Korean J Radiol.
2002 Sep;3(3):158-162. 10.3348/kjr.2002.3.3.158.
Brain MRI Findings of Carbon Disulfide Poisoning
- Affiliations
-
- 1Department of Radiology, Wonjin Green Hospital, Kangwon-do, Korea. sskim@kangwon.ac.kr
- 2Department of Radiology, Kangwon National University College of Medicine, Kangwon-do, Korea.
- 3Department of Environmental Health, School of Public Health, Seoul National University, Seoul, Korea.
- 4Department of Occupational Medicine, Wonjin Green Hospital, Kangwon-do, Korea.
- 5Department of Family Medicine, Wonjin Green Hospital, Kangwon-do, Korea.
- KMID: 754057
- DOI: http://doi.org/10.3348/kjr.2002.3.3.158
Abstract
OBJECTIVE
To evaluate the findings of brain MRI in patients with carbon disulfide poisoning.
MATERIALS AND METHODS
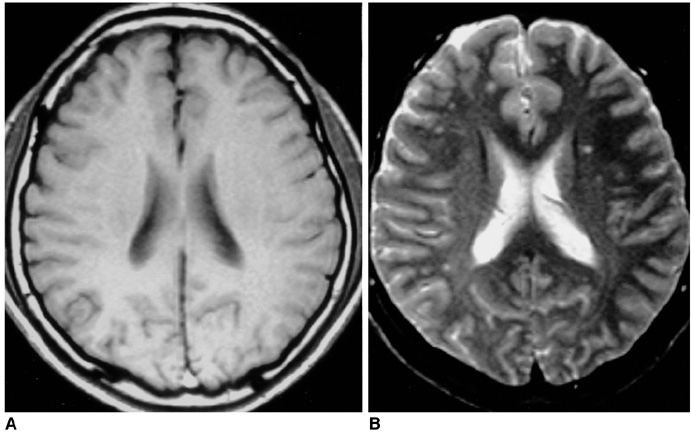
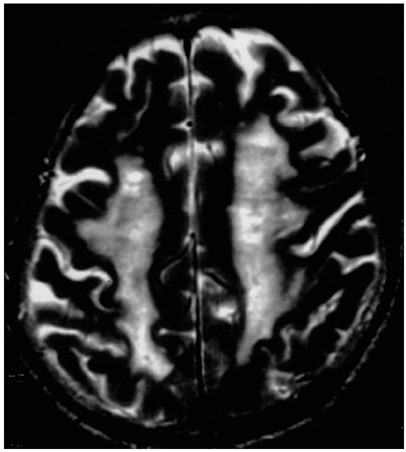
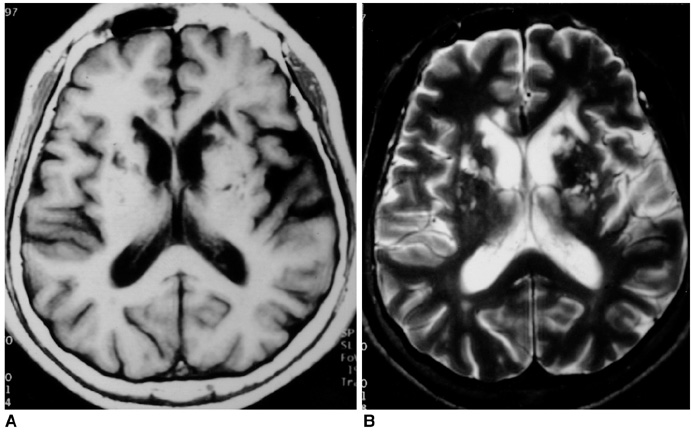
Ninety-one patients who had suffered carbon disulfide poisoning [male:female=87:4; age, 32-74 (mean 53.3) years] were included in this study. To determine the extent of white matter hyperintensity (Grade 0-V) and lacunar infarction, T2-weighted MR imaging of the brain was performed.
RESULTS
T2-weighted images depicted white matter hyperintensity in 70 patients (76.9%) and lacunar infarcts in 27 (29.7%).
CONCLUSION
In these patients, the prevalent findings at T2-weighted MR imaging of the brain were white matter hyperintensity and lacunar infarcts. Disturbance of the cardiovascular system by carbon disulfide might account for these results.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Occupational Neurologic Disorders in Korea
Yangho Kim, Kyoung Sook Jeong, Yong-Hun Yun, Myoung-Soon Oh
J Clin Neurol. 2010;6(2):64-72. doi: 10.3988/jcn.2010.6.2.64.
