J Korean Med Sci.
2024 Apr;39(12):e130. 10.3346/jkms.2024.39.e130.
Social Inequities in the Survival of Liver Cancer: A Nationwide Cohort Study in Korea, 2007–2017
- Affiliations
-
- 1Department of Preventive Medicine, College of Medicine, School of Medicine, Kangwon National University, Chuncheon, Korea
- 2Department of Preventive Medicine, College of Medicine, Korea University, Seoul, Korea
- 3Department of Internal Medicine, Kangwon National University Hospital, Kangwon National University School of Medicine, Chuncheon, Korea
- 4BK21FOUR R&E Center for Learning Health Systems, Korea University, Seoul, Korea
- 5Department of Nursing, College of Nursing, Kangwon National University, Chuncheon, Korea
- 6Wonjin Institute for Occupational & Environmental Health, Seoul, Korea
- 7National Cancer Center, Goyang, Korea
- 8Graduate School of Public Health, Seoul National University, Seoul, Korea
- KMID: 2554217
- DOI: http://doi.org/10.3346/jkms.2024.39.e130
Abstract
- Background
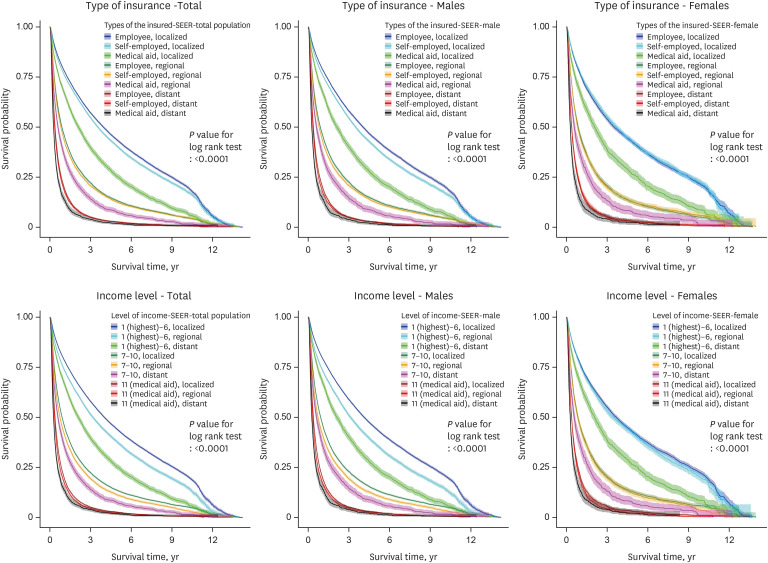
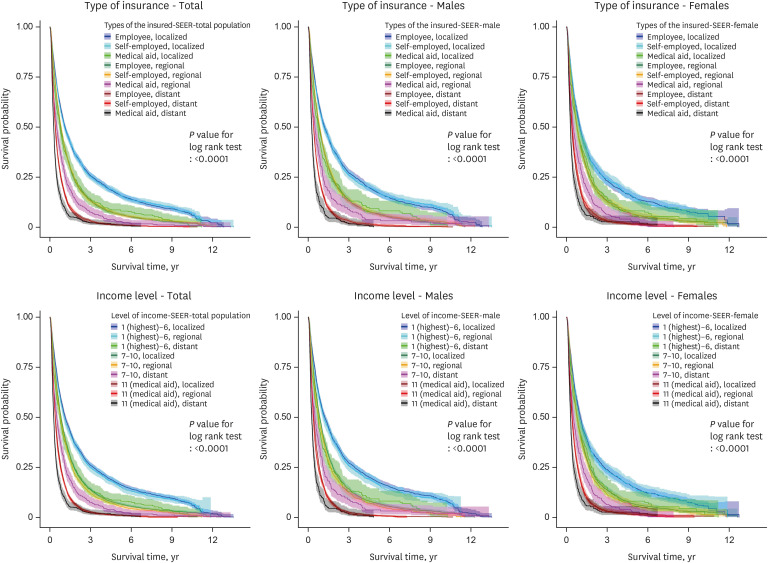
To analyze the effects of socioeconomic status (type of insurance and income level) and cancer stage on the survival of patients with liver cancer in Korea.
Methods
A retrospective cohort study was constructed using data from the Healthcare Big Data Platform project in Korea between January 1, 2007, and December 31, 2017. A total of 143,511 patients in Korea diagnosed with liver cancer (International Classification of Diseases, 10th Revision [ICD-10] codes C22, C220, and C221) were followed for an average of 11 years. Of these, 110,443 died. The patient’s insurance type and income level were used as indicators of socioeconomic status. Unadjusted and adjusted hazard ratios (HRs) and 95% confidence intervals (CIs) were calculated using a Cox proportional hazards regression model to analyze the relationship between the effects of sex, age, and cancer stage at first diagnosis (Surveillance, Epidemiology, and the End Results; SEER), type of insurance, and income level on the survival of patients with liver cancer. The interactive effects of the type of insurance, income level, and cancer stage on liver cancer death were also analyzed.
