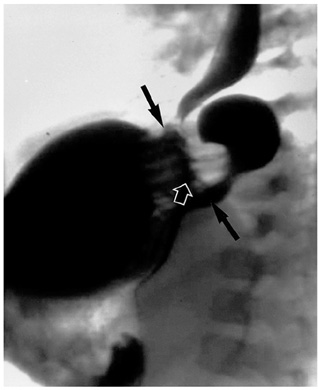
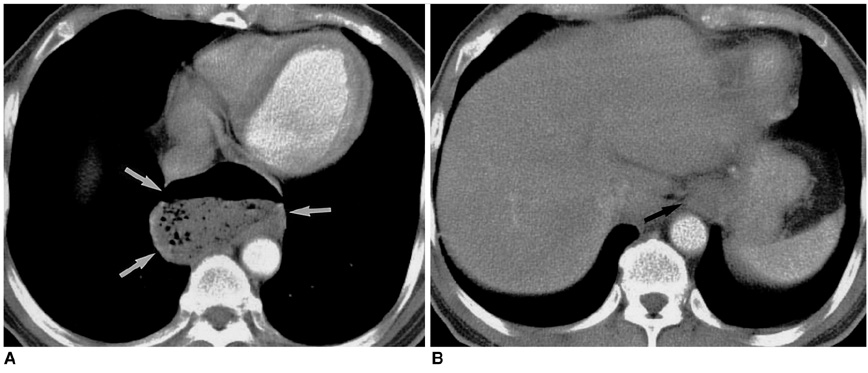
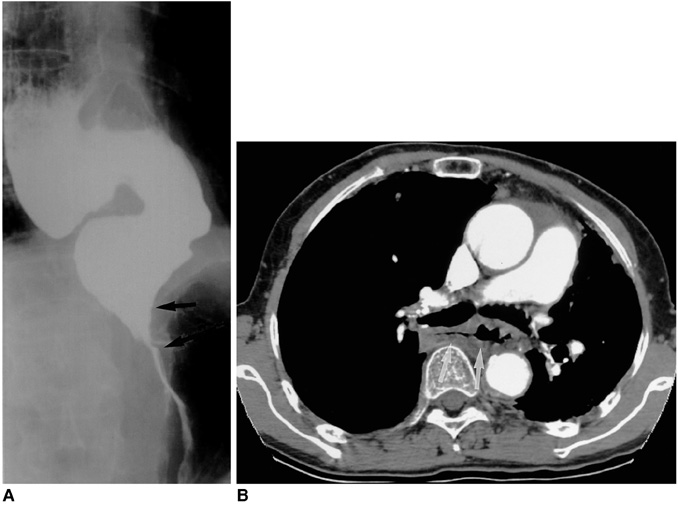
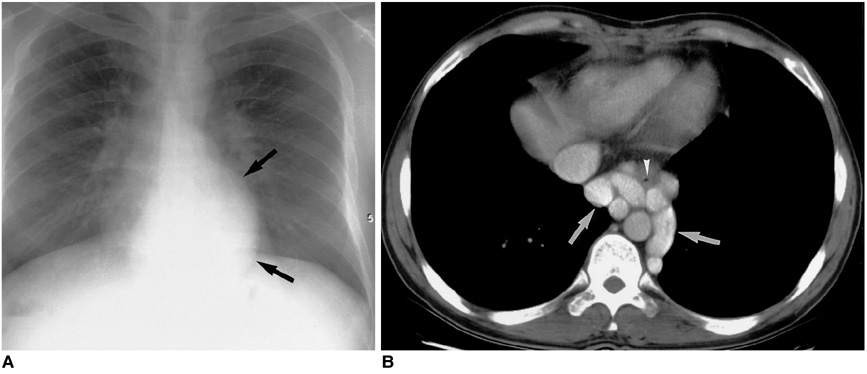
- Benign esophageal lesions occur in various diseases. Barium studies are useful for the evaluation of mucosal surface lesions but provide little information about the extramucosal extent of disease. Computed tomography and magnetic resonance imaging, on the other hand, permit the assessment of wall thickness, mediastinal involvement, adjacent lymphadenopathy, and distant spread. In diseases such as fibrovascular polyps, duplication cysts, scleroderma, trauma, caustic esophagitis, hiatal hernia, esophageal diverticulum, achalasia, and paraesophageal varices, the findings of imaging studies are specific, obviating the need for further invasive diagnostic work-up. The advent of helical computed tomography and its volume data set allows the acquisition of multiplanar images, and magnetic resonance imaging is useful both for this and for tissue characterization. Thus, multiplanar cross-sectional imaging further extends the role of imaging modalities to the evaluation of benign esophageal lesions. Through an awareness of the multiplanar cross-sectional appearances of various benign esophageal lesions, the radiologist can play an important role in the detection, diagnosis, further diagnostic planning, and treatment of the diseases in which they occur.
