J Pathol Transl Med.
2024 May;58(3):141-145. 10.4132/jptm.2024.04.12.
Primary epithelioid inflammatory myofibroblastic sarcoma of the brain with EML4::ALK fusion mimicking intra-axial glioma: a case report and brief literature review
- Affiliations
-
- 1Departments of Pathology, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea
- 2Departments of Neurosurgery, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea
- 3Departments of Radiology, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2555540
- DOI: http://doi.org/10.4132/jptm.2024.04.12
Abstract
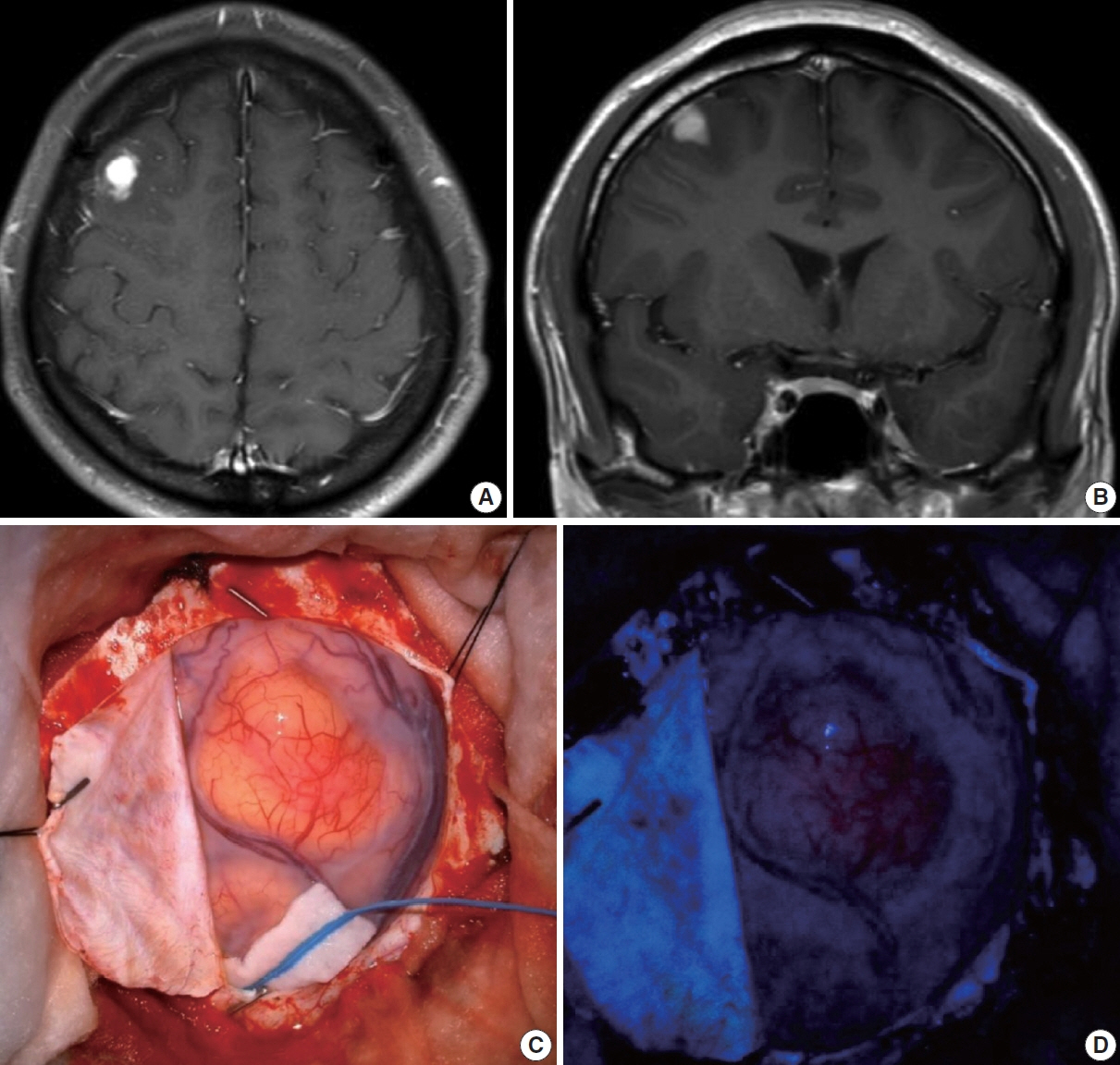
