Arch Hand Microsurg.
2024 Mar;29(1):1-23. 10.12790/ahm.23.0055.
Congenital hand differences: a comprehensive literature review
- Affiliations
-
- 1Department of Plastic and Reconstructive Surgery, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2553167
- DOI: http://doi.org/10.12790/ahm.23.0055
Abstract
- Upper extremity anomalies are the second most common type of congenital malformations. Approximately 1% to 3% of newborns are born with congenital anomalies, and among them, roughly 10% have upper extremity anomalies. Congenital hand anomalies are often isolated phenomena but may also coexist with other congenital anomalies or syndromes. These anomalies cause not only aesthetic concerns, but also significant functional deficits and psychological issues for children and their families. Surgeons should conduct a thorough examination to make an accurate diagnosis and provide appropriate treatment or refer the patient to a specialized clinic if necessary. Operative procedures should aim to restore both function and aesthetics. This article reviews the embryology of the hand, the classification of congenital hand anomalies, and the clinical features and treatment of common major congenital hand anomalies.
Figure
Reference
-
References
1. Wolfe SW, Pederson WC, Kozin SH, Cohen MS. Green’s operative hand surgery. 8th ed. Philadelphia: Elsevier;2021.2. Chang J, Neligan PC. Plastic surgery. Volume 6. Hand and upper limb. 4th ed. London: Elsevier;2017.3. Riddle RD, Johnson RL, Laufer E, Tabin C. Sonic hedgehog mediates the polarizing activity of the ZPA. Cell. 1993; 75:1401–16.
Article4. Bamshad M, Watkins WS, Dixon ME, et al. Reconstructing the history of human limb development: lessons from birth defects. Pediatr Res. 1999; 45:291–9.
Article5. Korean Society of Plastic and Reconstructive Surgeons. Standard plastic and reconstructive surgery. 3rd ed. Paju: Koonja Publishing;2019.6. Oberg KC, Greer LF, Naruse T. Embryology of the upper limb: the molecular orchestration of morphogenesis. Handchir Mikrochir Plast Chir. 2004; 36:98–107.
Article7. Niswander L, Jeffrey S, Martin GR, Tickle C. A positive feedback loop coordinates growth and patterning in the vertebrate limb. Nature. 1994; 371:609–12.
Article8. Laufer E, Nelson CE, Johnson RL, Morgan BA, Tabin C. Sonic hedgehog and Fgf-4 act through a signaling cascade and feedback loop to integrate growth and patterning of the developing limb bud. Cell. 1994; 79:993–1003.
Article9. Sun X, Lewandoski M, Meyers EN, Liu YH, Maxson RE, Martin GR. Conditional inactivation of Fgf4 reveals complexity of signalling during limb bud development. Nat Genet. 2000; 25:83–6.
Article10. Riddle RD, Ensini M, Nelson C, Tsuchida T, Jessell TM, Tabin C. Induction of the LIM homeobox gene Lmx1 by WNT7a establishes dorsoventral pattern in the vertebrate limb. Cell. 1995; 83:631–40.
Article11. Vogel A, Rodriguez C, Warnken W, Izpisúa Belmonte JC. Dorsal cell fate specified by chick Lmx1 during vertebrate limb development. Nature. 1995; 378:716–20.
Article12. Woods CG, Stricker S, Seemann P, et al. Mutations in WNT7A cause a range of limb malformations, including Fuhrmann syndrome and Al-Awadi/Raas-Rothschild/Schinzel phocomelia syndrome. Am J Hum Genet. 2006; 79:402–8.
Article13. Yang Y, Niswander L. Interaction between the signaling molecules WNT7a and SHH during vertebrate limb development: dorsal signals regulate anteroposterior patterning. Cell. 1995; 80:939–47.
