Ann Hepatobiliary Pancreat Surg.
2024 Feb;28(1):1-13. 10.14701/ahbps.23-090.
The impact of waiting time and delayed treatment on the outcomes of patients with hepatocellular carcinoma: A systematic review and meta-analysis
- Affiliations
-
- 1Yong Loo Lin School of Medicine, National University of Singapore, Singapore
- 2Department of General Surgery, Tan Tock Seng Hospital, Singapore
- 3Lee Kong Chian School of Medicine, Nanyang Technological University, Singapore
- KMID: 2553360
- DOI: http://doi.org/10.14701/ahbps.23-090
Abstract
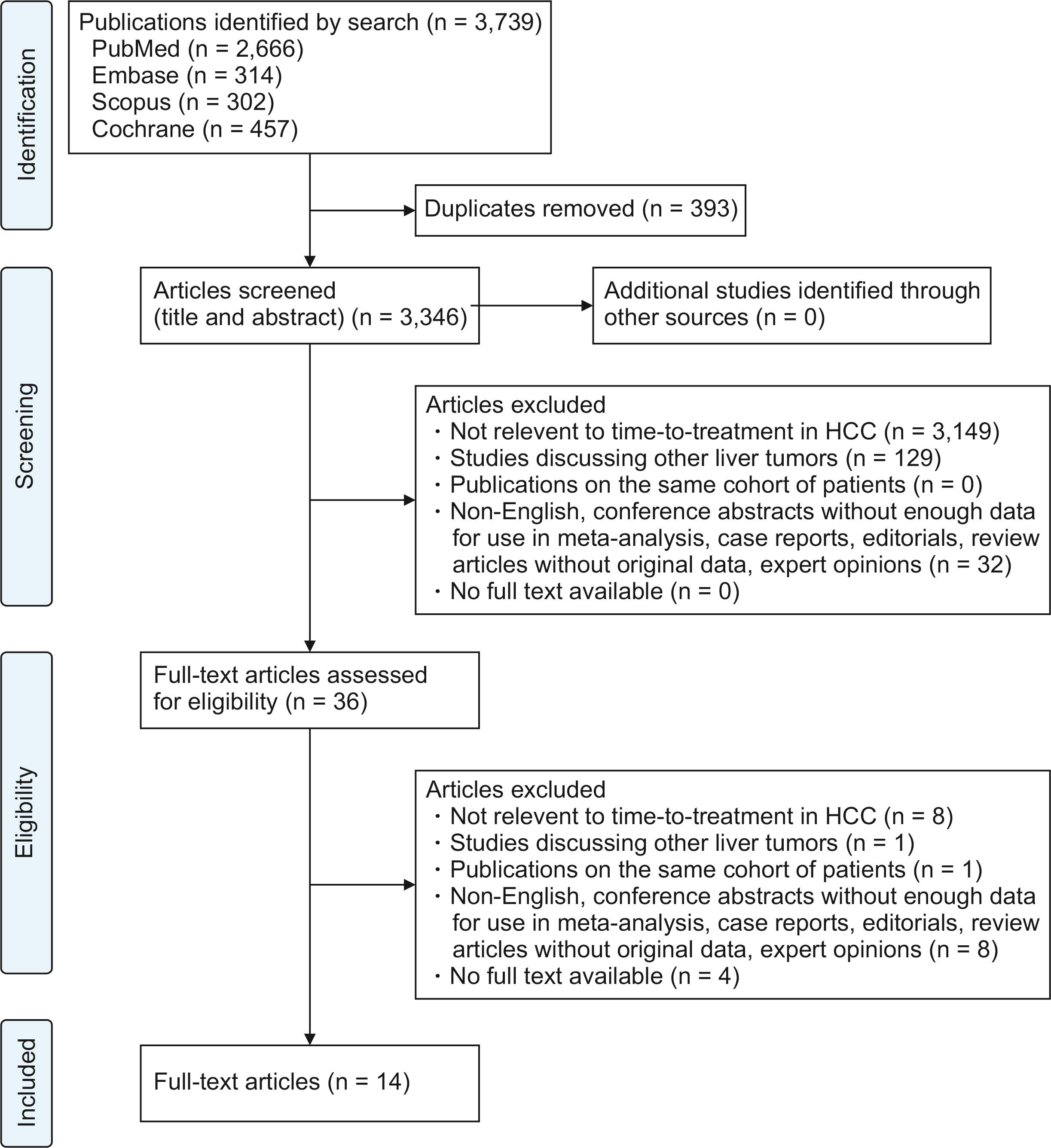
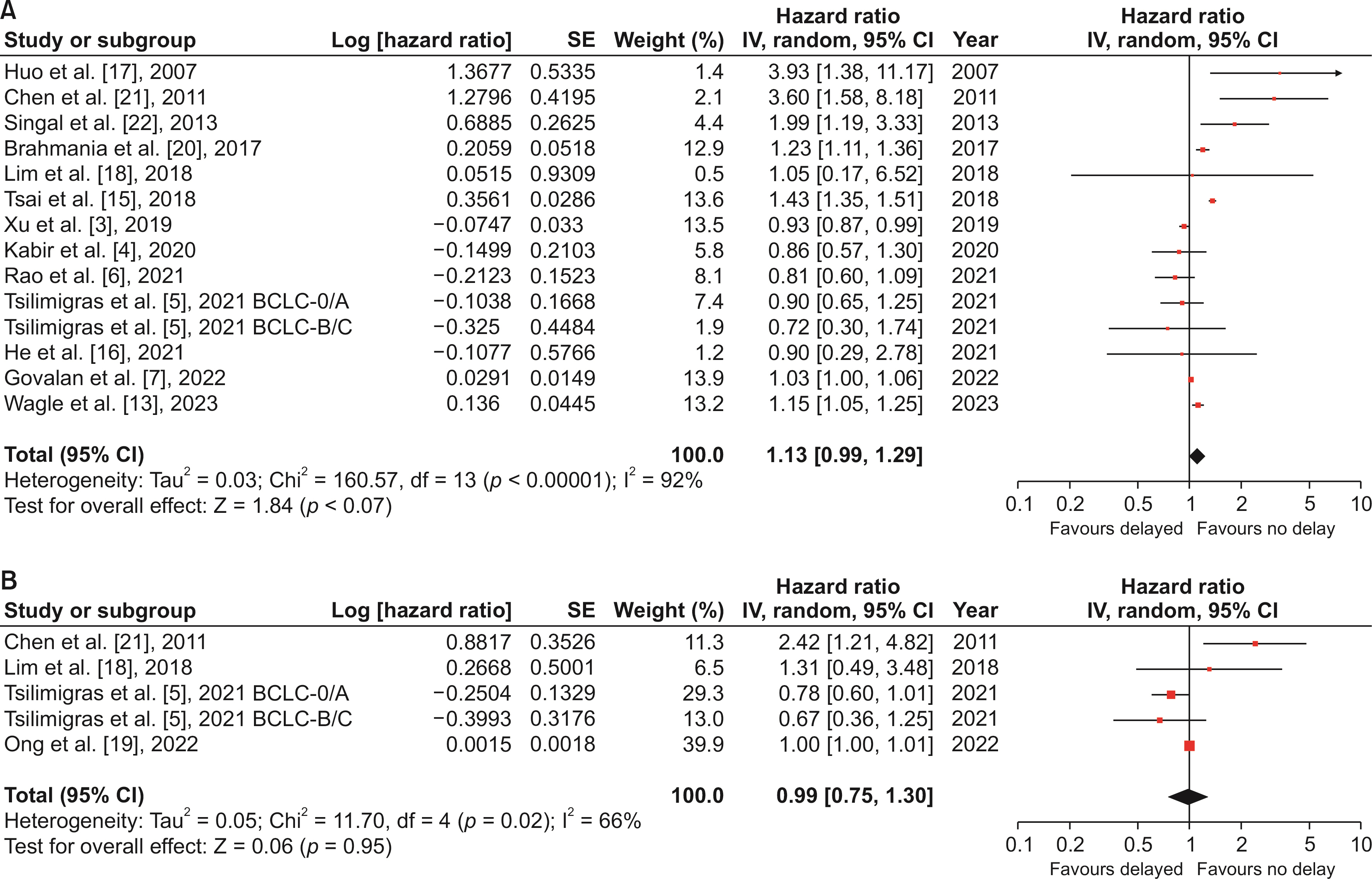
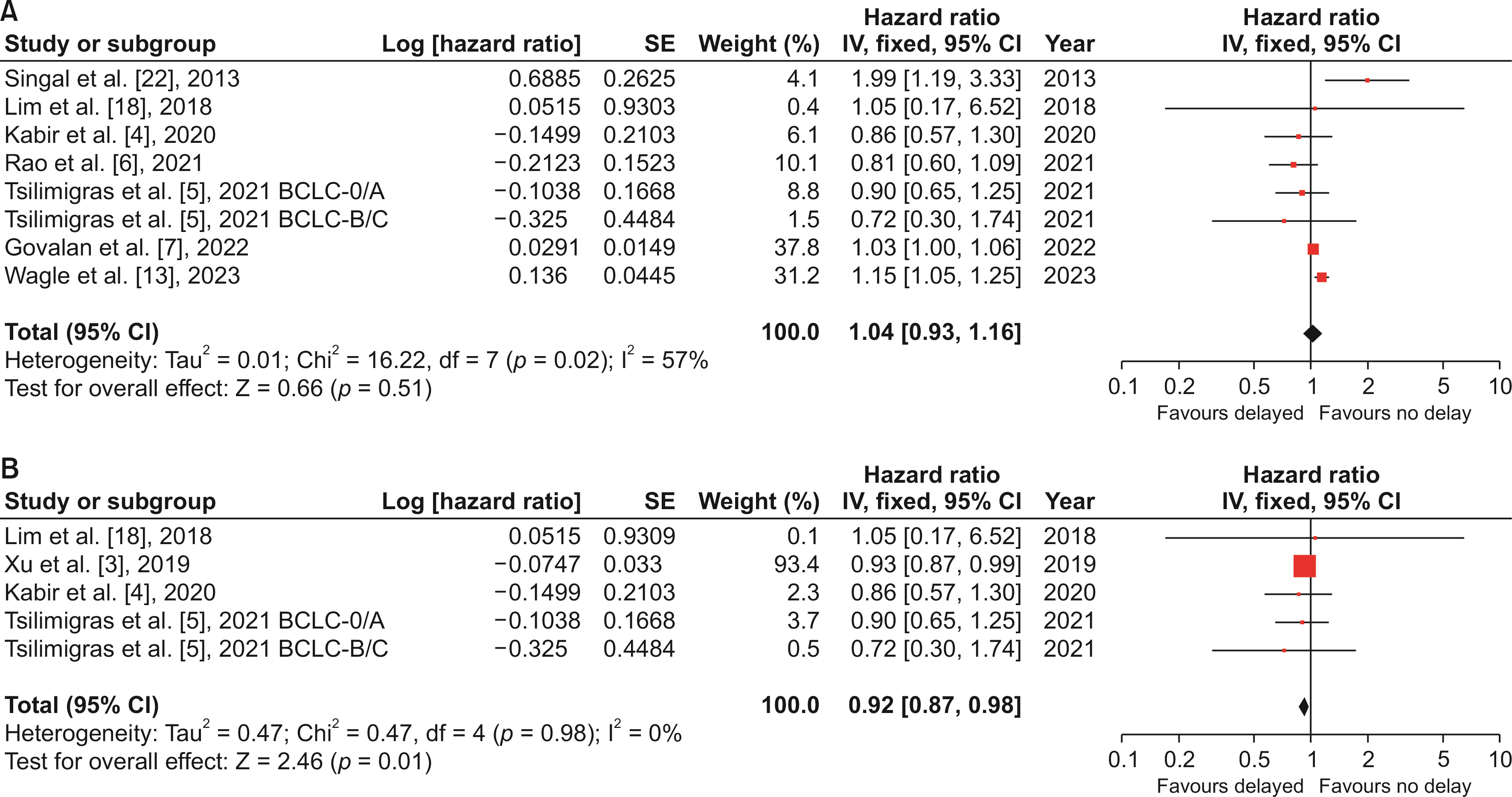
- Hepatocellular carcinoma (HCC) is the sixth most diagnosed cancer worldwide. Healthcare resource constraints may predispose treatment delays. We aim to review existing literature on whether delayed treatment results in worse outcomes in HCC. PubMed, Embase, The Cochrane Library, and Scopus