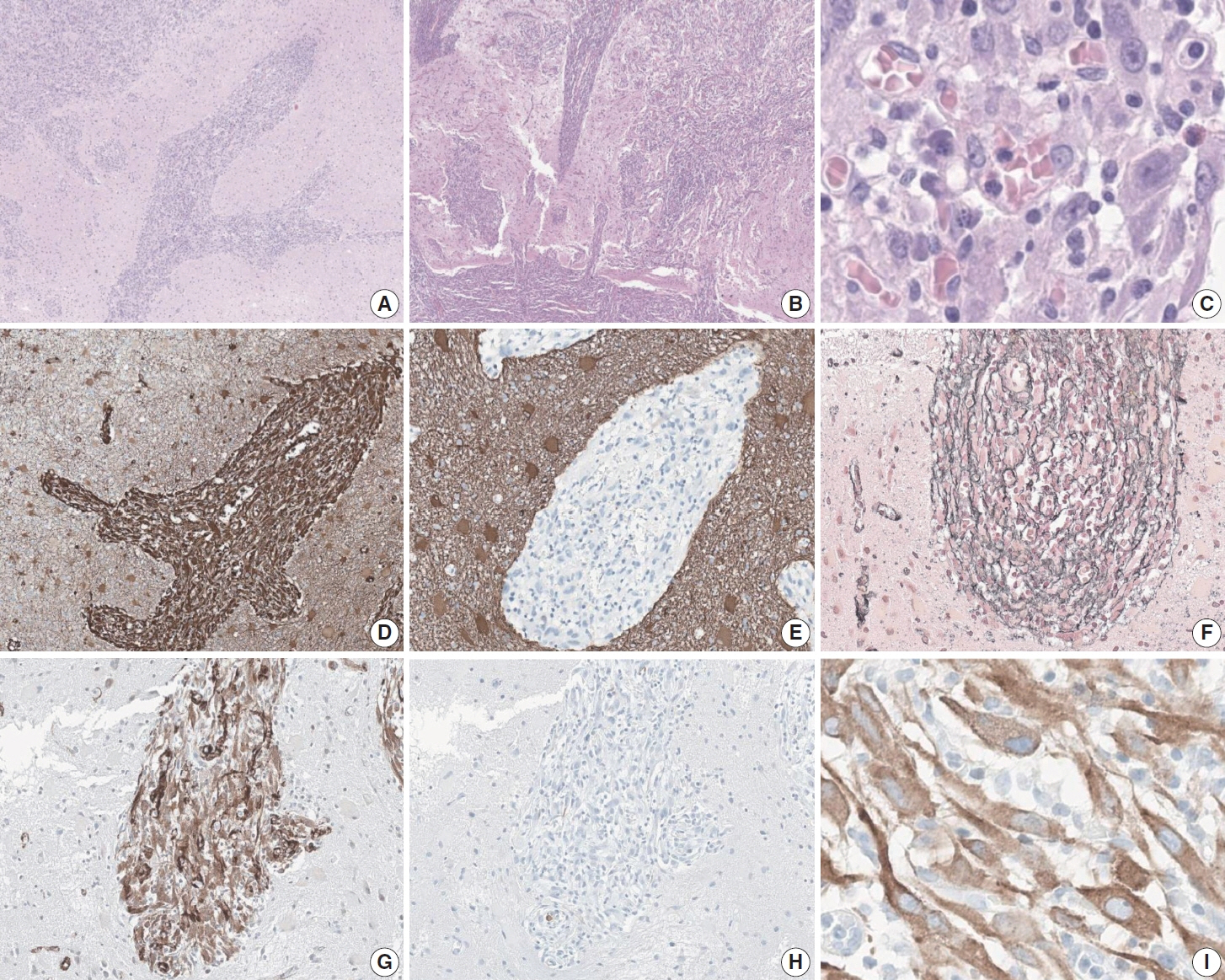
- An aggressive subtype of inflammatory myofibroblastic tumor, epithelioid inflammatory myofibroblastic sarcoma occurs primarily inside the abdominal cavity, followed by a pulmonary localization. Most harbor anaplastic lymphoma kinase (ALK) gene rearrangements, with RANBP2 and RRBP1 among the well-documented fusion partners. We report the second case of primary epithelioid inflammatory myofibroblastic sarcoma of the brain, with a well-known EML4::ALK fusion. The case is notable for its intra-axial presentation that clinico-radiologically mimicked glioma.