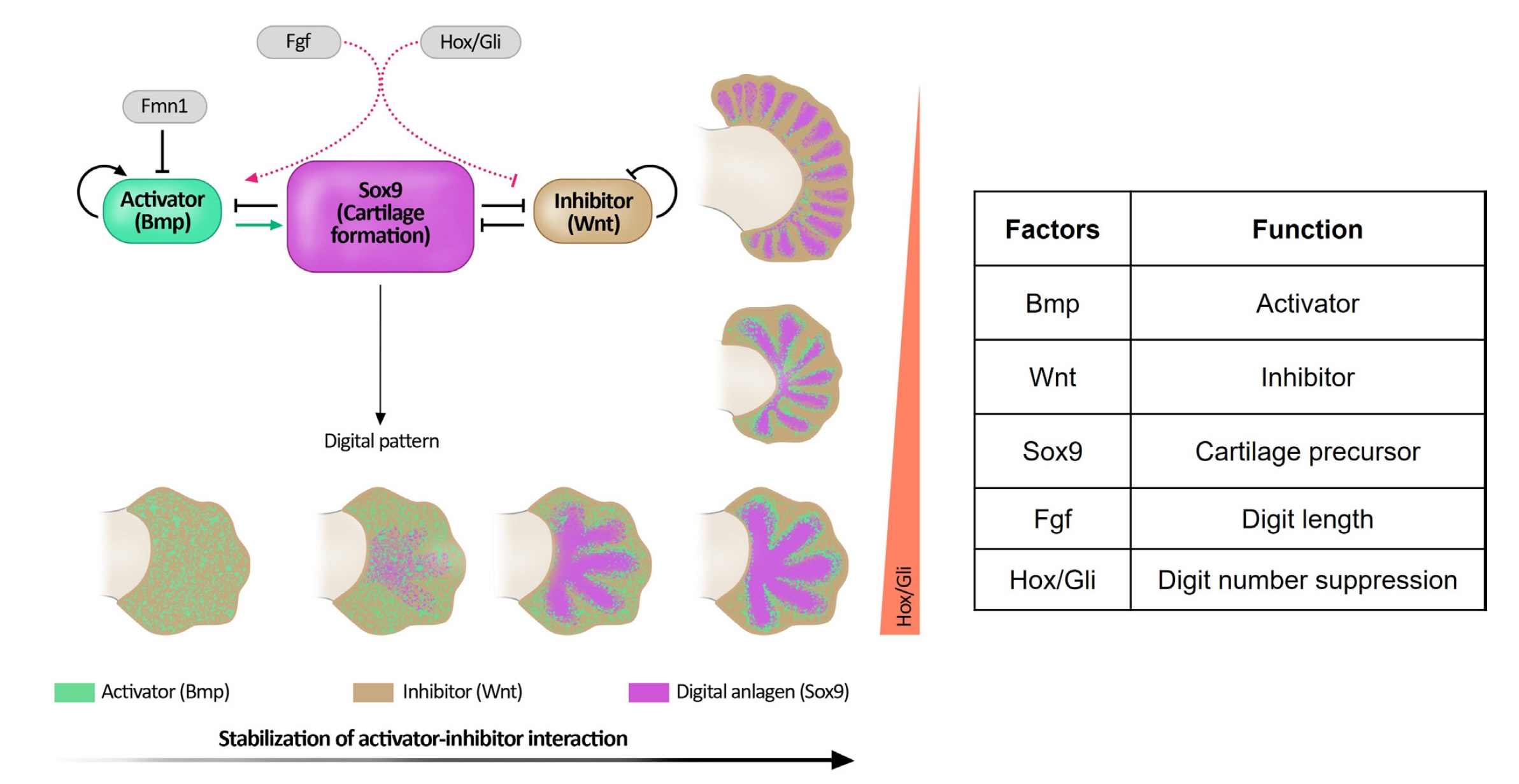
Article14. Raspopovic J, Marcon L, Russo L, Sharpe J. Modeling digits. Digit patterning is controlled by a Bmp-Sox9-Wnt Turing network modulated by morphogen gradients. Science. 2014; 345:566–70.