were systematically searched from inception till December 2022. Primary outcomes were overall survival (OS) and disease-free survival (DFS). Secondary outcomes included post-treatment mortality, readmission rates, and complications. Fourteen studies with a total of 135,389 patients (delayed n = 25,516, no delay n = 109,873) were included. Age, incidence of male patients, Child–Pugh B cirrhosis, and Barcelona Clinic Liver Cancer Stage 0/A HCC were comparable between delayed and no delay groups. Tumor size was significantly smaller in delayed versus no delay group (mean difference, –0.70 cm; 95% confidence interval [CI]: –1.14, 0.26; p = 0.002). More patients received radiofrequency ablation in delayed versus no delay group (OR, 1.22; 95% CI: 1.16, 1.27; p < 0.0001). OS was comparable between delayed and no delay in HCC treatment (hazard ratio [HR], 1.13; 95% CI: 0.99, 1.29; p = 0.07). Comparable DFS between delayed and no delay groups (HR, 0.99; 95% CI: 0.75, 1.30; p = 0.95) was observed. Subgroup analysis of studies that defined treatment delay as > 90 days showed comparable OS in the delayed group (HR, 1.04; 95% CI: 0.93, 1.16; p = 0.51). OS and DFS for delayed treatment were non-inferior compared to no delay, but might be due to better tumor biology/smaller tumor size in the delayed group.
Figure
Reference
-
References
1. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021; 71:209–249. DOI: 10.3322/caac.21660. PMID: 33538338.
Article2. Liao YY, Ou J, Luo CP, Peng NF, Zhong JH. 2018; Does delayed treatment affect the survival of patients with hepatocellular carcinoma? Transl Cancer Res. 7:E14–E16. DOI: 10.21037/tcr.2018.04.08.
Article3. Xu K, Watanabe-Galloway S, Rochling FA, Farazi PA, Monirul Islam KM, Wang H, et al. 2019; Surgical delay is associated with improved survival in hepatocellular carcinoma: results of the National Cancer Database. J Gastrointest Surg. 23:933–943. DOI: 10.1007/s11605-018-3925-4. PMID: 30328070.
Article4. Kabir T, Syn N, Ramkumar M, Yeo EYJ, Teo JY, Koh YX, et al. 2020; Effect of surgical delay on survival outcomes in patients undergoing curative resection for primary hepatocellular carcinoma: inverse probability of treatment weighting using propensity scores and propensity score adjustment. Surgery. 167:417–424. DOI: 10.1016/j.surg.2019.09.022. PMID: 31677800.
Article5. Tsilimigras DI, Hyer JM, Diaz A, Moris D, Bagante F, Ratti F, et al. 2021; Impact of time-to-surgery on outcomes of patients undergoing curative-intent liver resection for BCLC-0, A and B hepatocellular carcinoma. J Surg Oncol. 123:381–388. DOI: 10.1002/jso.26297. PMID: 33174627.
Article6. Rao A, Rich NE, Marrero JA, Yopp AC, Singal AG. 2021; Singal, diagnostic and therapeutic delays in patients with hepatocellular carcinoma. J Natl Compr Canc Netw. 19:1063–1071. DOI: 10.6004/jnccn.2020.7689. PMID: 34077908.