Results
The lowest income group (medical aid) showed a higher risk for mortality (HR (95% CI); 1.37 (1.27–1.47) for all patients, 1.44 (1.32–1.57) for men, and 1.16 (1.01–1.34) for women) compared to the highest income group (1–6) among liver cancer (ICD-10 code C22) patients. The risk of liver cancer death was also higher in the lowest income group with a distant cancer stage (SEER = 7) diagnosis than for any other group.
Conclusion
Liver cancer patients with lower socioeconomic status and more severe cancer stages were at greater risk of death. Reducing social inequalities is needed to improve mortality rates among patients in lower social class groups who present with advanced cancer.
Keyword
Figure
Reference
-
1. International Cancer Research Institute, Seoul National University. Updated 2020. Accessed December 31, 2020. https://cri.snu.ac.kr/en/about/greetings .2. Son M, Kim S, Lee JH, Kim J, Bae S, Oh JH, et al. Reducing Inequalities in Cancer Incidence and Mortality: Developing Epidemiologic Health Inequality Index and Health Policy in Korea. Report of National Cancer Center: 0720340. Sejong, Korea: Ministry of Health and Welfare;2007.3. Kim CW, Lee SY, Moon OR. Inequalities in cancer incidence and mortality across income groups and policy implications in South Korea. Public Health. 2008; 122(3):229–236. PMID: 17935744.4. Joshi S, Song YM, Kim TH, Cho SI. Socio-economic status and the risk of liver cancer mortality: a prospective study in Korean men. Public Health. 2008; 122(11):1144–1151. PMID: 18793784.5. Artinyan A, Mailey B, Sanchez-Luege N, Khalili J, Sun CL, Bhatia S, et al. Race, ethnicity, and socioeconomic status influence the survival of patients with hepatocellular carcinoma in the United States. Cancer. 2010; 116(5):1367–1377. PMID: 20101732.6. Yun EH, Lim MK, Oh JK, Park JH, Shin A, Sung J, et al. Combined effect of socioeconomic status, viral hepatitis, and lifestyles on hepatocelluar carcinoma risk in Korea. Br J Cancer. 2010; 103(5):741–746. PMID: 20648009.7. Jembere N, Campitelli MA, Sherman M, Feld JJ, Lou W, Peacock S, et al. Influence of socioeconomic status on survival of hepatocellular carcinoma in the Ontario population; a population-based study, 1990-2009. PLoS One. 2012; 7(7):e40917. PMID: 22808283.8. Yim J, Hwang SS, Yoo KY, Kim CY. Contribution of income-related inequality and healthcare utilisation to survival in cancers of the lung, liver, stomach and colon. J Epidemiol Community Health. 2012; 66(1):37–40. PMID: 20961877.9. Singh GK, Jemal A. Socioeconomic and racial/ethnic disparities in cancer mortality, incidence, and survival in the United States, 1950-2014: over six decades of changing patterns and widening inequalities. J Environ Public Health. 2017; 2017:2819372. PMID: 28408935.10. Kim YA, Kang D, Moon H, Sinn D, Kang M, Woo SM, et al. Survival in untreated hepatocellular carcinoma: a national cohort study. PLoS One. 2021; 16(2):e0246143. PMID: 33539397.11. Adler Jaffe S, Myers O, Meisner AL, Wiggins CL, Hill DA, McDougall JA. Relationship between insurance type at diagnosis and hepatocellular carcinoma survival. Cancer Epidemiol Biomarkers Prev. 2020; 29(2):300–307. PMID: 31796525.12. Kronenfeld JP, Ryon EL, Goldberg D, Lee RM, Yopp A, Wang A, et al. Survival inequity in vulnerable populations with early-stage hepatocellular carcinoma: a United States safety-net collaborative analysis. HPB. 2021; 23(6):868–876. PMID: 33487553.13. Spadea T, D’Errico A, Demaria M, Faggiano F, Pasian S, Zanetti R, et al. Educational inequalities in cancer incidence in Turin, Italy. Eur J Cancer Prev. 2009; 18(3):169–178. PMID: 19190494.14. Poulson MR, Blanco BA, Geary AD, Kenzik KM, McAneny DB, Tseng JF, et al. The role of racial segregation in treatment and outcomes among patients with hepatocellular carcinoma. HPB. 2021; 23(6):854–860. PMID: 33536151.15. The Healthcare Big Data Platform project, which was initiated by the Korea Health Industry Development Institute and the Ministry of Health and Welfare in Korea. Accessed April 28, 2023. https://hcdl.mohw.go.kr .16. The Korea National Cancer Incidence (KNCI) database from the Korea Central Cancer Registry (KCCR), the National Cancer Center (NCC). Accessed June 30, 2019. https://www.ncc.re.kr/main.ncc?uri=english/sub04_Introduction .17. The National Health Insurance Sharing Service (NHISS). Accessed June 30, 2019. https://nhiss.nhis.or.kr/bd/ay/bdaya001iv.do .18. The Health Insurance Review & Assessment Service (HIRA). Accessed June 30, 2019. https://www.hira.or.kr/main.do .19. National Institutes of Health, U.S. Department of Health and Human Services. USA.gov. National Cancer Institute SEER training modules. Accessed December 31, 2019. https://training.seer.cancer.gov/modules_site_spec.html .20. