Ann Hepatobiliary Pancreat Surg.
2024 Feb;28(1):70-79. 10.14701/ahbps.23-071.
Do some patients receive unnecessary parenteral nutrition after pancreatoduodenectomy? Results from an international multicentre study
- Affiliations
-
- 1Department of HPB Surgery, University Hospitals Plymouth NHS Trust, Plymouth, UK
- 2Department of HPB Surgery, Hospital Clinic de Barcelona, Barcelona, Spain
- 3Department of HPB Surgery, Hospital Universitari Vall d’Hebron, Barcelona, Spain
- 4Department of HPB Surgery, University Hospitals Birmingham NHS Foundation Trust, Birmingham, UK
- 5Department of HPB Surgery, East Lancashire Hospitals NHS Trust, Blackburn, UK
- 6Department of HPB Surgery, University Hospitals Bristol NHS Foundation Trust, Bristol, UK
- 7Department of HPB Surgery, The Royal Marsden NHS Foundation Trust, London, UK
- 8Department of HPB Surgery, University Hospital Coventry & Warwickshire, Coventry, UK
- 9Department of HPB Surgery, NHS Lothian, Edinburgh, UK
- 10Department of HPB Surgery, Royal Surrey NHS Foundation Trust, Guildford, UK
- 11Department of HPB Surgery, Hull University Teaching Hospitals NHS Trust, Hull, UK
- 12Department of HPB Surgery, Medical University of Innsbruck, Innsbruck, Austria
- 13Department of HPB Surgery, Ibn Sina Specialized Hospital, Khartoum, Sudan
- 14Department of HPB Surgery, Shaukat Khanum Memorial Cancer Hospital, Lahore, Pakistan
- 15Department of HPB Surgery, Leeds Teaching Hospitals NHS Trust, Leeds, UK
- 16Department of HPB Surgery, Imperial College Healthcare NHS Trust, London, UK
- 17Department of HPB Surgery, King’s College Hospital NHS Foundation Trust, London, UK
- 18Department of HPB Surgery, Royal Free London NHS Foundation Trust, London, UK
- 19Department of HPB Surgery, Monash Medical Centre, Melbourne, Australia
- 20Department of HPB Surgery, Salvador Zubiran National Institute of Health Sciences and Nutrition, Mexico City, Mexico
- 21Department of HPB Surgery, Newcastle upon Tyne Hospitals NHS Foundation Trust, Newcastle upon Tyne, UK
- 22Department of HPB Surgery, Nottingham University Hospitals NHS Trust, Nottingham, UK
- 23Department of HPB Surgery, Oxford University Hospitals NHS Foundation Trust, Oxford, UK
- 24Department of HPB Surgery, Policlinico Umberto I University Hospital Sapienza, Rome, Italy
- 25Department of HPB Surgery, Azienda Ospedaliero Universitaria di Sassari, Sassari, Italy
- 26Department of HPB Surgery, Sheffield Teaching Hospitals NHS Foundation Trust, Sheffield, UK
- 27Department of HPB Surgery, University Hospital Southampton NHS Foundation Trust, Southampton, UK
- 28Department of HPB Surgery, Swansea Bay University Health Board, Swansea, UK
- 29Department of HPB Surgery, Hospital Universitario Miguel Servet, Zaragoza, Spain
- KMID: 2553368
- DOI: http://doi.org/10.14701/ahbps.23-071
Abstract
- Backgrounds/Aims
After pancreatoduodenectomy (PD), an early oral diet is recommended; however, the postoperative nutritional management of PD patients is known to be highly variable, with some centers still routinely providing parenteral nutrition (PN). Some patients who receive PN experience clinically significant complications, underscoring its judicious use. Using a large cohort, this study aimed to determine the proportion of PD patients who received postoperative nutritional support (NS), describe the nature of this support, and investigate whether receiving PN correlated with adverse perioperative outcomes.