Article15. Sheth R, Marcon L, Bastida MF, et al. Hox genes regulate digit patterning by controlling the wavelength of a Turing-type mechanism. Science. 2012; 338:1476–80.
Article16. Oberg KC, Ros MA, Goldfarb CA. New insights on upper limb development: digitizing the hand. IFSSH Ezine. 2014; 4:16–22.17. Swanson AB, Barsky AJ, Entin MA. Classification of limb malformations on the basis of embryological failures. Surg Clin North Am. 1968; 48:1169–79.
Article18. Oberg KC, Feenstra JM, Manske PR, Tonkin MA. Developmental biology and classification of congenital anomalies of the hand and upper extremity. J Hand Surg Am. 2010; 35:2066–76.
Article19. Finley WH, Gustavson KH, Hall TM, Hurst DC, Barganier CM, Wiedmeyer JA. Birth defects surveillance: Jefferson County, Alabama, and Uppsala County, Sweden. South Med J. 1994; 87:440–5.
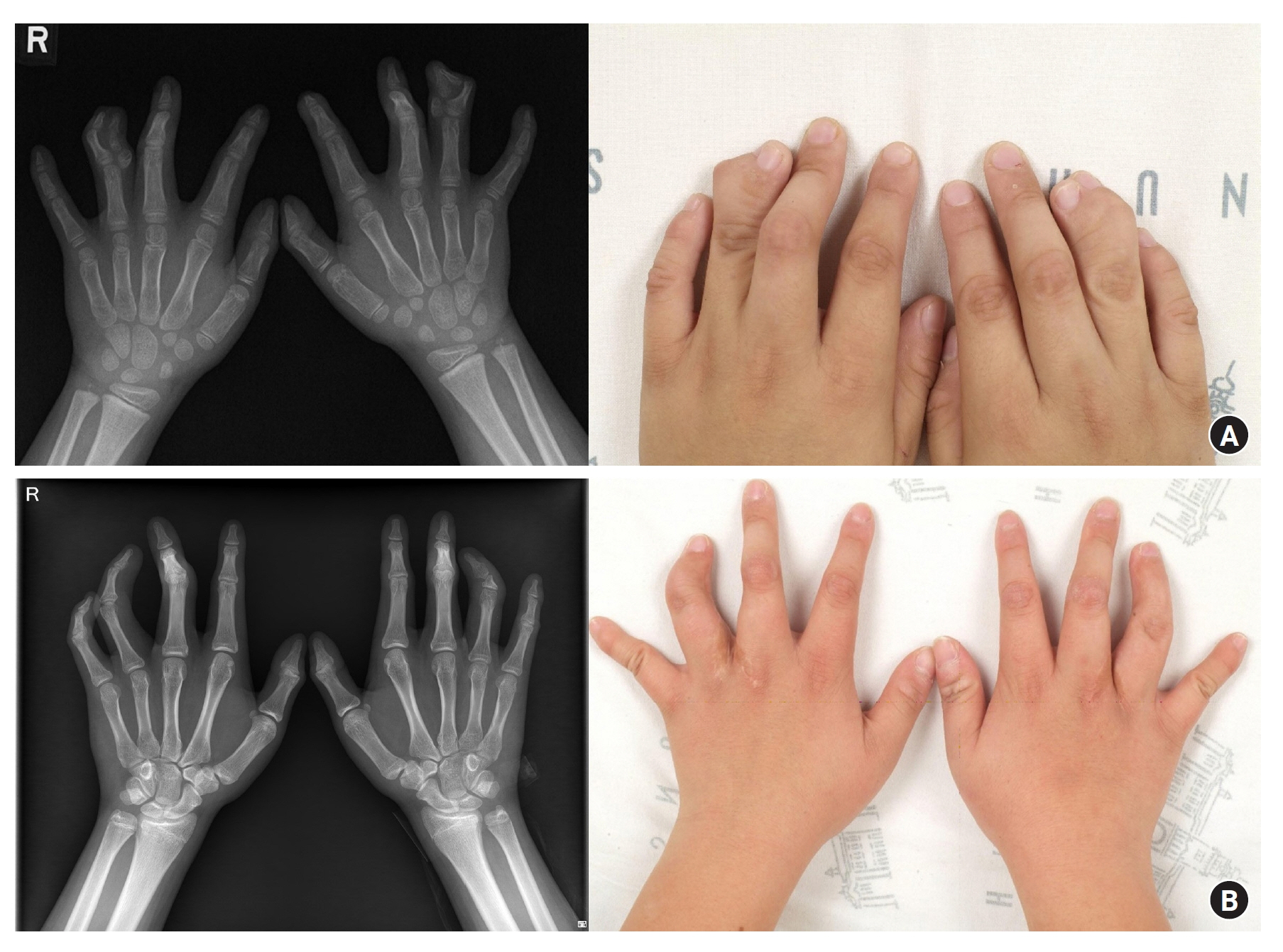
Article20. Kim D, Park SK, Kim DC, Oh SJ, Yoo KY. Nationwide estimation for incidence at birth of congenital polydactyly and syndactyly in Korean. J Korean Soc Plast Reconstr Surg. 2003; 30:24–32.21. Flatt AE. A test of a classification of congenital anomalies of the upper extremity. Surg Clin North Am. 1970; 50:509–16.
Article22. Wassel HD. The results of surgery for polydactyly of the thumb. A review. Clin Orthop Relat Res. 1969; 64:175–93.23. Temtamy SA, McKusick VA. The genetics of hand malformations. Birth Defects Orig Artic Ser. 1978; 14:i–xviii, 1-619.24. Wood VE. Treatment of central polydactyly. Clin Orthop Relat Res. 1971; 74:196–205.
