Ann Hepatobiliary Pancreat Surg.
2024 Feb;28(1):42-47. 10.14701/ahbps.23-085.
Outcomes of laparoscopic choledochotomy using cholangioscopy via percutaneous-choledochal tube for the treatment of hepatolithiasis and choledocholithiasis: A preliminary Vietnamese study
- Affiliations
-
- 1Department of Hepatopancreatobiliary Surgery, Institute of Digestive Surgery, 108 Military Central Hospital, Hanoi, Vietnam
- 2College of Health Sciences, VinUniversity, Hanoi, Vietnam
- KMID: 2553364
- DOI: http://doi.org/10.14701/ahbps.23-085
Abstract
- Backgrounds/Aims
Hepatolithiasis and choledocholithiasis are frequent pathologies and unfortunately, with the current treatment strategies, the recurrence incidence is still high. This study aimed to assess the outcomes of laparoscopic choledochotomy using cholangioscopy via the percutaneous-choledochal tube for the treatment of hepatolithiasis and choledocholithiasis in Vietnamese patients.
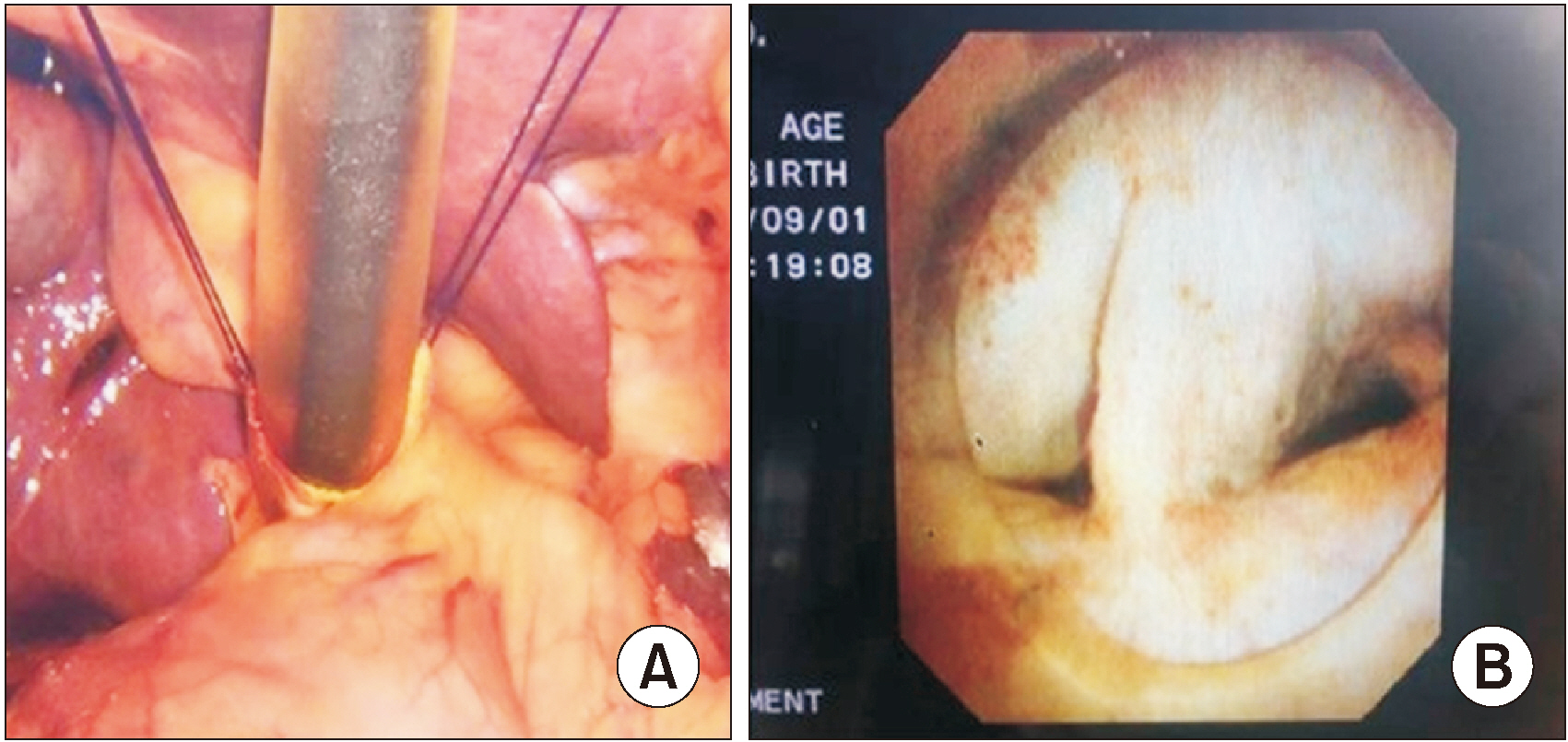
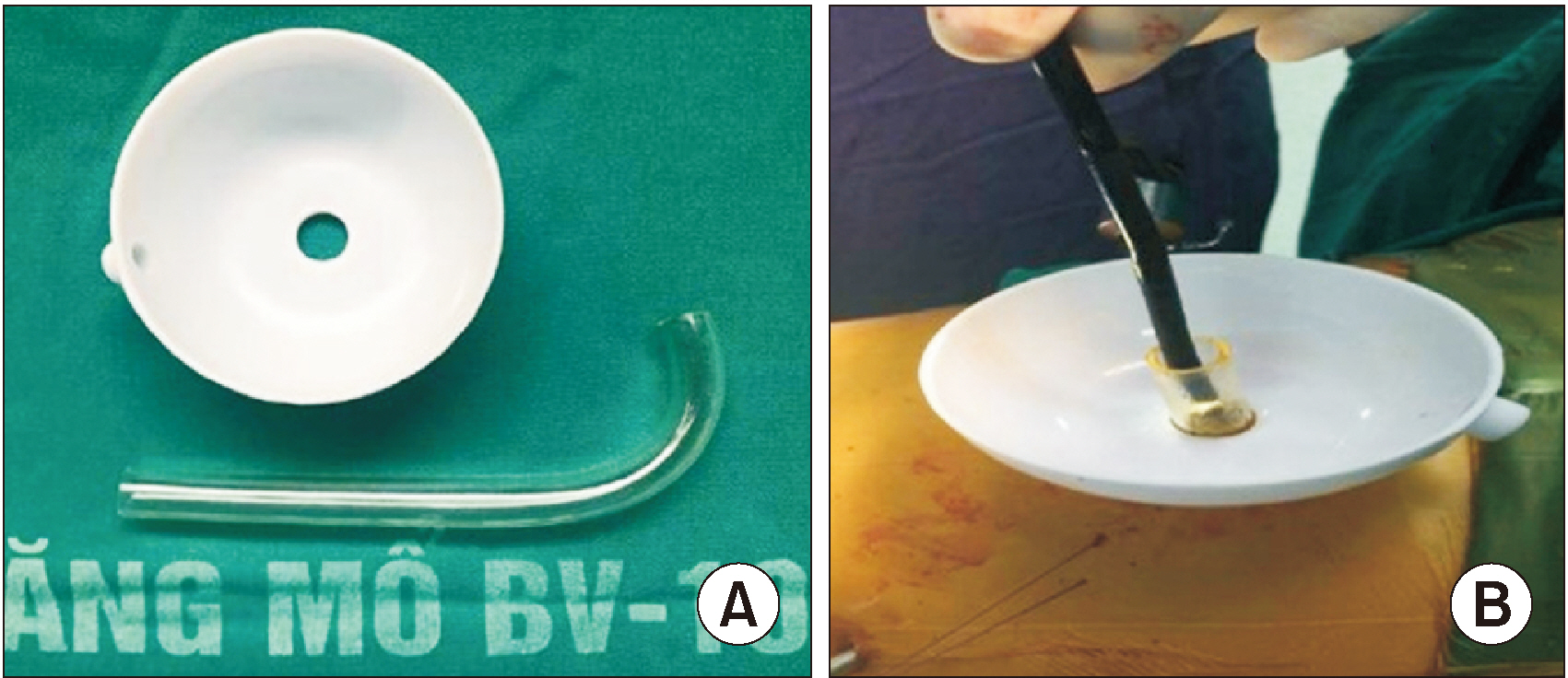
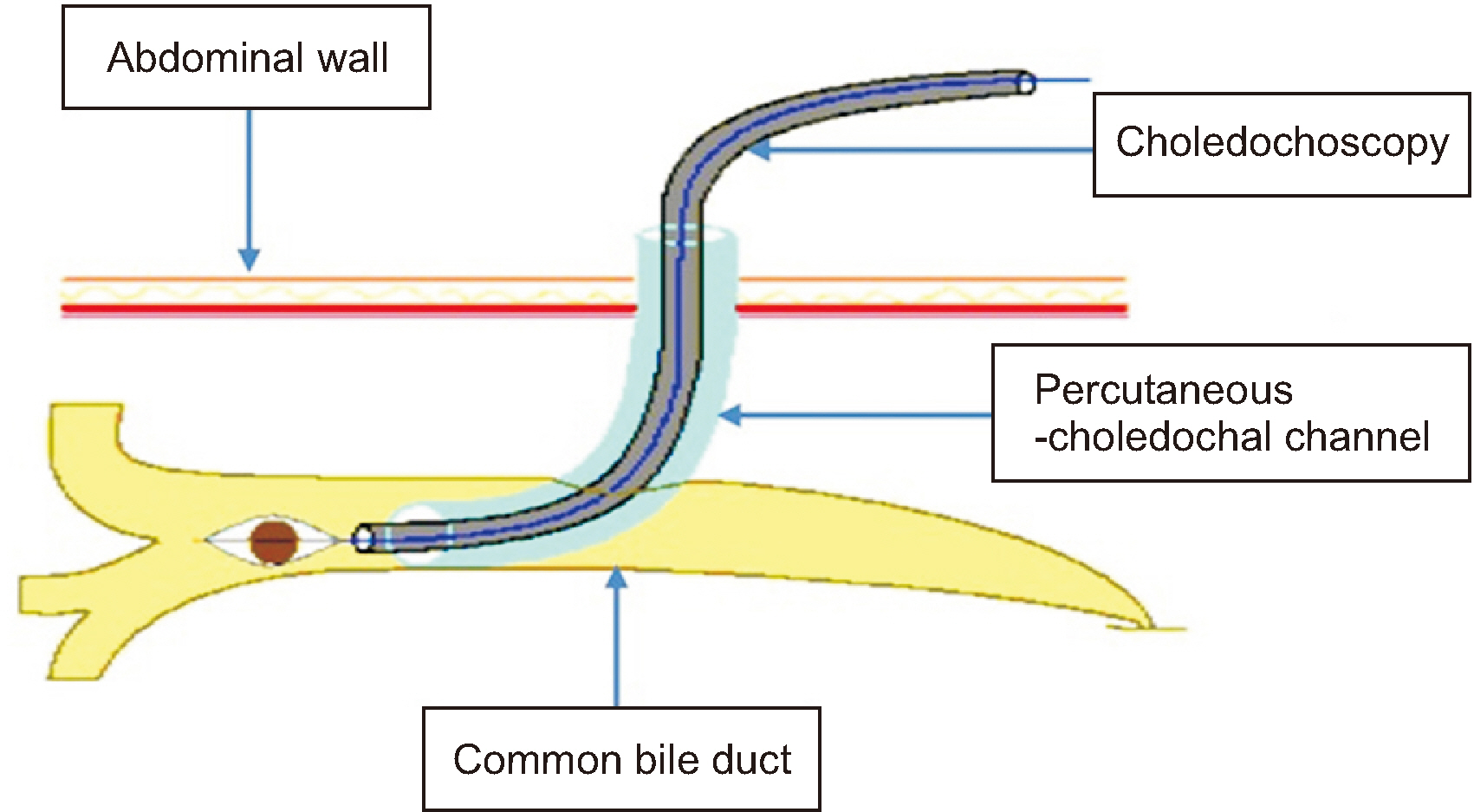
Methods
A cross-sectional study of patients with hepatolithiasis and/or choledocholithiasis who underwent laparoscopic choledochotomy using intraoperative cholangioscopy via percutaneous-choledochal tube at the Department of Hepatopancreatobiliary Surgery, 108 Military Central Hospital, from June 2017 to March 2020.