Methods
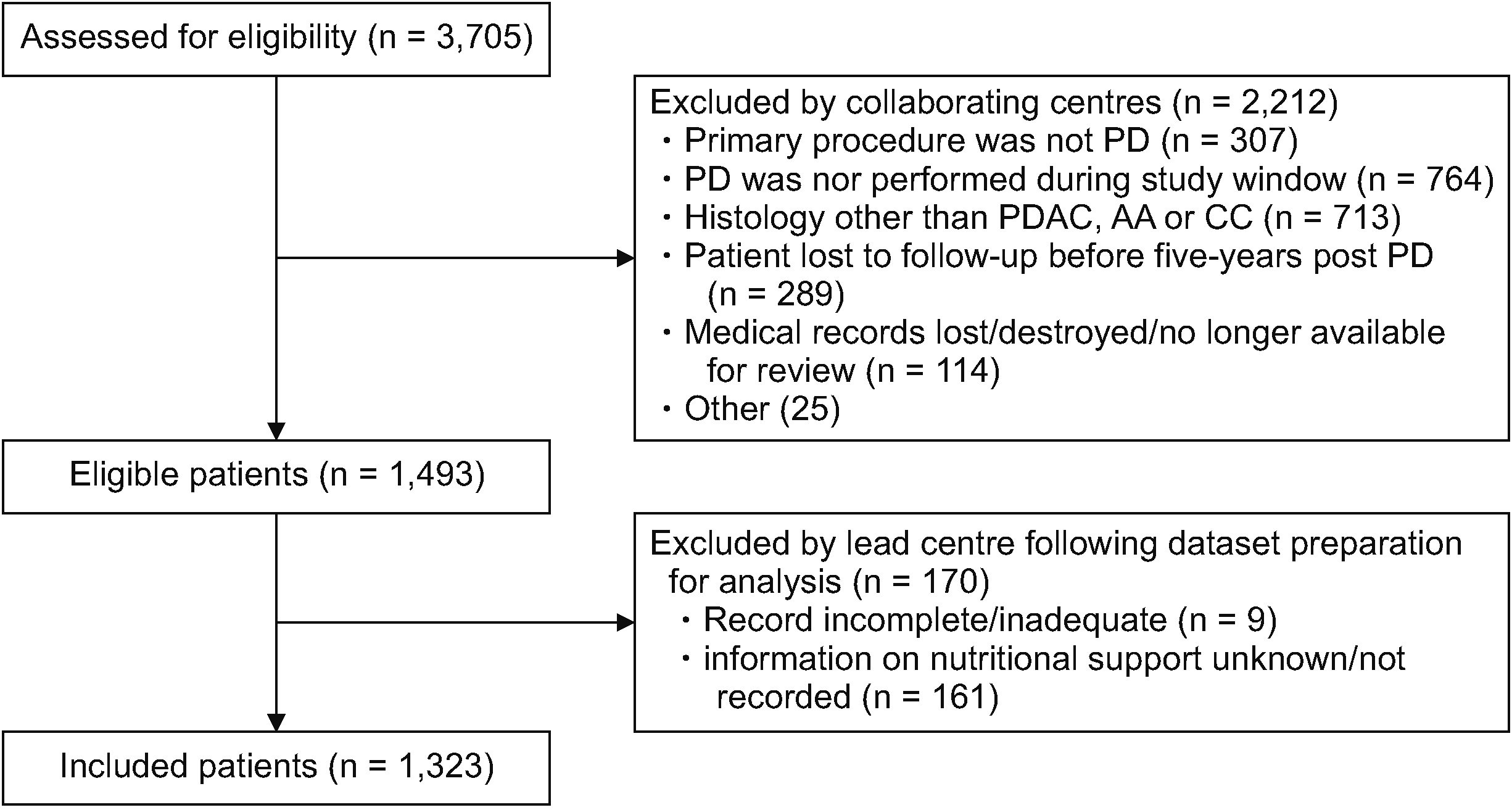
Data were extracted from the Recurrence After Whipple’s study, a retrospective multicenter study of PD outcomes.
