J Rhinol.
2024 Mar;31(1):37-41. 10.18787/jr.2023.00070.
Isolated Sphenoid Fungal Sinusitis With Mucocele Mistaken for Chordoma: A Study of Two Unique Cases
- Affiliations
-
- 1Department of Otorhinolaryngology-Head and Neck Surgery, Korea University Ansan Hospital, Korea University College of Medicine, Ansan, Republic of Korea
- KMID: 2554089
- DOI: http://doi.org/10.18787/jr.2023.00070
Abstract
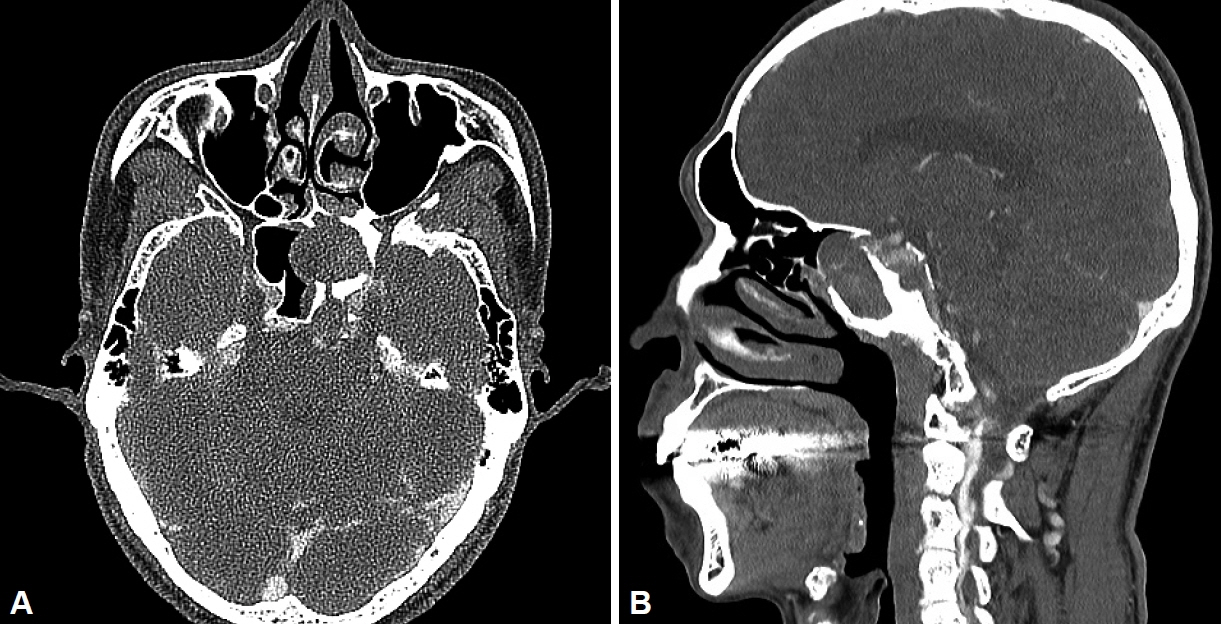
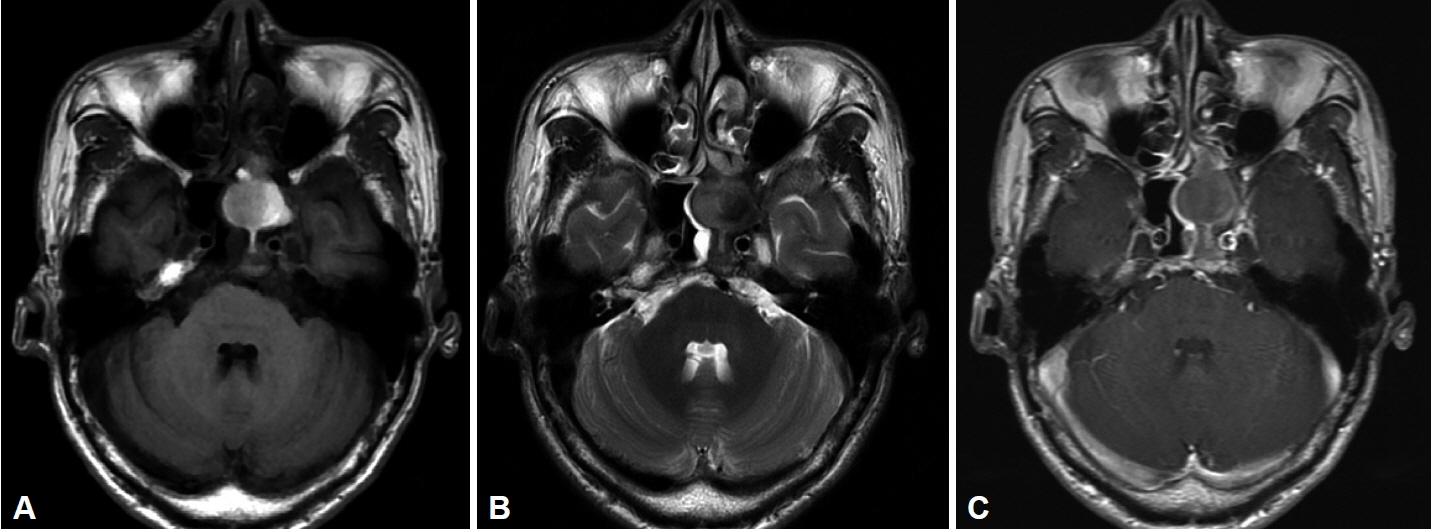
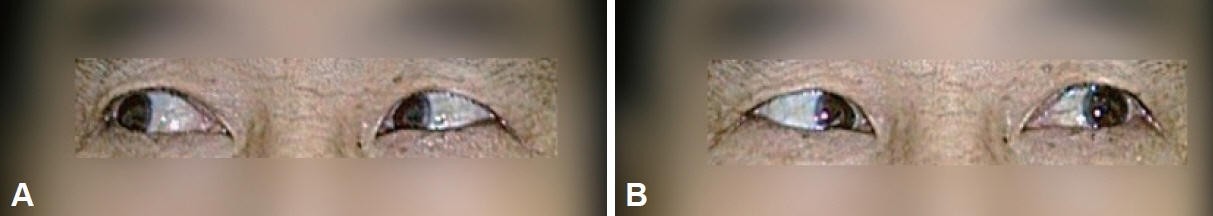
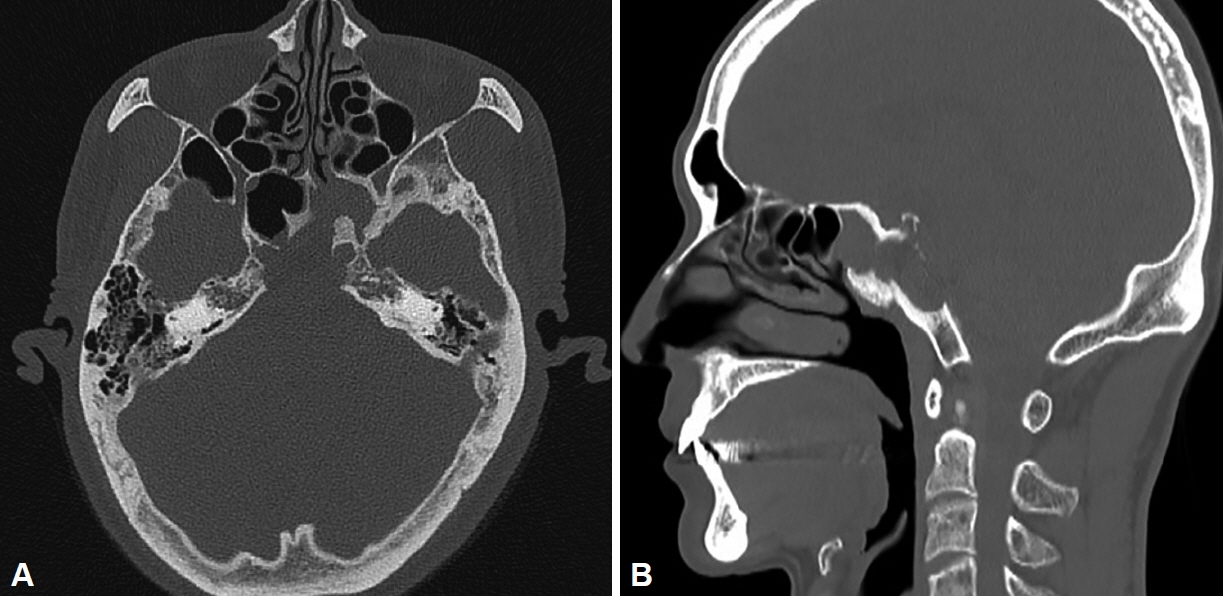
- Isolated sphenoid fungal sinusitis (ISFS) is a rare condition characterized by fungal infection of the sphenoid sinus. It often presents with non-specific symptoms, which can lead to misdiagnosis. This study presents two unique cases of ISFS with mucocele that were initially misdiagnosed as chordoma based on preoperative radiographic findings. Two cases of ISFS were thoroughly investigated, including clinical examinations, radiological assessments, and surgical explorations. The patients’ symptoms, radiographic findings, surgical procedures, and postoperative outcomes were documented. In both cases, radiographic assessments raised suspicion of chordoma due to bony destruction and soft tissue lesions involving the sphenoid sinus and clivus. However, endoscopic sinus surgery revealed fungal balls and mucoceles, confirming the diagnosis of ISFS. Postoperative pathology confirmed the presence of aspergilloma. The patients recovered well with appropriate treatment. ISFS is challenging to diagnose due to its deep anatomical location and non-specific symptoms. Visual disturbances, particularly affecting the abducens nerve, are common. Sphenoid sinus mucocele, though rare, can be present. Surgical exploration plays a crucial role in establishing an accurate diagnosis and initiating appropriate treatment. ISFS can mimic other skull base lesions, such as chordoma, on preoperative radiography. These cases underscore the value of surgical exploration in reaching an accurate diagnosis and highlight the need for the cautious interpretation of radiological findings in sphenoid sinus lesions to ensure optimal patient care.