Results
A total of 84 patients were analyzed. Most patients were females (56.0%) with a median age of 55.56 years. Among them, 41.8% of patients had previous abdominal operations, with 33.4% having choledochotomy. All patients underwent successful laparoscopic common bile duct exploration followed by T-tube drainage without needing to convert to open surgery. Most patients (64.3%) had both intrahepatic and extrahepatic stones. The rate of stones ≥ 10 mm in diameter was 64.3%. Biliary strictures were observed in 19.1% of patients during cholangioscopy. Complete removal of stones was achieved in 54.8% of patients. Intraoperative complications were encountered in two patients, but there was no need to change the strategy. The mean operating time was 121.85 ± 30.47 minutes. The early postoperative complication rate was 9.6%, and all patients were managed conservatively. The residual stones were removed through the T-tube tract by subsequent choledochoscopy in 34/38 patients, so the total success rate was 95.2%.
Conclusions
Laparoscopic choledochotomy combined with cholangioscopy through the percutaneous-choledochal tube is a safe and effective strategy for hepatolithiasis and/or choledocholithiasis, even in patients with a previous choledochotomy.
Figure
Reference
-
1. Feng X, Zheng S, Xia F, Ma K, Wang S, Bie P, et al. 2012; Classification and management of hepatolithiasis: a high-volume, single-center's experience. Intractable Rare Dis Res. 1:151–156. DOI: 10.5582/irdr.2012.v1.4.151. PMID: 25343089. PMCID: PMC4204570.2. Molvar C, Glaenzer B. 2016; Choledocholithiasis: evaluation, treatment, and outcomes. Semin Intervent Radiol. 33:268–276. DOI: 10.1055/s-0036-1592329. PMID: 27904245. PMCID: PMC5088099.3. Pausawasdi A, Watanapa P. 1997; Hepatolithiasis: epidemiology and classification. Hepatogastroenterology. 44:314–316. DOI: 10.3138/9781442672789-053.4. European Association for the Study of the Liver (EASL). 2016; EASL Clinical Practice Guidelines on the prevention, diagnosis and treatment of gallstones. J Hepatol. 65:146–181. DOI: 10.1016/j.jhep.2016.03.005. PMID: 27085810.5. Kim HJ, Kim JS, Suh SJ, Lee BJ, Park JJ, Lee HS, et al. 2015; Cholangiocarcinoma risk as long-term outcome after hepatic resection in the hepatolithiasis patients. World J Surg. 39:1537–1542. DOI: 10.1007/s00268-015-2965-0. PMID: 25648078.6. Xia H, Zhang H, Xin X, Liang B, Yang T, Liu Y, et al. 2023; Surgical management of recurrence of primary intrahepatic bile duct stones. Can J Gastroenterol Hepatol. 2023:5158580. DOI: 10.1155/2023/5158580. PMID: 36726399. PMCID: PMC9886471.7. Wu Y, Xu CJ, Xu SF. 2021; Advances in risk factors for recurrence of common bile duct stones. Int J Med Sci. 18:1067–1074. DOI: 10.7150/ijms.52974. PMID: 33456365. PMCID: PMC7807200.
Article8. Csendes A, Burdiles P, Diaz JC. 1998; Present role of classic open choledochostomy in the surgical treatment of patients with common bile duct stones. World J Surg. 22:1167–1170. DOI: 10.1007/s002689900537. PMID: 9828726.
Article9. Andriulli A, Loperfido S, Napolitano G, Niro G, Valvano MR, Spirito F, et al. 2007; Incidence rates of post-ERCP complications: a systematic survey of prospective studies. Am J Gastroenterol. 102:1781–1788. DOI: 10.1111/j.1572-0241.2007.01279.x. PMID: 17509029.
Article10. Liu YY, Li TY, Wu SD, Fan Y. 2022; The safety and feasibility of laparoscopic approach for the management of intrahepatic and extrahepatic bile duct stones in patients with prior biliary tract surgical interventions. Sci Rep. 12:14487. DOI: 10.1038/s41598-022-18930-1. PMID: 36008517. PMCID: PMC9411189.
Article11. Wang Y, Huang Y, Shi C, Wang L, Liu S, Zhang J, et al. 2022; Efficacy and safety of laparoscopic common bile duct exploration via choledochotomy with primary closure for the management of acute cholangitis caused by common bile duct stones. Surg Endosc. 36:4869–4877. DOI: 10.1007/s00464-021-08838-8. PMID: 34724579. PMCID: PMC9160116.