Results
In total, 1,323 patients (89%) had data on their postoperative NS status available. Of these, 45% received postoperative NS, which was “enteral only,” “parenteral only,” and “enteral and parenteral” in 44%, 35%, and 21% of cases, respectively. Body mass index < 18.5 kg/m2 (p = 0.03), absence of preoperative biliary stenting (p = 0.009), and serum albumin < 36 g/L (p = 0.009) all correlated with receiving postoperative NS. Among those who did not develop a serious postoperative complication, i.e., those who had a relatively uneventful recovery, 20% received PN.
Conclusions
A considerable number of patients who had an uneventful recovery received PN. PN is not without risk, and should be reserved for those who are unable to take an oral diet. PD patients should undergo pre- and postoperative assessment by nutrition professionals to ensure they are managed appropriately, and to optimize perioperative outcomes.
Keyword
Figure
Reference
-
1. Lassen K, Coolsen MM, Slim K, Carli F, de Aguilar-Nascimento JE, Schäfer M, et al. 2013; Guidelines for perioperative care for pancreaticoduodenectomy: Enhanced Recovery After Surgery (ERAS®) Society recommendations. World J Surg. 37:240–258. DOI: 10.1007/s00268-012-1771-1. PMID: 22956014.
Article2. Cai J, Yang G, Tao Y, Han Y, Lin L, Wang X. 2020; A meta-analysis of the effect of early enteral nutrition versus total parenteral nutrition on patients after pancreaticoduodenectomy. HPB (Oxford). 22:20–25. DOI: 10.1016/j.hpb.2019.06.002. PMID: 31353255.
Article3. Jeejeebhoy KN. 2007; Enteral nutrition versus parenteral nutrition-the risks and benefits. Nat Clin Pract Gastroenterol Hepatol. 4:260–265. DOI: 10.1038/ncpgasthep0797. PMID: 17476208.
Article4. Xiong J, Szatmary P, Huang W, de la Iglesia-Garcia D, Nunes QM, Xia Q, et al. 2016; Enhanced recovery after surgery program in patients undergoing pancreaticoduodenectomy: a PRISMA-compliant systematic review and meta-analysis. Medicine (Baltimore). 95:e3497. DOI: 10.1097/MD.0000000000003497. PMID: 27149448. PMCID: PMC4863765.5. Deng X, Cheng X, Huo Z, Shi Y, Jin Z, Feng H, et al. 2017; Modified protocol for enhanced recovery after surgery is beneficial for Chinese cancer patients undergoing pancreaticoduodenectomy. Oncotarget. 8:47841–47848. DOI: 10.18632/oncotarget.18092. PMID: 28615506. PMCID: PMC5564609.
Article6. Russell TB, Murphy P, Tanase A, Sen G, Aroori S. 2022; Results from a UK-wide survey: the nutritional assessment and management of pancreatic resection patients is highly variable. Eur J Clin Nutr. 76:1038–1040. DOI: 10.1038/s41430-021-01063-5. PMID: 35027684.
Article7. Martin D, Joliat GR, Halkic N, Demartines N, Schäfer M. 2020; Perioperative nutritional management of patients undergoing pancreatoduodenectomy: an international survey among surgeons. HPB (Oxford). 22:75–82. DOI: 10.1016/j.hpb.2019.05.009. PMID: 31257012.
Article8. Loinaz Segurola C, Ochando Cerdán F, Vicente López E, Serrablo Requejo A, López Cillero P, Gómez Bravo MÁ, et al. 2020; Results of a survey on peri-operative nutritional support in pancreatic and biliary surgery in Spain. Nutr Hosp. 37:238–242. DOI: 10.20960/nh.02895. PMID: 32090583.