Article7. Govalan R, Luu M, Lauzon M, Kosari K, Ahn JC, Rich NE, et al. 2022; Therapeutic underuse and delay in hepatocellular carcinoma: prevalence, associated factors, and clinical impact. Hepatol Commun. 6:223–236. DOI: 10.1002/hep4.1795. PMID: 34558830. PMCID: PMC8710787.
Article8. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. 2021; The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 372:n71. DOI: 10.1136/bmj.n71. PMID: 33782057. PMCID: PMC8005924.9. Lo CK, Mertz D, Loeb M. 2014; Newcastle-Ottawa Scale: comparing reviewers' to authors' assessments. BMC Med Res Methodol. 14:45. DOI: 10.1186/1471-2288-14-45. PMID: 24690082. PMCID: PMC4021422.
Article10. Wan X, Wang W, Liu J, Tong T. 2014; Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 14:135. DOI: 10.1186/1471-2288-14-135. PMID: 25524443. PMCID: PMC4383202.
Article11. Parmar MK, Torri V, Stewart L. 1998; Extracting summary statistics to perform meta-analyses of the published literature for survival endpoints. Stat Med. 17:2815–2834. DOI: 10.1002/(SICI)1097-0258(19981230)17:24<2815::AID-SIM110>3.0.CO;2-8.
Article12. Tierney JF, Stewart LA, Ghersi D, Burdett S, Sydes MR. 2007; Practical methods for incorporating summary time-to-event data into meta- analysis. Trials. 8:16. DOI: 10.1186/1745-6215-8-16. PMID: 17555582. PMCID: PMC1920534.13. Wagle NS, Park S, Washburn D, Ohsfeldt RL, Rich NE, Singal AG, et al. 2023; Racial, ethnic, and socioeconomic disparities in treatment delay among patients with hepatocellular carcinoma in the United States. Clin Gastroenterol Hepatol. 21:1281–1292.e10. DOI: 10.1016/j.cgh.2022.07.031. PMID: 35933076.
Article14. Singal AG, Waljee AK, Patel N, Chen EY, Tiro JA, Marrero JA, et al. 2013; Therapeutic delays lead to worse survival among patients with hepatocellular carcinoma. J Natl Compr Canc Netw. 11:1101–1108. DOI: 10.6004/jnccn.2013.0131. PMID: 24029125. PMCID: PMC5568242.
Article15. Tsai WC, Kung PT, Wang YH, Kuo WY, Li YH. 2018; Influence of the time interval from diagnosis to treatment on survival for early-stage liver cancer. PLoS One. 13:e0199532. DOI: 10.1371/journal.pone.0199532. PMID: 29933395. PMCID: PMC6014663.
Article16. He Y, Liang T, Mo S, Chen Z, Zhao S, Zhou X, et al. 2021; Effect of timing of surgical resection of primary hepatocellular carcinoma on survival outcomes in elderly patients and prediction of clinical models. BMC Gastroenterol. 21:230. DOI: 10.1186/s12876-021-01815-4. PMID: 34020603. PMCID: PMC8139139.
Article17. Huo TI, Huang YH, Chiang JH, Wu JC, Lee PC, Chi CW, et al. 2007; Survival impact of delayed treatment in patients with hepatocellular carcinoma undergoing locoregional therapy: is there a lead-time bias? Scand J Gastroenterol. 42:485–492. DOI: 10.1080/00365520600931402. PMID: 17454859.
Article18. Lim C, Bhangui P, Salloum C, Gómez-Gavara C, Lahat E, Luciani A, et al. 2018; Impact of time to surgery in the outcome of patients with liver resection for BCLC 0-A stage hepatocellular carcinoma. J Hepatol. 68:100–108. DOI: 10.1016/j.jhep.2017.09.017. PMID: 28989094.
Article19. Ong DY, Lee ZY, Pua U. 2022; Impact of waiting time on hepatocellular carcinoma progression in patients undergoing curative tumour ablation. Quant Imaging Med Surg. 12:1499–1504. DOI: 10.21037/qims-20-1411. PMID: 35111642. PMCID: PMC8739106.