Reference
-
1. Davidson M, Feinleib M. Carbon disulfide poisoning: A review. Am Heart J. 1972. 83:100–114.2. Lee KB, Byoun HJ, Choi TS, Kim SS, Cho WY, Kim HK. Clinical manifestation of chronic carbon disulfide intoxication. Korean J Int Med. 1990. 39:245–251.3. Choi JW, Jang SH. A review of the carbon disulfide poisoning experience in Korea. Korean J Occup Med. 1991. 3:11–20.4. Yang KS, Choi HR, Kim JJ, et al. Study of carbon disulfide intoxication. 1999. Seoul: Korean Ministry of Labor Press.5. Aaserud O, Gierstad L, Nakstad P, et al. Neurological examination, computerized tomography, cerebral blood flow and neurophysiological examination in workers with long-term exposure to carbon disulfide. Toxicology. 1988. 49:277–282.6. Aaserud O, Hommeren OJ, Tvedt B, et al. Carbon disulfide exposure and neurotoxic sequelae among viscose rayon workers. Am J Ind Med. 1990. 18:25–37.7. Sugimura K, Kabashima K, Tatetsu S. Computerized tomography in chronic carbon disulfide poisoning. No to Shinkei. 1979. 31:1245–1253.8. Huang CC, Chu CC, Chen RS, et al. Chronic carbon disulfide encephalopathy. Eur Neurol. 1996. 36:364–368.9. Peters HA, Levine RL, Matthews CGM, et al. Extrapyramidal and other neurologic manifestations associated with carbon disulfide fumigant exposure. Arch Neurol. 1988. 45:537–540.10. Horikoshi T, Yagi S, Fukamachi A. Incidental high-intensity foci in white matter on T2-weighted magnetic resonance imaging. Neuroradiology. 1993. 35:151–155.11. Wojtczak-Jaroszowa J, Kubow S. Carbon monoxide, carbon disulfide, lead and cadmium-four examples of occupational toxic agents linked to cardiovascular disease. Med Hypotheses. 1989. 30:141–150.12. Awad IA, Spetzler RF, Hodak JA, Awad CA, Carey R. Incidental subcortical lesions identified on magnetic resonance imaging in the elderly: I. Correlation with age and cerebrovascular risk factors. Stroke. 1986. 17:1084–1089.13. Fazekas F. Magnetic resonance signal abnormalities in asymptomatic individuals: their incidental and functional correlates. Eur Neurol. 1989. 29:164–168.14. Hendrie HC, Farlow MR, Austrom MG, Edward MK, Williams MA. Foci of increased T2 signal intensity on brain MR scans of healthy elderly subjects. AJNR. 1989. 10:703–707.15. Yetkin FZ, Fischer ME, Papke RA, Haughton VM. Focal hyperintensities in cerebral white matter on MR images of asymptomatic volunteers: correlation with social and medical histories. AJR. 1993. 161:855–858.16. Gerard G, Weisberg LA. MRI periventricular lesions in adults. Neurology. 1986. 36:998–1001.17. Braffman BH, Zimmerman RA, Trojanowski JQ, Gonatas NK, Hickey WF, Schlaepfer WW. Brain MR: pathologic correlation with gross and histopathology. 2. Hyperintense white-matter foci in the elderly. AJR Am J Roentgenol. 1988. 151:559–566.18. Brant-Zawadzki M, Kucharczk W. Brant-Zawadzki M, Norman D, editors. Vascular disease: ischemia. Magnetic resonance imaging of the central nervous system. 1987. New York: Raven;221–234.19. Lee E, Kim MH. Cerebral vasoreactivity by transcranial Doppler in carbon disulfide poisoning cases in Korea. J Korean Med Sci. 1998. 13:645–651.20. Victor M, Ropper AH. Principles of Neuroradiology. 2001. New York: McGraw-Hill;847–851.21. Fisher CM. Lacunes: small, deep cerebral infarcts. Neurology. 1965. 15:774–784.22. Fisher CM. Lacunar strokes and infarcts: a review. Neurology. 1982. 32:871–896.23. Braffman BH, Zimmerman RA, Trojanowski JQ, Gonatas NK, Hickey WF, Schlaepfer WW. Brian MR: pathologic correlation with gross and histopathology. 1. Lacunar infarction and Virchow-Robin spaces. AJR Am J Roentgenol. 1988. 151:551–558.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A review of the carbon disulfide poisoning experiences in Korean
- Clinical observation on patients with chronic carbon disulfide poisoning
- Health status of workers exposed to carbon disulfide at a viscoserayon factory in Korea
- Clinical Analysis of 8 Cases of Chronic Carbon Disulfide Poisoning in Workers Engaged in the Viscose Rayon Industry
- The study of blood carbon disulfide in rats after oral administration of carbon disulfide