Article9. Miller SJ. 2008; Death resulting from overzealous total parenteral nutrition: the refeeding syndrome revisited. Nutr Clin Pract. 23:166–171. DOI: 10.1177/0884533608314538. PMID: 18390784.
Article10. Dindo D, Demartines N, Clavien PA. 2004; Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 240:205–213. DOI: 10.1097/01.sla.0000133083.54934.ae. PMID: 15273542. PMCID: PMC1360123.11. Grau D, Clarivet B, Lotthé A, Bommart S, Parer S. 2017; Complications with peripherally inserted central catheters (PICCs) used in hospitalized patients and outpatients: a prospective cohort study. Antimicrob Resist Infect Control. 6:18. DOI: 10.1186/s13756-016-0161-0. PMID: 28149507. PMCID: PMC5273851.
Article12. Hartl WH, Jauch KW, Parhofer K, Rittler P. Working group for developing the guidelines for parenteral nutrition of The German Association for Nutritional Medicine. 2009; Complications and monitoring - Guidelines on Parenteral Nutrition, Chapter 11. Ger Med Sci. 7:Doc17.13. National Collaborating Centre for Acute Care. Nutrition Support for Adults: Oral Nutrition Support, Enteral Tube Feeding and Parenteral Nutrition. National Collaborating Centre for Acute Care (UK);2006.14. Melloul E, Lassen K, Roulin D, Grass F, Perinel J, Adham M, et al. 2020; Guidelines for perioperative care for pancreatoduodenectomy: Enhanced Recovery After Surgery (ERAS) recommendations 2019. World J Surg. 44:2056–2084. DOI: 10.1007/s00268-020-05462-w. PMID: 32161987.
Article15. Weimann A, Braga M, Harsanyi L, Laviano A, Ljungqvist O, Soeters P, et al. 2006; ESPEN guidelines on enteral nutrition: surgery including organ transplantation. Clin Nutr. 25:224–244. DOI: 10.1016/j.clnu.2006.01.015. PMID: 16698152.
Article16. Weimann A, Braga M, Carli F, Higashiguchi T, Hübner M, Klek S, et al. 2017; ESPEN guideline: clinical nutrition in surgery. Clin Nutr. 36:623–650. DOI: 10.1016/j.clnu.2017.02.013. PMID: 28385477.
Article17. Takagi K, Domagala P, Hartog H, van Eijck C, Groot Koerkamp B. 2019; Current evidence of nutritional therapy in pancreatoduodenectomy: systematic review of randomized controlled trials. Ann Gastroenterol Surg. 3:620–629. DOI: 10.1002/ags3.12287. PMID: 31788650. PMCID: PMC6875945.
Article18. Kapoor D, Barreto SG, Perwaiz A, Singh A, Chaudhary A. 2022; Can we predict the need for nutritional support following pancreatoduodenectomy? Pancreatology. 22:160–167. DOI: 10.1016/j.pan.2021.11.010. PMID: 34893447.
Article19. Atema JJ, Eshuis WJ, Busch OR, van Gulik TM, Gouma DJ. 2013; Association of preoperative symptoms of gastric outlet obstruction with delayed gastric emptying after pancreatoduodenectomy. Surgery. 154:583–588. DOI: 10.1016/j.surg.2013.04.006. PMID: 23972659.
Article20. Greenblatt DY, Kelly KJ, Rajamanickam V, Wan Y, Hanson T, Rettammel R, et al. 2011; Preoperative factors predict perioperative morbidity and mortality after pancreaticoduodenectomy. Ann Surg Oncol. 18:2126–2135. DOI: 10.1245/s10434-011-1594-6. PMID: 21336514.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Incidence of sepsis associated with total parenteral nutrition solutions made in the nursery and pharmacy
- Strategy for Activation of Home Total Parenteral Nutrition
- Management and Prevention of Possible Complications Associated with Total Parenteral Nutrition
- Nutrition Support Methods in Elderly Patients
- Parenteral Nutrition Support in Preterm Infants