Article20. Brahmania M, Ahmed O, Kelley M, Wong D, Kowgier M, Khalili K, et al. 2017; Wait time for curative intent radio frequency ablation is associated with increased mortality in patients with early stage hepatocellular carcinoma. Ann Hepatol. 16:765–771. DOI: 10.5604/01.3001.0010.2776. PMID: 28809734.
Article21. Chen WT, Fernandes ML, Lin CC, Lin SM. 2011; Delay in treatment of early-stage hepatocellular carcinoma using radiofrequency ablation may impact survival of cirrhotic patients in a surveillance program. J Surg Oncol. 103:133–139. DOI: 10.1002/jso.21797. PMID: 21259246.
Article22. Singal AG, Patel NJ, Marrero JA, Tiro JA, Yopp A. 2013; 794 institution of a multidisciplinary liver tumor clinic reduces therapeutic delays for patients with hepatocellular carcinoma. Gastroenterology. 144:S–961. DOI: 10.1016/S0016-5085(13)63569-6.
Article23. Hanna TP, King WD, Thibodeau S, Jalink M, Paulin GA, Harvey-Jones E, et al. 2020; Mortality due to cancer treatment delay: systematic review and meta-analysis. BMJ. 371:m4087. DOI: 10.1136/bmj.m4087. PMID: 33148535. PMCID: PMC7610021.
Article24. Cone EB, Marchese M, Paciotti M, Nguyen DD, Nabi J, Cole AP, et al. 2020; Assessment of time-to-treatment initiation and survival in a cohort of patients with common cancers. JAMA Netw Open. 3:e2030072. DOI: 10.1001/jamanetworkopen.2020.30072. PMID: 33315115. PMCID: PMC7737088.
Article25. Nathani P, Gopal P, Rich N, Yopp A, Yokoo T, John B, et al. 2021; Hepatocellular carcinoma tumour volume doubling time: a systematic review and meta-analysis. Gut. 70:401–407. DOI: 10.1136/gutjnl-2020-321040. PMID: 32398224. PMCID: PMC7657990.
Article26. Jha RC, Zanello PA, Nguyen XM, Pehlivanova M, Johnson LB, Fishbein T, et al. 2014; Small hepatocellular carcinoma: MRI findings for predicting tumor growth rates. Acad Radiol. 21:1455–1464. DOI: 10.1016/j.acra.2014.06.011. PMID: 25300723.27. An C, Choi YA, Choi D, Paik YH, Ahn SH, Kim MJ, et al. 2015; Growth rate of early-stage hepatocellular carcinoma in patients with chronic liver disease. Clin Mol Hepatol. 21:279–286. DOI: 10.3350/cmh.2015.21.3.279. PMID: 26523271. PMCID: PMC4612289.
Article28. Kim JK, Kim HD, Jun MJ, Yun SC, Shim JH, Lee HC, et al. 2017; Tumor volume doubling time as a dynamic prognostic marker for patients with hepatocellular carcinoma. Dig Dis Sci. 62:2923–2931. DOI: 10.1007/s10620-017-4708-6. PMID: 28815349.
Article29. Park MS. 2014; Early stage hepatocellular carcinoma in Koreans with chronic liver disease: tumor growth rate and 5-year survival. J Hepatol. 60:S534. DOI: 10.1016/S0168-8278(14)61484-7.30. Rich NE, John BV, Parikh ND, Rowe I, Mehta N, Khatri G, et al. 2020; Hepatocellular carcinoma demonstrates heterogeneous growth patterns in a multicenter cohort of patients with cirrhosis. Hepatology. 72:1654–1665. DOI: 10.1002/hep.31159. PMID: 32017165. PMCID: PMC7398837.
Article31. Jones M, Fowler R. 2016; Immortal time bias in observational studies of time-to-event outcomes. J Crit Care. 36:195–199. DOI: 10.1016/j.jcrc.2016.07.017. PMID: 27546771.