Article25. Tada K, Kurisaki E, Yonenobu K, Tsuyuguchi Y, Kawai H. Central polydactyly: a review of 12 cases and their surgical treatment. J Hand Surg Am. 1982; 7:460–5.26. Comer GC, Potter M, Ladd AL. Polydactyly of the hand. J Am Acad Orthop Surg. 2018; 26:75–82.
Article27. McCarroll HR. Congenital anomalies: a 25-year overview. J Hand Surg Am. 2000; 25:1007–37.
Article28. Kim BJ, Choi JH, Kwon ST. Oblique osteotomy for the correction of the zigzag deformity of Wassel type IV polydactyly. Plast Reconstr Surg. 2017; 140:1220–8.
Article29. Bilhaut M. The curing of a bifid thumb by a new operative procedure (translated from the original French by HE Tonkin and MA Tonkin). Hand Surg. 1997; 2:75–7.
Article30. Townsend DJ, Lipp EB, Chun K, Reinker K, Tuch B. Thumb duplication, 66 years’ experience: a review of surgical complications. J Hand Surg Am. 1994; 19:973–6.31. Kim BJ, Choi JH, Kwon ST. Surgical treatment of axial polysyndactyly and postaxial polydactyly of the hand in Korean: a clinical analysis of 24 cases. J Korean Soc Surg Hand. 2017; 22:20–6.
Article32. Watson BT, Hennrikus WL. Postaxial type-B polydactyly. Prevalence and treatment. J Bone Joint Surg Am. 1997; 79:65–8.33. Singer G, Thein S, Kraus T, Petnehazy T, Eberl R, Schmidt B. Ulnar polydactyly: an analysis of appearance and postoperative outcome. J Pediatr Surg. 2014; 49:474–6.34. Mullick S, Borschel GH. A selective approach to treatment of ulnar polydactyly: preventing painful neuroma and incomplete excision. Pediatr Dermatol. 2010; 27:39–42.
Article35. Stutz C, Mills J, Wheeler L, Ezaki M, Oishi S. Long-term outcomes following radial polydactyly reconstruction. J Hand Surg Am. 2014; 39:1549–52.
