J Rhinol.
2024 Mar;31(1):42-45. 10.18787/jr.2023.00071.
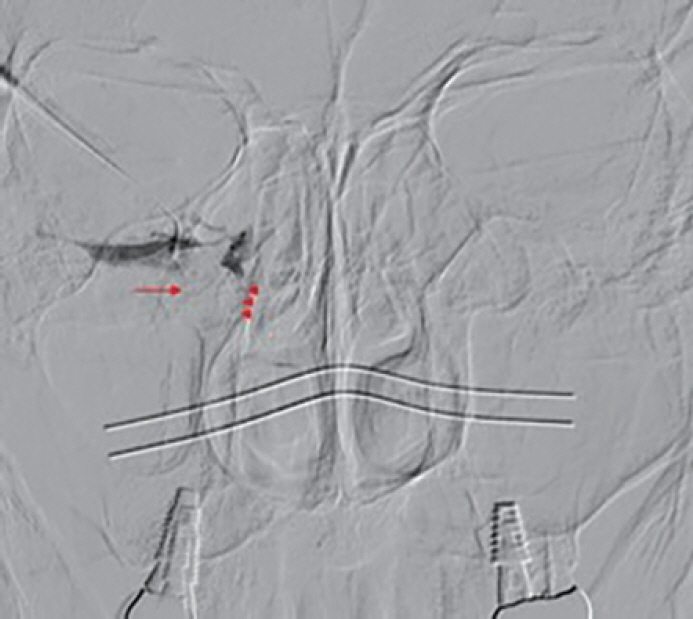
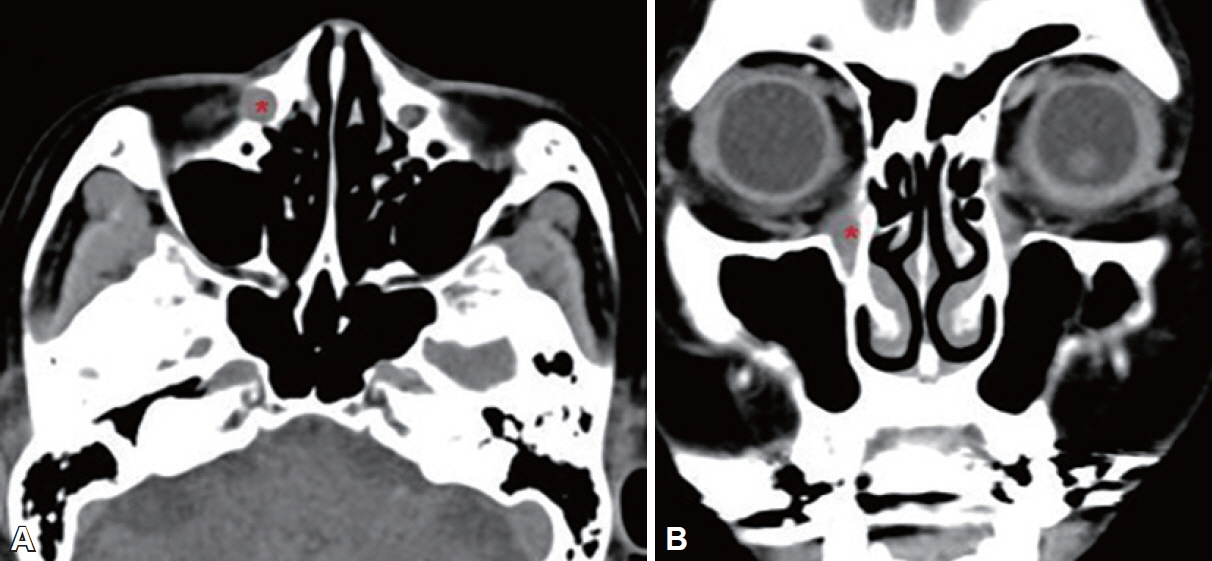
A Case of Nasolacrimal Duct Obstruction Caused by a Lacrimal Sac Retention Cyst
- KMID: 2554090
- DOI: http://doi.org/10.18787/jr.2023.00071
Abstract
- Acquired nasolacrimal duct obstruction may result from chronic infection, lacrimal stones, anatomical variations such as aberrant ethmoid cells, facial fractures, or complications following nasal surgery. In Korea, there has been no reported case of secondary nasolacrimal duct obstruction due to a retention cyst in the lacrimal sac. Recently, the authors encountered a 65-year-old female patient who presented with epiphora, was diagnosed with a lacrimal sac retention cyst, and was successfully treated with endoscopic marsupialization.
Figure
Reference
-
References
1. Perry LJ, Jakobiec FA, Zakka FR, Rubin PA. Giant dacryocystomucopyocele in an adult: a review of lacrimal sac enlargements with clinical and histopathologic differential diagnoses. Surv Ophthalmol. 2012; 57(5):474–85.
Article2. Yazici B, Hammad AM, Meyer DR. Lacrimal sac dacryoliths: predictive factors and clinical characteristics. Ophthalmology. 2001; 108(7):1308–12.3. Lee-Wing MW, Ashenhurst ME. Clinicopathologic analysis of 166 patients with primary acquired nasolacrimal duct obstruction. Ophthalmology. 2001; 108(11):2038–40.
Article4. Woog JJ. The incidence of symptomatic acquired lacrimal outflow obstruction among residents of Olmsted County, Minnesota, 1976-2000 (an American Ophthalmological Society thesis). Trans Am Ophthalmol Soc. 2007; 105:649–66.5. Bhaya M, Meehan R, Har-El G. Dacryocystocele in an adult: endoscopic management. Am J Otolaryngol. 1997; 18(2):131–4.
Article6. Cho SI, Do NY, Yu SW, Choi JY. [A case of endoscopic management of dacryocystocele in an adult]. Korean J Otorhinolaryngol-Head Neck Surg. 2010; 53(5):306–9. Korean.
Article7. Singh S, Ali MJ, Paulsen F. Dacryocystography: from theory to current practice. Ann Anat. 2019; 224:33–40.
Article8. Mills DM, Meyer DR. Acquired nasolacrimal duct obstruction. Otolaryngol Clin North Am. 2006; 39(5):979–99.
Article9. Hesselink JR, Davis KR, Dallow RL, Roberson GH, Taveras JM. Computed tomography of masses in the lacrimal gland region. Radiology. 1979; 131(1):143–7.
Article10. Kang MG, Shim WS, Shin DK, Kim JY, Lee JE, Jung HJ. A systematic review of benefit of silicone intubation in endoscopic dacryocystorhinostomy. Clin Exp Otorhinolaryngol. 2018; 11(2):81–8.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Nasolacrimal Duct Obstruction Following Midfacial Autologous Fat Injection
- Results with Silicone Stent in Lacrimal Drainage System
- The Role of Dacryocystography in Evaluation of Nasolacrimal Duct Obstruction
- Small Cell Neuroendocrine Carcinoma of the Lacrimal Sac Presenting with Lacrimal Duct Obstruction
- Result of Partial Nasolacrimal Duct Obstruction After Silicone Tube Intubation