J Rhinol.
2024 Nov;31(3):162-167. 10.18787/jr.2024.00036.
Surgical Timing and Stenting in Neonatal Choanal Atresia
- Affiliations
-
- 1Department of Otorhinolaryngology, Yonsei University College of Medicine, Seoul, Republic of Korea
- 2Department of Otorhinolaryngology, Chung-Ang University College of Medicine, Seoul, Republic of Korea
- KMID: 2561499
- DOI: http://doi.org/10.18787/jr.2024.00036
Abstract
- Background and Objectives
Congenital choanal atresia is a rare condition that occurs in approximately 1 in 7,000 to 8,000 live births and involves the obstruction of the posterior nasal airway. It may present as either unilateral or bilateral, with bilateral cases being more severe due to the risk of immediate neonatal respiratory distress. Bilateral congenital choanal atresia (BCCA) necessitates prompt medical intervention to prevent cyanosis and significant breathing difficulties. This study focuses on the timing of surgery, the duration of stent use, and postoperative care in patients with bilateral congenital choanal atresia who underwent endoscopic transnasal surgery. Unlike previous studies, this research emphasizes the efficacy of an extended stenting period and introduces novel stenting techniques aimed at reducing restenosis.
Methods
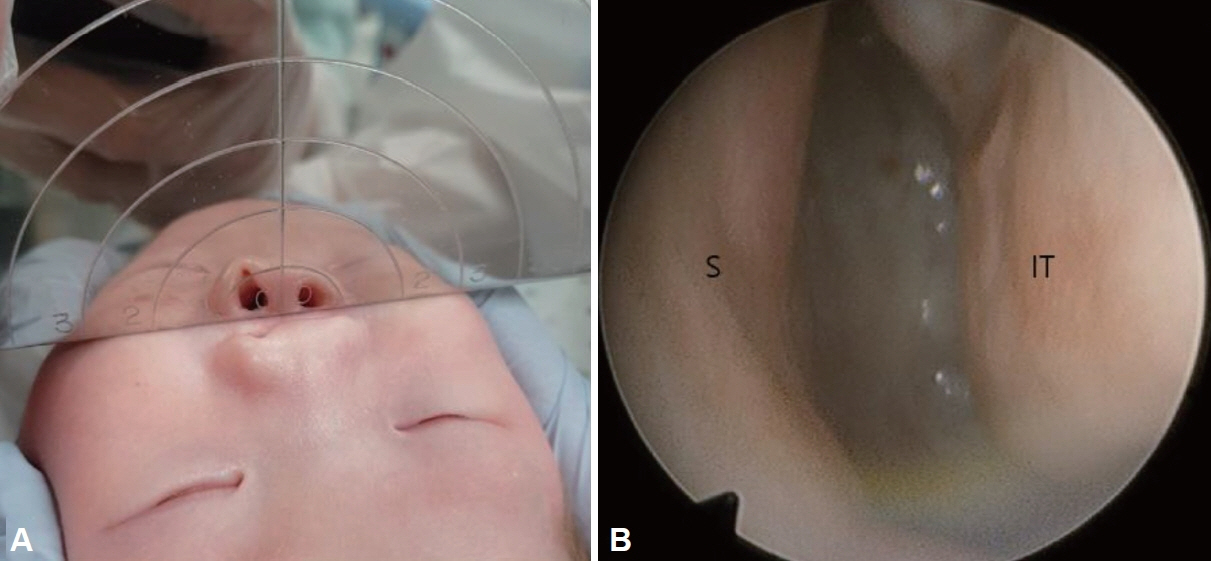
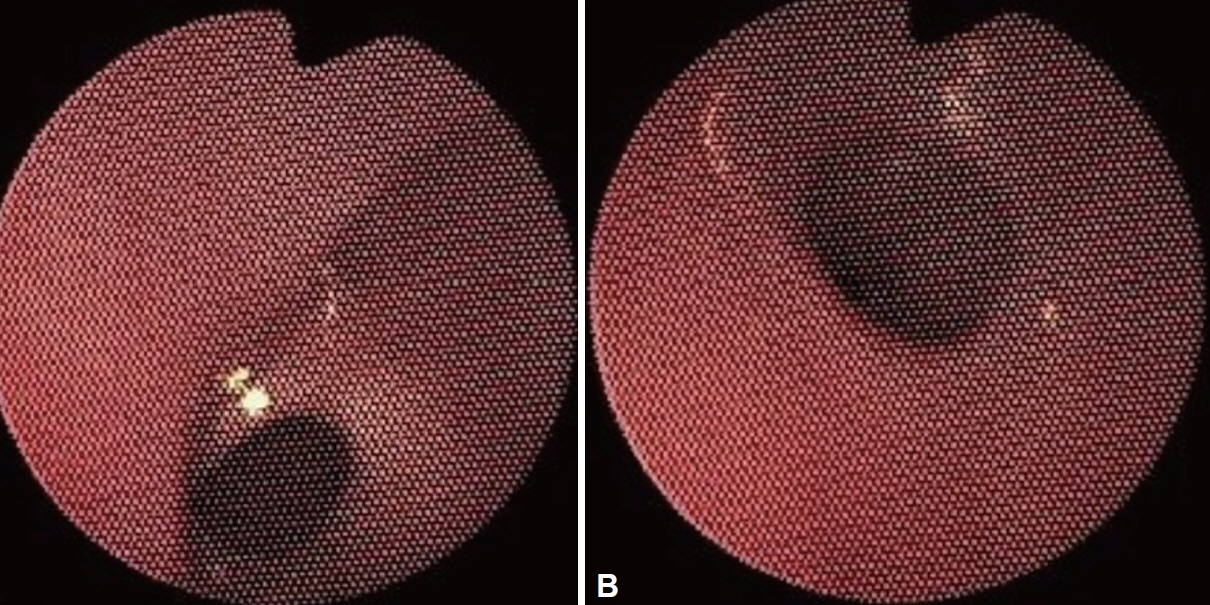
From 2018 to 2021, three patients with BCCA underwent transnasal surgery that included the placement of stents. We retrospectively analyzed their medical records, focusing on the surgical outcomes in relation to the duration of stent placement and postoperative care. A novel approach was adopted, involving the use of customized stent sizes tailored to the specific anatomical factors of each patient, which facilitated improved neochoana maintenance.