Article36. Jordan D, Hindocha S, Dhital M, Saleh M, Khan W. The epidemiology, genetics and future management of syndactyly. Open Orthop J. 2012; 6:14–27.
Article37. Mantero R, Ferrari GL, Ghigliazza GB, Auxilia E. [Syndactyly: an angiographic study]. Ann Chir Main. 1983; 2:62–5. French.38. Samson P, Salazard B. [Syndactyly]. Chir Main. 2008; 27 Suppl 1:S100–14. French.39. Tonkin MA. Classification of congenital anomalies of the hand and upper limb. J Hand Surg Eur Vol. 2017; 42:448–56.
Article40. Le Hanneur M, Cambon-Binder A, Bachy M, Fitoussi F. Treatment of congenital syndactyly. Hand Surg Rehabil. 2020; 39:143–53.
Article41. Kozin SH, Zlotolow DA. Common pediatric congenital conditions of the hand. Plast Reconstr Surg. 2015; 136:241e–57e.
Article42. Hynes SL, Harvey I, Thomas K, Copeland J, Borschel GH. CT angiography-guided single-stage release of adjacent webspaces in non-Apert syndactyly. J Hand Surg Eur Vol. 2015; 40:625–32.
Article43. Tian X, Xiao J, Li T, Chen W, Lin Q, Chim H. Single-stage separation of 3- and 4-finger incomplete simple syndactyly with contiguous gull wing flaps: a technique to minimize or avoid skin grafting. J Hand Surg Am. 2017; 42:257–64.
Article44. Flatt AE. Treatment of syndactylism. Plast Reconstr Surg Transplant Bull. 1962; 29:336–41.
Article45. Toledo LC, Ger E. Evaluation of the operative treatment of syndactyly. J Hand Surg Am. 1979; 4:556–64.
Article46. Keret D, Ger E. Evaluation of a uniform operative technique to treat syndactyly. J Hand Surg Am. 1987; 12(5 Pt 1):727–9.
Article47. Barabás AG, Pickford MA. Results of syndactyly release using a modification of the Flatt technique. J Hand Surg Eur Vol. 2014; 39:984–8.
Article48. De Smet L, Van Ransbeeck H, Deneef G. Syndactyly release: results of the Flatt technique. Acta Orthop Belg. 1998; 64:301–5.49. D’Arcangelo M, Gilbert A, Pirrello R. Correction of syndactyly using a dorsal omega flap and two lateral and volar flaps. A long-term review. J Hand Surg Br. 1996; 21:320–4.50. Uzunismail A. Utility of the “seagull” flap for unoperated simple complete syndactyly in adults. Br J Plast Surg. 1988; 41:548–50.
Article51. Delord M, Forli A, Aribert M, Moutet F, Corcella D. [Results of Blauth Palmar flap in congenital syndactyly: long-term outcome in a 31 webs study]. Ann Chir Plast Esthet. 2020; 65:204–12. French.52. Killian JT, Neimkin RJ. Syndactyly reconstruction by a modified Cronin method. South Med J. 1985; 78:414–8.
Article53. Lewis RC, Nordyke MD, Duncan KH. Web space reconstruction with a M-V flap. J Hand Surg Am. 1988; 13:40–3.
Article54. Karacaoglan N, Velidedeoglu H, Ciçekçi B, Bozdogan N, Sahin U, Türkgüven Y. Reverse W-M plasty in the repair of congenital syndactyly: a new method. Br J Plast Surg. 1993; 46:300–2.
Article55. Savaci N, Hoŝnuter M, Tosun Z. Use of reverse triangular V-Y flaps to create a web space in syndactyly. Ann Plast Surg. 1999; 42:540–4.
Article56. Mericli AF, Black JS, Morgan RF. Syndactyly web space reconstruction using the tapered M-to-V flap: a single-surgeon, 30-year experience. J Hand Surg Am. 2015; 40:1755–63.
Article57. Karamese M, Akdag O, Selimoglu MN, Unal Yıldıran G, Tosun Z. V-Y and rectangular flap combination for syndactyly repair. J Plast Surg Hand Surg. 2016; 50:102–6.