Article32. Agarwal P, Moshier E, Ru M, Ohri N, Ennis R, Rosenzweig K, et al. 2018; Immortal time bias in observational studies of time-to-event outcomes: assessing effects of postmastectomy radiation therapy using the National Cancer Database. Cancer Control. 25:1073274818789355. DOI: 10.1177/1073274818789355. PMID: 30021466. PMCID: PMC6053873.33. Yau T, Tang VY, Yao TJ, Fan ST, Lo CM, Poon RT. 2014; Development of Hong Kong Liver Cancer staging system with treatment stratification for patients with hepatocellular carcinoma. Gastroenterology. 146:1691–1700.e3. DOI: 10.1053/j.gastro.2014.02.032. PMID: 24583061.
Article34. Reig M, Forner A, Rimola J, Ferrer-Fàbrega J, Burrel M, Garcia-Criado Á, et al. 2022; BCLC strategy for prognosis prediction and treatment recommendation: the 2022 update. J Hepatol. 76:681–693. DOI: 10.1016/j.jhep.2021.11.018. PMID: 34801630. PMCID: PMC8866082.
Article35. Villanueva A. 2019; Hepatocellular carcinoma. N Engl J Med. 380:1450–1462. DOI: 10.1056/NEJMra1713263. PMID: 30970190.
Article36. Singal AG, Pillai A, Tiro J. 2014; Early detection, curative treatment, and survival rates for hepatocellular carcinoma surveillance in patients with cirrhosis: a meta-analysis. PLoS Med. 11:e1001624. DOI: 10.1371/journal.pmed.1001624. PMID: 24691105. PMCID: PMC3972088.
Article37. Llovet JM, Kelley RK, Villanueva A, Singal AG, Pikarsky E, Roayaie S, et al. 2021; Hepatocellular carcinoma. Nat Rev Dis Primers. 7:6. DOI: 10.1038/s41572-020-00240-3. PMID: 33479224.
Article38. Johnson BA, Waddimba AC, Ogola GO, Fleshman JW Jr, Preskitt JT. 2021; A systematic review and meta-analysis of surgery delays and survival in breast, lung and colon cancers: implication for surgical triage during the COVID-19 pandemic. Am J Surg. 222:311–318. DOI: 10.1016/j.amjsurg.2020.12.015. PMID: 33317814. PMCID: PMC7834494.
Article39. Wang B, Shelat VG, Chow JJL, Huey TCW, Low JK, Woon WWL, et al. 2020; Prehabilitation program improves outcomes of patients undergoing elective liver resection. J Surg Res. 251:119–125. DOI: 10.1016/j.jss.2020.01.009. PMID: 32135382.
Article40. Chan KS, Low JK, Shelat VG. 2020; Associated liver partition and portal vein ligation for staged hepatectomy: a review. Transl Gastroenterol Hepatol. 5:37. DOI: 10.21037/tgh.2019.12.01. PMID: 32632388. PMCID: PMC7063517.
Article41. Liang BY, Gu J, Xiong M, Zhang EL, Zhang ZY, Chen XP, et al. 2021; Tumor size may influence the prognosis of solitary hepatocellular carcinoma patients with cirrhosis and without macrovascular invasion after hepatectomy. Sci Rep. 11:16343. DOI: 10.1038/s41598-021-95835-5. PMID: 34381132. PMCID: PMC8357938.
Article42. Menahem B, Lubrano J, Duvoux C, Mulliri A, Alves A, Costentin C, et al. 2017; Liver transplantation versus liver resection for hepatocellular carcinoma in intention to treat: an attempt to perform an ideal meta-analysis. Liver Transpl. 23:836–844. DOI: 10.1002/lt.24758. PMID: 28295992.
Article43. Kamath PS, Kim WR. Advanced Liver Disease Study Group. 2007; The model for end-stage liver disease (MELD). Hepatology. 45:797–805. DOI: 10.1002/hep.21563. PMID: 17326206.
