J Korean Med Sci.
2024 Feb;39(7):e62. 10.3346/jkms.2024.39.e62.
Do Death Certificate Errors Decrease as Clinical Experience in an Emergency Department Increases?
- Affiliations
-
- 1Department of Emergency Medicine, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Korea
- 2Department of Emergency Medicine, Dong-A University Hospital, Dong-A University College of Medicine, Busan, Korea
- KMID: 2553315
- DOI: http://doi.org/10.3346/jkms.2024.39.e62
Abstract
- Background
This study aimed to evaluate the relationship between clinical experience and death certificate (DC) errors by analyzing DCs written by experienced emergency physicians (EPs).
Methods
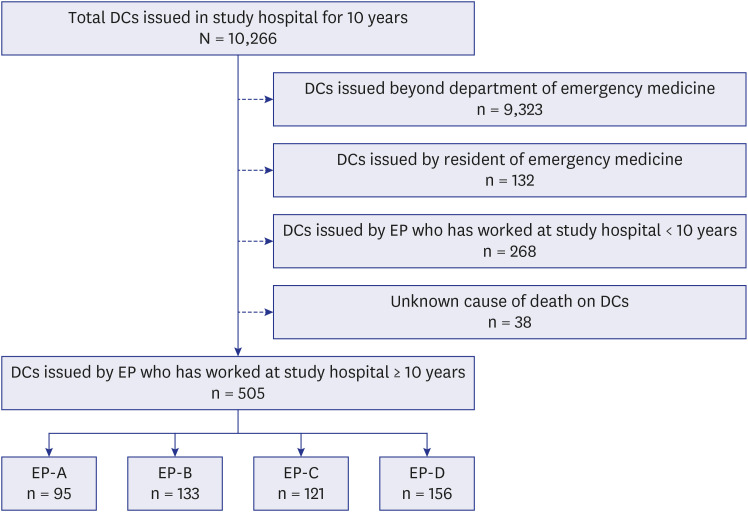
DCs issued by four experienced EPs over a 10-year period were retrospectively reviewed. DC errors were divided into major and minor errors based on whether they affected the cause of death (COD) determination. The errors were judged through first and second evaluations. Basic information regarding DCs and 10-year changes in DC errors were analyzed.
Results
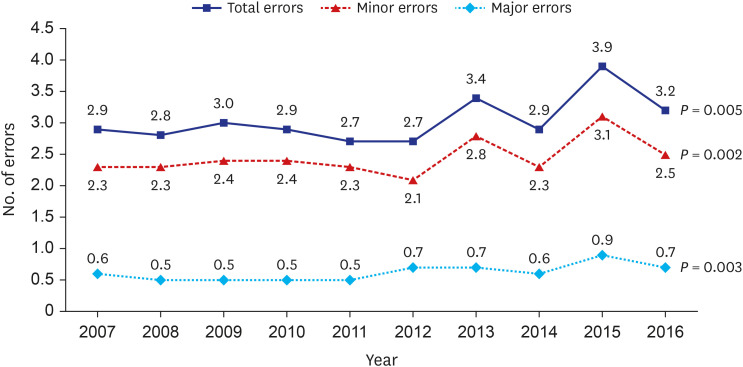
A total of 505 DCs were analyzed, with an average of 34 to 70 for each study year. The number of CODs written in the DCs tended to decrease over time. The presentation of major DC errors did not show a tendency to change over time. However, the sum of the major and minor errors tended to increase over time. Secondary conditions as the underlying COD tended to increase, and the incompatible causal relationships between CODs tended to decrease over time in the detailed analysis of major errors. The increasing tendency for incorrect other significant conditions, incorrect type of accident, incorrect intention of the external cause, no record of the trauma mechanism, and record of the trauma mechanism without another COD were found in the detailed analysis of minor errors.
Conclusion
DC errors did not decrease as clinical experience increased. Education to reduce DC errors and a feedback process for written DCs are necessary, regardless of clinical experience.
