J Korean Med Sci.
2024 Mar;39(8):e80. 10.3346/jkms.2024.39.e80.
Mildly Reduced Renal Function Is Associated With Increased Heart Failure Admissions in Patients With Hypertrophic Cardiomyopathy
- Affiliations
-
- 1Department of Internal Medicine, Seoul National University Hospital, Seoul, Korea
- 2Department of Internal Medicine, Healthcare System Gangnam Center, Seoul National University Hospital, Seoul, Korea
- 3Department of Internal Medicine, Korea University Guro Hospital, Seoul, Korea
- 4Cardiovascular Center and Department of Internal Medicine, Seoul National University Bundang Hospital, Seongnam, Korea
- KMID: 2553329
- DOI: http://doi.org/10.3346/jkms.2024.39.e80
Abstract
- Background
The association between renal dysfunction and cardiovascular outcomes has yet to be determined in patients with hypertrophic cardiomyopathy (HCM). We aimed to investigate whether mildly reduced renal function is associated with the prognosis in patients with HCM.
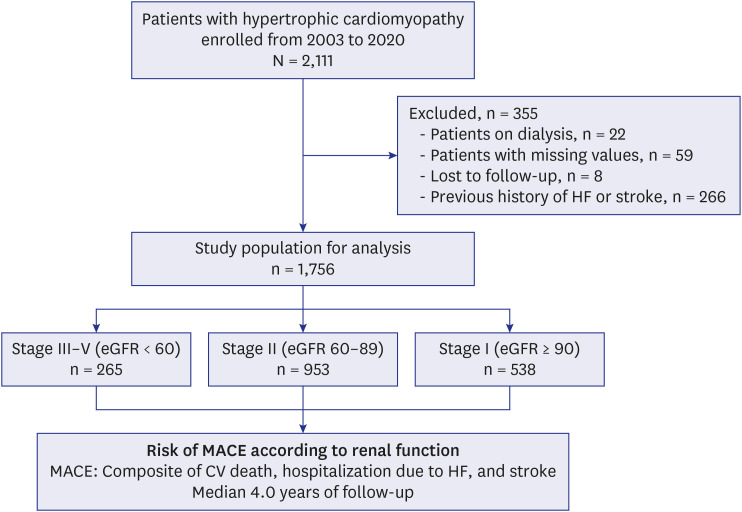
Methods
Patients with HCM were enrolled at two tertiary HCM centers. Patients who were on dialysis, or had a previous history of heart failure (HF) or stroke were excluded. Patients were categorized into 3 groups by estimated glomerular filtration rate (eGFR): stage I (eGFR ≥ 90 mL/min/1.73 m2 , n = 538), stage II (eGFR 60–89 mL/min/1.73 m2 , n = 953), and stage III–V (eGFR < 60 mL/min/1.73 m2 , n = 265). Major adverse cardiovascular events (MACEs) were defined as a composite of cardiovascular death, hospitalization for HF (HHF), or stroke during median 4.0-year follow-up. Multivariable Cox regression model was used to adjust for covariates.