Figure
Reference
-
References
1. Shaw CL, McCleave M, Wormald PJ. Unusual presentations of isolated sphenoid fungal sinusitis. J Laryngol Otol. 2000; 114(5):385–8.
Article2. Lew D, Southwick FS, Montgomery WW, Weber AL, Baker AS. Sphenoid sinusitis. A review of 30 cases. N Engl J Med. 1983; 309(19):1149–54.3. Giovannetti F, Filiaci F, Ramieri V, Ungari C. Isolated sphenoid sinus mucocele: etiology and management. J Craniofac Surg. 2008; 19(5):1381–4.4. Bharti S, Bharti JN. A case report of chordoma presenting as a sphenoid sinus mass: a diagnostic challenge. Curr Med Imaging. 2023; 19(7):780–3.5. Socher JA, Cassano M, Filheiro CA, Cassano P, Felippu A. Diagnosis and treatment of isolated sphenoid sinus disease: a review of 109 cases. Acta Otolaryngol. 2008; 128(9):1004–10.
Article6. Lawson W, Reino AJ. Isolated sphenoid sinus disease: an analysis of 132 cases. Laryngoscope. 1997; 107(12 Pt 1):1590–5.
Article7. Broderick DF. The opacified paranasal sinus: approach and differential. Appl Radiol. 2015; 44(8):9–17.
Article8. Seo YJ, Kim J, Kim K, Lee JG, Kim CH, Yoon JH. Radiologic characteristics of sinonasal fungus ball: an analysis of 119 cases. Acta Radiol. 2011; 52(7):790–5.
Article9. Betts AM, Cornelius R. Magnetic resonance imaging in sinonasal disease. Top Magn Reson Imaging. 2015; 24(1):15–22.
Article10. Madani G, Beale TJ. Differential diagnosis in sinonasal disease. Semin Ultrasound CT MR. 2009; 30(1):39–45.
Article11. Bowman J, Panizza B, Gandhi M. Sphenoid sinus fungal balls. Ann Otol Rhinol Laryngol. 2007; 116(7):514–9.
Article12. Moss WJ, Finegersh A, Jafari A, Panuganti B, Coffey CS, DeConde A, et al. Isolated sphenoid sinus opacifications: a systematic review and meta-analysis. Int Forum Allergy Rhinol. 2017; 7(12):1201–6.
Article13. Lee KJ, Yanagisawa K. An obscure etiology for headache: sphenoid sinus disease. Yonsei Med J. 1988; 29(3):209–18.
Article14. Soon SR, Lim CM, Singh H, Sethi DS. Sphenoid sinus mucocele: 10 cases and literature review. J Laryngol Otol. 2010; 124(1):44–7.
Article15. Lee DH, Jang WY, Yoon TM, Lee JK, Jung S, Lim SC. Sphenoid sinus mucocele caused by complications after transsphenoidal pituitary surgery. J Craniofac Surg. 2018; 29(7):1859–61.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endoscopic Diagnosis and Treatment of Isolated Sphenoid Sinus Lesions
- A Case of Abducens Nerve Palsy Caused by Isolated Sphenoid Fungal Sinusitis
- Acute Rhinosinusitis in Prominently Pneumatized Sphenoid Sinus Presenting with Unilateral Abducens Nerve Palsy
- A Case of Ethmoid Mucocele with Superimposed Fungal Infection
- Clinical Analysis of Isolated Sphenoid Sinusitis