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987; 40(5):373–383. PMID: 3558716.21. Health Insurance Review and Assessment Service. Building data for analysis of comorbidities. Updated 2019. Accessed December 31, 2019. https://repository.hira.or.kr/handle/2019.oak/2067 .22. Yun SC. Imputation of missing values. J Prev Med Public Health. 2004; 37(3):209–211. PMID: 25175463.23. Ji J, Hemminki K. Variation in the risk for liver and gallbladder cancers in socioeconomic and occupational groups in Sweden with etiological implications. Int Arch Occup Environ Health. 2005; 78(8):641–649. PMID: 16001211.24. Menvielle G, Kunst AE, Stirbu I, Borrell C, Bopp M, Regidor E, et al. Socioeconomic inequalities in alcohol related cancer mortality among men: to what extent do they differ between Western European populations? Int J Cancer. 2007; 121(3):649–655. PMID: 17415714.25. Korean Liver Cancer Association (KLCA). National Cancer Center (NCC), Goyang, Korea. 2018 Korean Liver Cancer Association-National Cancer Center Korea practice guidelines for the management of hepatocellular carcinoma. Korean J Radiol. 2019; 20(7):1042–1113. PMID: 31270974.26. Korean Association for the Study on the Liver. White Paper on Liver Diseases in Korea. Seoul, Korea: YD&P;2021.27. Park B, Choi KS, Lee HY, Jun JK, Park EC. Socioeconomic inequalities in completion of hepatitis B vaccine series among Korean women: results from a nationwide interview survey. Vaccine. 2012; 30(40):5844–5848. PMID: 22828587.28. Bhuiyan AR, Kabir N, Mitra AK, Ogungbe O, Payton M. Disparities in hepatitis B vaccine coverage by race/ethnicity: the National Health and Nutrition Examination Survey (NHANES) 2015-2016. Diseases. 2020; 8(2):10. PMID: 32316174.29. Zhu D, Guo N, Wang J, Nicholas S, Wang Z, Zhang G, et al. Socioeconomic inequality in hepatitis B vaccination of rural adults in China. Hum Vaccin Immunother. 2018; 14(2):464–470. PMID: 29072546.30. Clouston S, Kidman R, Palermo T. Social inequalities in vaccination uptake among children aged 0-59 months living in Madagascar: an analysis of Demographic and Health Survey data from 2008 to 2009. Vaccine. 2014; 32(28):3533–3539. PMID: 24814558.31. Barata RB, Ribeiro MC, de Moraes JC, Flannery B. Vaccine Coverage Survey 2007 Group. Socioeconomic inequalities and vaccination coverage: results of an immunisation coverage survey in 27 Brazilian capitals, 2007-2008. J Epidemiol Community Health. 2012; 66(10):934–941. PMID: 22268129.32. World Health Organization. Republic of Korea-WHO country Cooperation Strategy 2019-2023. WPRO/2019/DPM/001. Manila, Philippines: World Health Organization, Westen Pacific Region;2019.33. Heo JH, Whang JN. Income-related inequalities in cancer screening in Korea: using Concentration Index and Decomposition of CI. Pogon Sahoe Yongu. 2014; 34(3):59–81.34. Kwak M, Kim C. Disparities by age, sex, tumor stage, diagnosis path, and area-level socioeconomic status in survival time for major cancers: results from the Busan Cancer Registry. J Korean Med Sci. 2017; 32(12):1974–1983. PMID: 29115079.35. Yang D, Hanna DL, Usher J, LoCoco J, Chaudhari P, Lenz HJ, et al. Impact of sex on the survival of patients with hepatocellular carcinoma: a Surveillance, Epidemiology, and End Results analysis. Cancer. 2014; 120(23):3707–3716. PMID: 25081299.36. Income data of the National Tax Service’s quintile. Updated 2023. Accessed September 11, 2023. https://www.hidomin.com/news/articleView.html?idxno=523403 .37. OECD gender wage gap 2017. Updated 2023. Accessed September 11, 2023. https://www.oecd.org/country/korea/thematic-focus/gender-equality-korea-has-come-a-long-way-but-there-is-more-work-to-do-8bb81613/ .38. OECD gender wage gap 2022. Updated 2023. Accessed September 11, 2023. https://data.oecd.org/earnwage/gender-wage-gap.htm .39. National Health Insurance Service. Annual health examination rate. Updated 2023. Accessed September 12, 2023. https://www.nhis.or.kr/announce/wbhaec11407m01.do .
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Epidemiology of liver cancer in Korea
- Health Inequities in Cancer Incidence According to Economic Status and Regions Are Still Existed Even under Universal Health Coverage System in Korea: A Nationwide Population Based Study Using the National Health Insurance Database
- Impact of tumor size on hepatectomy outcomes in hepatocellular carcinoma: a nationwide propensity score matching analysis
- Yoon et al. Hepatocellular Carcinoma in Korea: an Analysis of the 2015 Korean Nationwide Cancer Registry
- Introduction of Relative Survival Analysis Program: Using Sample of Cancer Registry Data with Stata Software