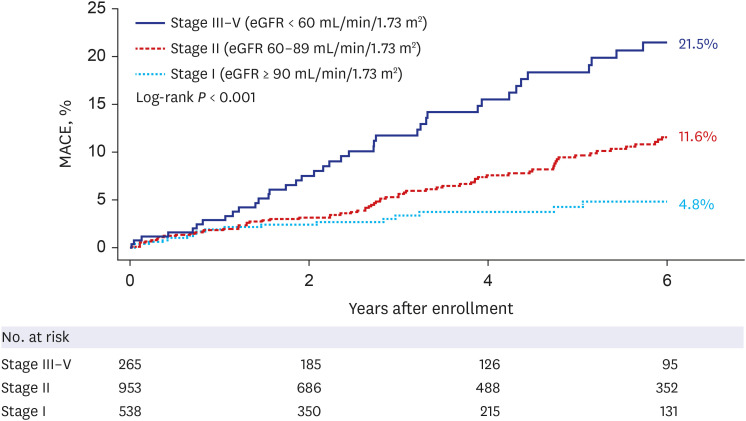
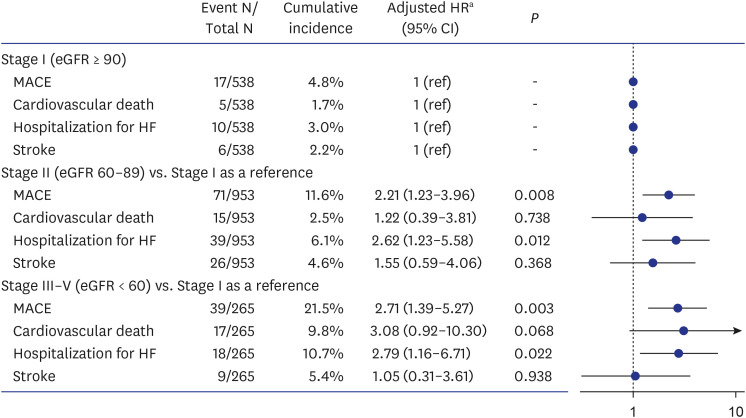
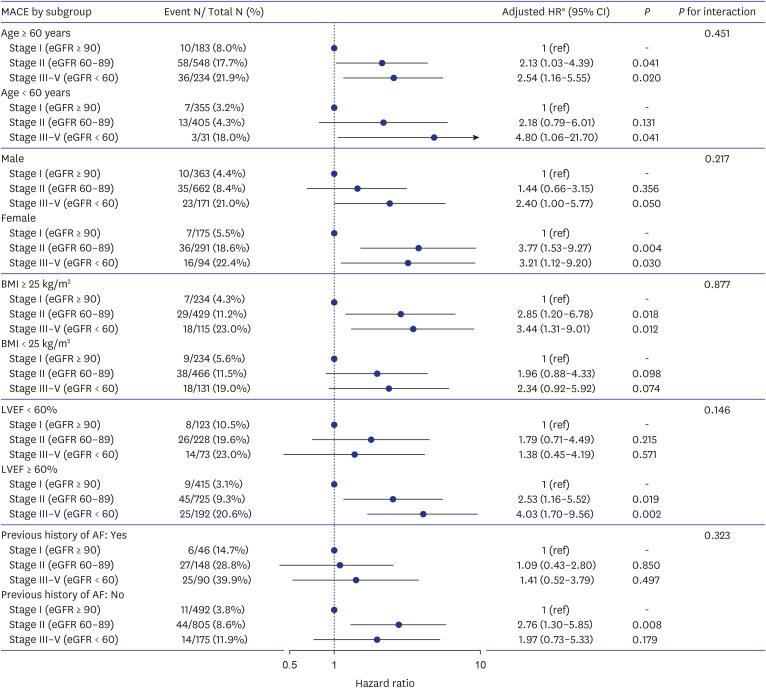
Results
Among 1,756 HCM patients (mean 61.0 ± 13.4 years; 68.1% men), patients with stage III–V renal function had a significantly higher risk of MACEs (adjusted hazard ratio [aHR], 2.71; 95% confidence interval [CI], 1.39–5.27; P = 0.003), which was largely driven by increased incidence of cardiovascular death and HHF compared to those with stage I renal function. Even in patients with stage II renal function, the risk of MACE (vs. stage I: aHR, 2.21’ 95% CI, 1.23–3.96; P = 0.008) and HHF (vs. stage I: aHR, 2.62; 95% CI, 1.23–5.58; P = 0.012) was significantly increased.
Conclusion
This real-world observation showed that even mildly reduced renal function (i.e., eGFR 60–89 mL/min/1.73 m2 ) in patients with HCM was associated with an increased risk of MACEs, especially for HHF.