Article12. Lien HH, Huang CC, Huang CS, Shi MY, Chen DF, Wang NY, et al. 2005; Laparoscopic common bile duct exploration with T-tube choledochotomy for the management of choledocholithiasis. J Laparoendosc Adv Surg Tech A. 15:298–302. DOI: 10.1089/lap.2005.15.298. PMID: 15954833.
Article13. Khaled YS, Malde DJ, de Souza C, Kalia A, Ammori BJ. 2013; Laparoscopic bile duct exploration via choledochotomy followed by primary duct closure is feasible and safe for the treatment of choledocholithiasis. Surg Endosc. 27:4164–4170. DOI: 10.1007/s00464-013-3015-3. PMID: 23719974.
Article14. Zhang WL, Fang ZP, Shi BY, Chen T, Lv SD, Wang C, et al. 2021; Low-pressure pulse flushing choledochoscopy combined with neodymium laser lithotripsy for the treatment of intrahepatic bile duct stones. Hepatobiliary Pancreat Dis Int. 20:383–386. DOI: 10.1016/j.hbpd.2021.04.002. PMID: 33931315.
Article15. Zhou Y, Wu XD, Fan RG, Zhou GJ, Mu XM, Zha WZ, et al. 2014; Laparoscopic common bile duct exploration and primary closure of choledochotomy after failed endoscopic sphincterotomy. Int J Surg. 12:645–648. DOI: 10.1016/j.ijsu.2014.05.059. PMID: 24879343.
Article16. Gómez DA, Mendoza Zuchini A, Pedraza M, Salcedo Miranda DF, Mantilla-Sylvain F, Pérez Rivera CJ, et al. 2023; Long-term outcomes of laparoscopic common bile duct exploration through diathermy, choledochotomy, and primary closure: a 6-year retrospective cohort study. J Laparoendosc Adv Surg Tech A. 33:281–286. DOI: 10.1089/lap.2022.0453. PMID: 36576507.
Article17. Al-Qudah G, Tuma F. T Tube [Internet]. 2022. Available from: https://www.ncbi.nlm.nih.gov/books/NBK532867/. cited 2023 Jun 15.18. Li S, Su B, Chen P, Hao J. 2018; Risk factors for recurrence of common bile duct stones after endoscopic biliary sphincterotomy. J Int Med Res. 46:2595–2605. DOI: 10.1177/0300060518765605. PMID: 29865913. PMCID: PMC6124257.
Article19. Deng F, Zhou M, Liu PP, Hong JB, Li GH, Zhou XJ, et al. 2019; Causes associated with recurrent choledocholithiasis following therapeutic endoscopic retrograde cholangiopancreatography: a large sample sized retrospective study. World J Clin Cases. 7:1028–1037. DOI: 10.12998/wjcc.v7.i9.1028. PMID: 31123675. PMCID: PMC6511924.
Article20. Dilek ON, Atasever A, Acar N, Karasu Ş, Özlem Gür E, Özşay O, et al. 2020; Hepatolithiasis: clinical series, review and current management strategy. Turk J Surg. 36:382–392. DOI: 10.47717/turkjsurg.2020.4551. PMID: 33778398. PMCID: PMC7963303.
Article21. Jutric Z, Hammill CW, Hansen PD. Jarnagin WR, editor. 2017; Chapter 36B - Stones in the bile duct: Minimally invasive surgical approaches. Blumgart's Surgery of the Liver, Biliary Tract and Pancreas, 2-Volume Set. Sixth Edition. Elsevier;2017; 604–610.e1. DOI: 10.1016/B978-0-323-34062-5.00143-6.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Treatment of hepatolithiasis
- Primary common bile duct closure and antegrade stent insertion in choledocholithiasis patients
- Analysis on the Clinical Significance of Biliary Exploration through the Left Hepatic Duct Opening during Left Hepatectomy for the Patients with Hepatolithiasis
- Comparison of Primary Closure and T-tube Drainage following Laparoscopic CBD Exploration
- A Clinical Analysis of Open T-tube Choledochostomy