Results
The average interval from diagnosis to surgery was 3.6 weeks. Surgery was successful in all cases, and the stent was removed after 6 months. In all patients, stable neochoanae were maintained without significant restenosis. Additionally, we observed that maintaining a stent for a period longer than previously recommended significantly reduced the risk of restenosis compared to the shorter durations used in earlier studies.
Conclusion
Our study suggests that an extended stenting period of 6 months or more is crucial for maintaining long-term patency in patients with BCCA. This approach could lead to a more reliable stenting protocol and improved postoperative care, potentially establishing a new standard for managing BCCA.
Keyword
Figure
Reference
-
References
1. Feuerstein SS, Krespi YP, Sachdev RK. Transnasal correction of choanal atresia. Head Neck Surg. 1980; 3(2):97–104.
Article2. Schoem SR. Transnasal endoscopic repair of choanal atresia: why stent? Otolaryngol Head Neck Surg. 2004; 131(4):362–6.
Article3. Kwong KM. Current updates on choanal atresia. Front Pediatr. 2015; 3:52.
Article4. Hengerer AS, Brickman TM, Jeyakumar A. Choanal atresia: embryologic analysis and evolution of treatment, a 30-year experience. Laryngoscope. 2008; 118(5):862–6.
Article5. Ramsden JD, Campisi P, Forte V. Choanal atresia and choanal stenosis. Otolaryngol Clin North Am. 2009; 42(2):339–52.
Article6. Brown OE, Pownell P, Manning SC. Choanal atresia: a new anatomic classification and clinical management applications. Laryngoscope. 1996; 106(1 Pt 1):97–101.7. Corrales CE, Koltai PJ. Choanal atresia: current concepts and controversies. Curr Opin Otolaryngol Head Neck Surg. 2009; 17(6):466–70.
Article8. Alvo A, Villarroel G, Sedano C. Neonatal nasal obstruction. Eur Arch Otorhinolaryngol. 2021; 278(10):3605–11.
Article9. Rajan R, Tunkel DE. Choanal atresia and other neonatal nasal anomalies. Clin Perinatol. 2018; 45(4):751–67.
Article10. Bedwell J, Shah RK, Bauman N, Zalzal GH, Preciado DA. Balloon dilation for management of choanal atresia and stenosis. Int J Pediatr Otorhinolaryngol. 2011; 75(12):1515–8.
Article11. Diop M, Balakrishnan K. Neonatal nasal obstruction. Curr Otorhinolaryngol Rep. 2021; 9:389–98.
Article12. Gulşen S, Baysal E, Celenk F, Aytaç I, Durucu C, Kanlikama M, et al. Treatment of congenital choanal atresia via transnasal endoscopic method. J Craniofac Surg. 2017; 28(2):338–42.
Article13. Albdah A, Alanbari M, Alwadi F. Choanal atresia repair in pediatric patients: is the use of stents recommended? Cureus. 2019; 11(3):e4206.
Article14. Goudy SL. Diagnosis and management of pediatric ENT conditions. Clin Perinatol. 2018; 45(4):i.
Article15. Mercado P, Eklund JE, Anderson JL. Charge syndrome. In: Lalwani K, Cohen IT, Choi EY, Raman VT, editors. Pediatric anesthesia: a problem- based learning approach. New York: Oxford University Press; 2018. p.19-28.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Congenital Choanal Atresia : Analysis of 7 Cases
- Treatment of Bilateral Choanal Atresia in the Neonate
- A Case of Bilateral Choanal Atresia without Stenting
- SURGICAL REPAIR OF COMPLETE 80NY BILATERAL CHOANAL ATRESIA VIA TRANSPALATAL APPROACH
- A Case of Endoscopic Treatment of Membranous Choanal Atresia with Contralateral Choanal Stenosis Using Powered Instrumentation and Mitomycin C