Keyword
Figure
Reference
-
References
1. Marino-Enriquez A, Wang WL, Roy A, et al. Epithelioid inflammatory myofibroblastic sarcoma: an aggressive intra-abdominal variant of inflammatory myofibroblastic tumor with nuclear membrane or perinuclear ALK. Am J Surg Pathol. 2011; 35:135–44.2. Coffin CM, Watterson J, Priest JR, Dehner LP. Extrapulmonary inflammatory myofibroblastic tumor (inflammatory pseudotumor): a clinicopathologic and immunohistochemical study of 84 cases. Am J Surg Pathol. 1995; 19:859–72.
Article3. Gleason BC, Hornick JL. Inflammatory myofibroblastic tumours: where are we now? J Clin Pathol. 2008; 61:428–37.
Article4. Chopra S, Maloney N, Wang WL. Epithelioid inflammatory myofibroblastic sarcoma with VCL-ALK fusion of central nervous system: case report and brief review of the literature. Brain Tumor Pathol. 2022; 39:35–42.
Article5. WHO Classification of Tumors Editorial Board. WHO classification of tumours: central nervous system tumours. 5th ed. Lyon: International Agency for Research on Cancer;2021.6. Yu L, Liu J, Lao IW, Luo Z, Wang J. Epithelioid inflammatory myofibroblastic sarcoma: a clinicopathological, immunohistochemical and molecular cytogenetic analysis of five additional cases and review of the literature. Diagn Pathol. 2016; 11:67.
Article7. Lee JC, Li CF, Huang HY, et al. ALK oncoproteins in atypical inflammatory myofibroblastic tumours: novel RRBP1-ALK fusions in epithelioid inflammatory myofibroblastic sarcoma. J Pathol. 2017; 241:316–23.
Article8. Singh P, Nambirajan A, Gaur MK, et al. Primary pulmonary epithelioid inflammatory myofibroblastic sarcoma: a rare entity and a literature review. J Pathol Transl Med. 2022; 56:231–7.
Article9. Yamamoto H, Yoshida A, Taguchi K, et al. ALK, ROS1 and NTRK3 gene rearrangements in inflammatory myofibroblastic tumours. Histopathology. 2016; 69:72–83.
Article10. Drilon A, Laetsch TW, Kummar S, et al. Efficacy of larotrectinib in TRK fusion-positive cancers in adults and children. N Engl J Med. 2018; 378:731–9.11. Lovly CM, Gupta A, Lipson D, et al. Inflammatory myofibroblastic tumors harbor multiple potentially actionable kinase fusions. Cancer Discov. 2014; 4:889–95.
Article12. Sokai A, Enaka M, Sokai R, et al. Pulmonary inflammatory myofibroblastic tumor harboring EML4-ALK fusion gene. Jpn J Clin Oncol. 2014; 44:93–6.
Article13. Jiang Q, Tong HX, Hou YY, et al. Identification of EML4-ALK as an alternative fusion gene in epithelioid inflammatory myofibroblastic sarcoma. Orphanet J Rare Dis. 2017; 12:97.
Article14. Fletcher CD, Bridge JA, Hogendoorn PC, Mertens F. WHO classification of tumours of soft tissue and bone. 4th ed. Lyon: IARC Press;2013.15. WHO Classification of Tumors Editorial Board. WHO classification of tumours: breast tumours. 5th ed. Lyon: International Agency for Research on Cancer;2019.16. Zhou L, Pan W, Huang R, Lu Z, You Z, Li Y. Intracranial inflammatory myofibroblastic tumor: a literature review and a rare case misdiagnosed as acoustic neuroma. Diagnostics (Basel). 2023; 13:2725.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Primary pulmonary epithelioid inflammatory myofibroblastic sarcoma: a rare entity and a literature review
- A case of epithelioid sarcoma arising in the vulva
- EML4-ALK Fusion Gene in Korean Non-Small Cell Lung Cancer
- A Case of Simultaneously Diagnosed Lung Adenocarcinoma and Endobronchial Inflammatory Myofibroblastic Tumor with Two Distinct Types of ALK Translocation
- A Case of Epithelioid Sarcoma in a Child