Figure
Reference
-
1. Akakpo PK, Awuku YA, Derkyi-Kwarteng L, Gyamera KA, Eliason S. Review of errors in the issue of medical certificates of cause of death in a tertiary hospital in Ghana. Ghana Med J. 2017; 51(1):30–35. PMID: 28959070.2. Alipour J, Payandeh A. Common errors in reporting cause-of-death statement on death certificates: a systematic review and meta-analysis. J Forensic Leg Med. 2021; 82:102220. PMID: 34325081.3. Ben Khelil M, Kamel M, Lahmar S, Mrabet A, Borsali Falfoul N, Hamdoun M. Death certificate accuracy in a Tunisian emergency department. Tunis Med. 2017; 95(6):422–428. PMID: 29512798.4. Burger EH, van der Merwe L, Volmink J. Errors in the completion of the death notification form. S Afr Med J. 2007; 97(11):1077–1081. PMID: 18250917.5. Chang JH, Kim SH, Lee H, Choi B. Analysis of errors on death certificate for trauma related death. J Trauma Inj. 2019; 32(3):127–135.6. Chung S, Kim SH, Park BJ, Park S. Factors associated with major errors on death certificates. Healthcare (Basel). 2022; 10(4):726. PMID: 35455903.7. Fernando D, Oxley JD, Nottingham J. Death certification: do consultant pathologists do it better? J Clin Pathol. 2012; 65(10):949–951. PMID: 22774219.8. Filippatos G, Andriopoulos P, Panoutsopoulos G, Zyga S, Souliotis K, Gennimata V, et al. The quality of death certification practice in Greece. Hippokratia. 2016; 20(1):19–25. PMID: 27895438.9. Katsakiori PF, Panagiotopoulou EC, Sakellaropoulos GC, Papazafiropoulou A, Kardara M. Errors in death certificates in a rural area of Greece. Rural Remote Health. 2007; 7(4):822. PMID: 18067402.10. Lee H, Kim SH, Choi B, Ock M, Park EJ. Concordance between the underlying causes of death on death certificates written by three emergency physicians. Clin Exp Emerg Med. 2019; 6(3):218–225. PMID: 31571438.11. Lu TH, Shau WY, Shih TP, Lee MC, Chou MC, Lin CK. Factors associated with errors in death certificate completion. A national study in Taiwan. J Clin Epidemiol. 2001; 54(3):232–238. PMID: 11223320.12. Maharjan L, Shah A, Shrestha KB, Shrestha G. Errors in cause-of-death statement on death certificates in intensive care unit of Kathmandu, Nepal. BMC Health Serv Res. 2015; 15(1):507. PMID: 26563325.13. McGivern L, Shulman L, Carney JK, Shapiro S, Bundock E. Death certification errors and the effect on mortality statistics. Public Health Rep. 2017; 132(6):669–675. PMID: 29091542.14. Myers KA, Farquhar DR. Improving the accuracy of death certification. CMAJ. 1998; 158(10):1317–1323. PMID: 9614825.15. Park BJ, Kim SH. Errors in pediatric death certificates issued in an emergency department. Pediatr Emerg Med J. 2022; 9(1):17–22.16. Park CH, Kim SH. Errors of death certificate for poisoning related death. J Korean Soc Clin Toxicol. 2020; 18(1):11–17.17. Park S, Kim SH. Does the application of international classification of disease codes for the cause of death on death certificates reduce garbage codes? Inquiry. 2022; 59:469580221081433. PMID: 35384751.18. Schuppener LM, Olson K, Brooks EG. Death certification: errors and interventions. Clin Med Res. 2020; 18(1):21–26. PMID: 31597655.19. Kim HG, Park JW, Cho WY, Seo JH, Choi CH, Na JY. The discrepancy of the cause and manner of death between death certificates and autopsy reports. Korean J Leg Med. 2014; 38(4):139–144.20. Yoon SH, Kim R, Lee CS. Analysis of death certificate errors of a university hospital emergency room. Korean J Leg Med. 2017; 41(3):61–66.21. Lakkireddy DR, Gowda MS, Murray CW, Basarakodu KR, Vacek JL. Death certificate completion: how well are physicians trained and are cardiovascular causes overstated? Am J Med. 2004; 117(7):492–498. PMID: 15464706.22. Kang E, Lee H, Kim SH. The effect of education on ‘how to write the death certificate’ for resident trainees of the emergency department. J Korean Soc Emerg Med. 2018; 29(5):529–550.23. Mikkelsen L, Richards N, Lopez A. Redefining ‘Garbage Codes’ for Public Health Policy: Report on the Expert Group Meeting, 27-28 February 2017. Melbourne, Australia: University of Melbourne;2018.24. Yoo S. Determination of cause and manner of death. J Korean Med Assoc. 2018; 1975(8456):2093–5951.25. Korean Medical Association. How to Write and Issue Medical Certificates. Seoul, Korea: Korean Medical Association;2015. p. 34–53.26. Brämer GR. International statistical classification of diseases and related health problems. Tenth revision. World Health Stat Q. 1988; 41(1):32–36. PMID: 3376487.27. Hanzlick R. Cause of Death and the Death Certificate: Important Information for Physicians, Coroners, Medical Examiners, and The Public. Northfield, IL, USA: College of American Pathologists;2006.28. KOrean Statistical Information Service. Cause of death statistics. Accessed November 27, 2023. https://kosis.kr/index/index.do .29. Pandya H, Bose N, Shah R, Chaudhury N, Phatak A. Educational intervention to improve death certification at a teaching hospital. Natl Med J India. 2009; 22(6):317–319. PMID: 20384023.30. Rogena EA, Waruru A, Young PW, Abade P, Nyagah LM, Walong EO. A review of completeness, correctness, and order of cause of death statements among decedents with documented causes of death and HIV status at two major mortuaries in Kenya, 2015. J Forensic Leg Med. 2020; 73:101993. PMID: 32658751.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Analysis of Death Certificate Errors of a University Hospital Emergency Room
- Analysis of Errors on Death Certificate for Trauma Related Death
- The effect of education on ‘how to write the death certificate’ for resident trainees of the emergency department
- Errors of Death Certificate for Poisoning Related Death
- Concordance between the underlying causes of death on death certificates written by three emergency physicians