Keyword
Figure
Reference
-
1. Marian AJ, Braunwald E. Hypertrophic cardiomyopathy: genetics, pathogenesis, clinical manifestations, diagnosis, and therapy. Circ Res. 2017; 121(7):749–770. PMID: 28912181.2. Ommen SR, Mital S, Burke MA, Day SM, Deswal A, Elliott P, et al. 2020 AHA/ACC guideline for the diagnosis and treatment of patients with hypertrophic cardiomyopathy: a report of the American College of Cardiology/American Heart Association joint committee on clinical practice guidelines. Circulation. 2020; 142(25):e558–e631. PMID: 33215931.3. Authors/Task Force members. Elliott PM, Anastasakis A, Borger MA, Borggrefe M, Cecchi F, et al. 2014 ESC guidelines on diagnosis and management of hypertrophic cardiomyopathy: the Task Force for the Diagnosis and Management of Hypertrophic Cardiomyopathy of the European Society of Cardiology (ESC). Eur Heart J. 2014; 35(39):2733–2779. PMID: 25173338.4. Lee HJ, Kim J, Chang SA, Kim YJ, Kim HK, Lee SC. Major clinical issues in hypertrophic cardiomyopathy. Korean Circ J. 2022; 52(8):563–575. PMID: 35929051.5. Song MK, Baek SM, Kim GB, Lee SY, Kwon HW, Lee HJ, et al. Relationship between life-threatening events and electromechanical window in patients with hypertrophic cardiomyopathy: a novel parameter for risk stratification of sudden cardiac death. Heart Rhythm. 2022; 19(4):588–594. PMID: 34933113.6. Gansevoort RT, Correa-Rotter R, Hemmelgarn BR, Jafar TH, Heerspink HJ, Mann JF, et al. Chronic kidney disease and cardiovascular risk: epidemiology, mechanisms, and prevention. Lancet. 2013; 382(9889):339–352. PMID: 23727170.7. Lee H, Han K, Park JB, Hwang IC, Yoon YE, Park HE, et al. Risk of end-stage renal disease in patients with hypertrophic cardiomyopathy: a nationwide population-based cohort study. Sci Rep. 2019; 9(1):14565. PMID: 31601873.8. Manjunath G, Tighiouart H, Coresh J, Macleod B, Salem DN, Griffith JL, et al. Level of kidney function as a risk factor for cardiovascular outcomes in the elderly. Kidney Int. 2003; 63(3):1121–1129. PMID: 12631096.9. Anavekar NS, McMurray JJ, Velazquez EJ, Solomon SD, Kober L, Rouleau JL, et al. Relation between renal dysfunction and cardiovascular outcomes after myocardial infarction. N Engl J Med. 2004; 351(13):1285–1295. PMID: 15385655.10. Ataklte F, Song RJ, Upadhyay A, Musa Yola I, Vasan RS, Xanthakis V. Association of mildly reduced kidney function with cardiovascular disease: the Framingham Heart Study. J Am Heart Assoc. 2021; 10(16):e020301. PMID: 34387110.11. Cerasola G, Nardi E, Palermo A, Mulè G, Cottone S. Epidemiology and pathophysiology of left ventricular abnormalities in chronic kidney disease: a review. J Nephrol. 2011; 24(1):1–10. PMID: 20437402.12. Gori M, Senni M, Gupta DK, Charytan DM, Kraigher-Krainer E, Pieske B, et al. Association between renal function and cardiovascular structure and function in heart failure with preserved ejection fraction. Eur Heart J. 2014; 35(48):3442–3451. PMID: 24980489.13. Lee HJ, Kim HK, Lee SC, Kim J, Park JB, Hwang IC, et al. Supplementary role of left ventricular global longitudinal strain for predicting sudden cardiac death in hypertrophic cardiomyopathy. Eur Heart J Cardiovasc Imaging. 2022; 23(8):1108–1116. PMID: 34542591.14. Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Ann Intern Med. 1999; 130(6):461–470. PMID: 10075613.15. Stevens PE, Levin A. Kidney Disease: Improving Global Outcomes Chronic Kidney Disease Guideline Development Work Group Members. Evaluation and management of chronic kidney disease: synopsis of the kidney disease: improving global outcomes 2012 clinical practice guideline. Ann Intern Med. 2013; 158(11):825–830. PMID: 23732715.16. Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015; 28(1):1–39.e14. PMID: 25559473.17. Lee HJ, Kim HK, Lee SC, Ommen SR, Kim J, Park JB, et al. Age-related sex differences in the outcomes of patients with hypertrophic cardiomyopathy. PLoS One. 2022; 17(2):e0264580. PMID: 35213653.18. Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, et al. 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC): developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016; 37(27):2129–2200. PMID: 27206819.19. Sacco RL, Kasner SE, Broderick JP, Caplan LR, Connors JJ, Culebras A, et al. An updated definition of stroke for the 21st century: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013; 44(7):2064–2089. PMID: 23652265.20. Choi YJ, Kim HK, Hwang IC, Park CS, Rhee TM, Lee HJ, et al. Prognosis of patients with hypertrophic cardiomyopathy and low-normal left ventricular ejection fraction. Heart. 2023; 109(10):771–778. PMID: 36581445.21. Huang FY, Zhang JL, Huang BT, Peng Y, Chen SJ, Chen M. Renal function as a predictor of outcomes in patients with hypertrophic cardiomyopathy: a cohort study of a hospitalized population. Clin Chim Acta. 2021; 512:92–99. PMID: 33279500.22. Higuchi S, Minami Y, Shoda M, Shirotani S, Kanai M, Kataoka S, et al. Effect of renal dysfunction on risk of sudden cardiac death in patients with hypertrophic cardiomyopathy. Am J Cardiol. 2021; 144:131–136. PMID: 33383012.23. Kwon S, Kim HK, Kim B, Lee HJ, Han KD, Hwang IC, et al. Comparison of mortality and cause of death between adults with and without hypertrophic cardiomyopathy. Sci Rep. 2022; 12(1):6386. PMID: 35430580.24. Melacini P, Basso C, Angelini A, Calore C, Bobbo F, Tokajuk B, et al. Clinicopathological profiles of progressive heart failure in hypertrophic cardiomyopathy. Eur Heart J. 2010; 31(17):2111–2123. PMID: 20513729.25. Mullens W, Damman K, Testani JM, Martens P, Mueller C, Lassus J, et al. Evaluation of kidney function throughout the heart failure trajectory - a position statement from the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail. 2020; 22(4):584–603. PMID: 31908120.26. Coresh J, Selvin E, Stevens LA, Manzi J, Kusek JW, Eggers P, et al. Prevalence of chronic kidney disease in the United States. JAMA. 2007; 298(17):2038–2047. PMID: 17986697.27. Kim TO, Kang DY, Ahn JM, Kim SO, Lee PH, Lee J, et al. Prognostic impact of mildly impaired renal function in patients undergoing multivessel coronary revascularization. J Am Coll Cardiol. 2022; 79(13):1270–1284. PMID: 35361350.28. Tbahriti HF, Meknassi D, Moussaoui R, Messaoudi A, Zemour L, Kaddous A, et al. Inflammatory status in chronic renal failure: the role of homocysteinemia and pro-inflammatory cytokines. World J Nephrol. 2013; 2(2):31–37. PMID: 24175263.29. Mihai S, Codrici E, Popescu ID, Enciu AM, Albulescu L, Necula LG, et al. Inflammation-related mechanisms in chronic kidney disease prediction, progression, and outcome. J Immunol Res. 2018; 2018:2180373. PMID: 30271792.30. Suh-Chiou C, Moysés RM, Bittencourt MS, Bensenor IM, Lotufo PA. Chronic kidney disease and coronary artery calcification in the Brazilian Longitudinal Study of Adult Health (ELSA-Brasil). Clin Cardiol. 