Keyword
MeSH Terms
Figure
Reference
-
1. Halber MD, Daffner RH, Thompson WM. CT of the esophagus: normal appearance. AJR. 1979. 133:1047–1050.2. Berkovich GY, Levine MS, Miller WT. CT findings in patients with esophagitis. AJR. 2000. 175:1431–1434.3. Seremetis MG, Lyons WS, DeGuzman VC, et al. Leiomyomata of the esophagus: an analysis of 838 cases. Cancer. 1976. 38:2166–2177.4. Cochat P, Guibaud P, Garcia Torres R, Roussel B, Guarner V, Larbre F. Diffuse leiomyomatosis in Alport syndrome. J Pediatr. 1988. 113:339–343.5. Yang PS, Lee KS, Lee SJ, et al. Esophageal leiomyoma: radiologic findings in 12 patients. Korean J Radiol. 2001. 2:132–137.6. Levine MS, Buck JL, Pantongrag-Brown L, Buetow PC, Hallman JR, Sobin LH. Fibrovascular polyps of the esophagus: clinical, radiographic, and pathologic findings in 16 patients. AJR. 1996. 166:781–787.7. Cochet B, Hohl P, Sans M, et al. Asphyxia caused by laryngeal impaction of an esophageal polyp. Arch Otoloaryngol. 1980. 106:176–178.8. Stoane JM, Torrisi JM, Haller JO, David M. Fibrovascular polyps of the esophagus: MRI findings. J Comput Assist Tomogr. 1995. 19:157–159.9. Macpherson RI. Gastrointestinal tract duplications: clinical, pathologic, etiologic, and radiologic considerations. RadioGraphics. 1993. 13:1063–1080.10. Kim YS, Park CK, Choi YW, Jeon SC, Seo HS, Hahm CK. Esophageal tubular duplication complicated by intraluminal hematoma: a case report. J Korean Med Sci. 2000. 15:463–466.11. Kuhlman JE, Fishman EK, Wang KP, Siegelman SS. Esophageal duplication cyst: CT and transesophageal needle aspiration. AJR. 1985. 145:531–532.12. Saito R, Kitamura M, Suzuki H, Ogawa J, Sageshima M. Esophageal schwannoma. Ann Thorac Surg. 2000. 69:1947–1949.13. Ueyama T, Guo KJ, Hashimoto H, Daimaru Y, Enjoji M. Benign schwannoma of the gastrointestinal tract: a clinicopathologic and immunohistochemical study. Hum Pathol. 1988. 19:257–264.14. Im J-G, Kim JH, Han MC, Kim CW. Computed tomography of esophagomediastinal fistula in tuberculous mediastinal lymphadenitis. J Comput Assist Tomogr. 1990. 14:89–92.15. Levine MS, Macones AJ Jr, Laufer I. Candida esophagitis: accuracy of radiographic diagnosis. Radiology. 1985. 154:581–587.16. Vahey TN, Maglinte DD, Chernish SM. State-of-the-art barium examination in opportunistic esophagitis. Dig Dis Sci. 1986. 31:1192–1195.17. Graziani L, De Nigris E, Pesaresi A, Baldelli S, Dini L, Montesi A. Reflux esophagitis: radiologic-endoscopic correlation in 39 symptomatic cases. Gastrointest Radiol. 1983. 8:1–6.18. Laufer I. Radiology of esophagitis. Radiol Clin North Am. 1982. 20:687–699.19. Levine MS. Barrett's esophagus: a radiologic diagnosis? AJR. 1988. 151:433–438.20. Reid BJ. Barrett's esophagus and esophageal adenocarcinoma. Gastroenterol Clin North Am. 1991. 20:817–834.21. Mori S, Yoshihira A, Kawamura H, Takeuchi A, Hashimoto T, Inaba G. Esophageal involvement in Behcet's disease. Am J Gastroenterol. 1983. 78:548–553.22. Bhalla M, Silver RM, Shepard JO, McLoud TC. Chest CT in patients with scleroderma. AJR. 1993. 161:269–272.23. Pasricha PJ, Fleischer DE, Kalloo AN. Endoscopic perforations of the upper digestive tract: a review of their pathogenesis, prevention, and management. Gastroenterology. 1994. 106:787–802.24. Backer CL, LoCicero J, Hartz RS, Donaldson JS, Shields T. Computed tomography in patients with esophageal perforation. Chest. 1990. 98:1078–1080.25. Berkman YM, Auh YH. CT diagnosis of acquired tracheoesophageal fistula in adults. J Comput Assist Tomogr. 1985. 9:302–304.26. Wechsler RJ. CT of esophageal-pleural fistulae. AJR. 1986. 147:907–909.27. Appelqvist P, Salmo M. Lye corrosion carcinoma of the esophagus: a review of 63 cases. Cancer. 1980. 45:2655–2685.28. Lindell MM Jr, Bernardino ME. Diagnosis of hiatus hernia by computed tomography. J Comput Assist Tomogr. 1981. 5:16–19.29. Kim KW, Berkmen YM, Auh YH, Kazam E. Diagnosis of epiphrenic esophageal diverticulum by computed tomography. J Comput Assist Tomogr. 1988. 12:25–28.30. Rabushka LS, Fishman EK, Kuhlman JE. CT evaluation of achalasia. J Comput Assist Tomogr. 1991. 15:434–439.31. Tishler JM, Shin MS, Stanley RJ, Koehler RE. CT of the thorax in patients with achalasia. Dig Dis Sci. 1983. 28:692–697.32. Hirose J, Takashima T, Suzuki M, Matsui O. "Downhill" esophageal varices demonstrated by dynamic computed tomography. J Comput Assist Tomogr. 1984. 8:1007–1009.33. Balthazar EJ, Naidich DP, Megibow AJ, Lefleur RS. CT evaluation of esophageal varices. AJR. 1987. 148:131–135.34. Lee SJ, Lee KS, Kim SA, Kim TS, Hwang JH, Lim JH. Computed radiography of the chest in patients with paraesophageal varices: diagnostic accuracy and characteristic findings. AJR. 1998. 170:1527–1531.