Article44. Mehta N, Dodge JL, Hirose R, Roberts JP, Yao FY. 2019; Predictors of low risk for dropout from the liver transplant waiting list for hepatocellular carcinoma in long wait time regions: implications for organ allocation. Am J Transplant. 19:2210–2218. DOI: 10.1111/ajt.15353. PMID: 30861298. PMCID: PMC7072024.
Article45. Tan CHN, Yu Y, Tan YRN, Lim BLK, Iyer SG, Madhavan K, et al. 2018; Bridging therapies to liver transplantation for hepatocellular carcinoma: a bridge to nowhere? Ann Hepatobiliary Pancreat Surg. 22:27–35. DOI: 10.14701/ahbps.2018.22.1.27. PMID: 29536053. PMCID: PMC5845608.
Article46. Kwong AJ, Ebel NH, Kim WR, Lake JR, Smith JM, Schladt DP, et al. 2022; OPTN/SRTR 2020 annual data report: liver. Am J Transplant. 22 Suppl 2:204–309. DOI: 10.1111/ajt.16978. PMID: 35266621.
Article47. Kanwal F, Hernaez R, Liu Y, Taylor TJ, Rana A, Kramer JR, et al. 2021; Factors associated with access to and receipt of liver transplantation in veterans with end-stage liver disease. JAMA Inter Med. 181:949–959. DOI: 10.1001/jamainternmed.2021.2051. PMID: 34028505. PMCID: PMC8145153.
Article48. Klassen AC, Klassen DK, Brookmeyer R, Frank RG, Marconi K. 1998; Factors influencing waiting time and successful receipt of cadaveric liver transplant in the United States. 1990 to 1992. Med Care. 36:281–294. DOI: 10.1097/00005650-199803000-00006. PMID: 9520954.
Article49. Liver transplant: National University Hospital. Diseases & Conditions (n.d.). Available from: https://www.nuh.com.sg/Health-Information/Diseases-Conditions/Pages/Liver-Transplant.aspx. 2023. cited 2023 April 6.50. Mehta N, Heimbach J, Lee D, Dodge JL, Harnois D, Burns J, et al. Wait time of less than 6 and greater than 18 months predicts hepatocellular carcinoma recurrence after liver transplantation: proposing a wait time "sweet spot.". Transplantation. 2017; 101:2071–2078. DOI: 10.1097/TP.0000000000001752. PMID: 28353492. PMCID: PMC5568965.
Article51. Schlansky B, Chen Y, Scott DL, Austin D, Naugler WE. 2014; Waiting time predicts survival after liver transplantation for hepatocellular carcinoma: a cohort study using the United Network for Organ Sharing registry. Liver Transpl. 20:1045–1056. DOI: 10.1002/lt.23917. PMID: 24838471.
Article52. Halazun KJ, Patzer RE, Rana AA, Verna EC, Griesemer AD, Parsons RF, et al. 2014; Standing the test of time: outcomes of a decade of prioritizing patients with hepatocellular carcinoma, results of the UNOS natural geographic experiment. Hepatology. 60:1957–1962. DOI: 10.1002/hep.27272. PMID: 24954365.
Article53. Roberts JP, Venook A, Kerlan R, Yao F. 2010; Hepatocellular carcinoma: ablate and wait versus rapid transplantation. Liver Transpl. 16:925–929. DOI: 10.1002/lt.22103. PMID: 20658555.
Article54. McGlynn KA, Petrick JL, London WT. 2015; Global epidemiology of hepatocellular carcinoma: an emphasis on demographic and regional variability. Clin Liver Dis. 19:223–238. DOI: 10.1016/j.cld.2015.01.001. PMID: 25921660. PMCID: PMC4712629.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- An Introduction of the Systematic Review and Meta-Analysis
- Comparison of Radioembolization and Sorafenib for the Treatment of Hepatocellular Carcinoma with Portal Vein Tumor Thrombosis: A Systematic Review and Meta-Analysis of Safety and Efficacy
- Critical Appraisal of Systematic Review/Meta-analysis
- Concepts and emerging issues of network meta-analysis
- Introduction to systematic review and meta-analysis