2017; 40(12):1309–1315. PMID: 29243272.31. Budoff MJ, Rader DJ, Reilly MP, Mohler ER 3rd, Lash J, Yang W, et al. Relationship of estimated GFR and coronary artery calcification in the CRIC (Chronic Renal Insufficiency Cohort) Study. Am J Kidney Dis. 2011; 58(4):519–526. PMID: 21783289.32. Maron BJ, Rowin EJ, Udelson JE, Maron MS. Clinical spectrum and management of heart failure in hypertrophic cardiomyopathy. JACC Heart Fail. 2018; 6(5):353–363. PMID: 29655822.33. Heidenreich PA, Bozkurt B, Aguilar D, Allen LA, Byun JJ, Colvin MM, et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association joint committee on clinical practice guidelines. Circulation. 2022; 145(18):e895–1032. PMID: 35363499.34. Yau K, Dharia A, Alrowiyti I, Cherney DZ. Prescribing SGLT2 inhibitors in patients with CKD: expanding indications and practical considerations. Kidney Int Rep. 2022; 7(7):1463–1476. PMID: 35812300.35. van Driel B, Nijenkamp L, Huurman R, Michels M, van der Velden J. Sex differences in hypertrophic cardiomyopathy: new insights. Curr Opin Cardiol. 2019; 34(3):254–259. PMID: 30747730.36. Jousilahti P, Vartiainen E, Tuomilehto J, Puska P. Sex, age, cardiovascular risk factors, and coronary heart disease: a prospective follow-up study of 14 786 middle-aged men and women in Finland. Circulation. 1999; 99(9):1165–1172. PMID: 10069784.37. Regitz-Zagrosek V, Kararigas G. Mechanistic pathways of sex differences in cardiovascular disease. Physiol Rev. 2017; 97(1):1–37. PMID: 27807199.38. Park JB, Kim DH, Lee H, Hwang IC, Yoon YE, Park HE, et al. Obesity and metabolic health status are determinants for the clinical expression of hypertrophic cardiomyopathy. Eur J Prev Cardiol. 2020; 27(17):1849–1857. PMID: 31787021.39. Chen Z, Xu B. Clinical significance of overweight in patients with hypertrophic cardiomyopathy: a retrospective cohort study. Medicine (Baltimore). 2021; 100(40):e27445. PMID: 34622863.40. Shi K, Huang S, Li X, Xu HY, Yang MX, Li Y, et al. Effect of obesity on left ventricular remodeling and clinical outcome in Chinese patients with hypertrophic cardiomyopathy: assessed by cardiac MRI. J Magn Reson Imaging. 2023; 57(3):800–809. PMID: 35715897.41. Walther CP, Benoit JS, Gregg LP, Bansal N, Nambi V, Feldman HI, et al. Heart failure-type symptom scores in chronic kidney disease: the importance of body mass index. Int J Obes (Lond). 2022; 46(10):1910–1917. PMID: 35978101.42. Chamberlain AM, Redfield MM, Alonso A, Weston SA, Roger VL. Atrial fibrillation and mortality in heart failure: a community study. Circ Heart Fail. 2011; 4(6):740–746. PMID: 21920917.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Maternally Inherited Familial Hypertrophic Cardiomyopathy Manifested by Pregnancy Related Early Progression and Sudden Cardiac Death
- The Echocardiographic Study on the 13 Patients with the Hypertrophic Cardiomyopathy
- A Case of Congenital Hypertrophic Cardiomyopathy
- A case of hypertrophic obstructive cardiomyopathy complicated by infective endocarditis and treated by surgical intervention
- A Comparative Study of Left Ventricular Diastolic Function between Hypertrophic Cardiomyopathy and Hypertensive Patients with Left Ventricular Hypertrophy