Article58. Bulic K. Long-term aesthetic outcome of fingertip reconstruction in complete syndactyly release. J Hand Surg Eur Vol. 2013; 38:281–7.
Article59. Golash A, Watson JS. Nail fold creation in complete syndactyly using Buck-Gramcko pulp flaps. J Hand Surg Br. 2000; 25:11–4.
Article60. Buck-Gramcko D. Congenital malformations of the hand and forearm. London: Churchill Livingstone;1998.
Article61. Duteille F, Truffandier MV, Perrot P. ‘Matriderm’ dermal substitute with split-thickness skin graft compared with full-thickness skin graft for the coverage of skin defects after surgical treatment of congenital syndactyly: results in 40 commissures. J Hand Surg Eur Vol. 2016; 41:350–1.
Article62. Deunk J, Nicolai JP, Hamburg SM. Long-term results of syndactyly correction: full-thickness versus split-thickness skin grafts. J Hand Surg Br. 2003; 28:125–30.
Article63. Landi A, Garagnani L, Leti Acciaro A, Lando M, Ozben H, Gagliano MC. Hyaluronic acid scaffold for skin defects in congenital syndactyly release surgery: a novel technique based on the regenerative model. J Hand Surg Eur Vol. 2014; 39:994–1000.
Article64. Wang S, Zheng S, Li N, Feng Z, Liu Q. Dorsal hexagon local flap without skin graft for web reconstruction of congenital syndactyly. J Hand Surg Am. 2020; 45:63.
Article65. Widerberg A, Sommerstein K, Dahlin LB, Rosberg HE. Long-term results of syndactyly correction by the trilobed flap technique focusing on hand function and quality of life. J Hand Surg Eur Vol. 2016; 41:315–21.
Article66. Ni F, Mao H, Yang X, Zhou S, Jiang Y, Wang B. The use of an hourglass dorsal advancement flap without skin graft for congenital syndactyly. J Hand Surg Am. 2015; 40:1748–54.
Article67. Dong Y, Wang Y. The use of a dorsal double-wing flap without skin grafts for congenital syndactyly treatment: a STROBE compliant study. Medicine (Baltimore). 2017; 96:e7639.68. Yuan F, Zhong L, Chung KC. Aesthetic comparison of two different types of web-space reconstruction for finger syndactyly. Plast Reconstr Surg. 2018; 142:963–71.
Article69. Ferrari BR, Werker PM. A cross-sectional study of long-term satisfaction after surgery for congenital syndactyly: does skin grafting influence satisfaction? J Hand Surg Eur Vol. 2019; 44:296–303.
Article70. Wang AA, Hutchinson DT. Syndactyly release: a comparison of skin graft versus graftless techniques in the same patient. J Hand Surg Eur Vol. 2019; 44:845–9.
Article71. Zucker RM, Cleland HJ, Haswell T. Syndactyly correction of the hand in Apert syndrome. Clin Plast Surg. 1991; 18:357–64.
Article72. Chang J, Danton TK, Ladd AL, Hentz VR. Reconstruction of the hand in Apert syndrome: a simplified approach. Plast Reconstr Surg. 2002; 109:465–71.
Article73. Fearon JA. Treatment of the hands and feet in Apert syndrome: an evolution in management. Plast Reconstr Surg. 2003; 112:1–12.
Article74. Guero SJ. Algorithm for treatment of Apert hand. Tech Hand Up Extrem Surg. 2005; 9:126–33.
Article75. Taghinia AH, Yorlets RR, Doyle M, Labow BI, Upton J. Long-term functional upper-extremity outcomes in adults with Apert syndrome. Plast Reconstr Surg. 2019; 143:1136–45.
Article76. Flatt AE. The care of congenital hand anomalies. St. Louis: Quality Medical;1994.77. Rios JJ, Paria N, Burns DK, et al. Somatic gain-of-function mutations in PIK3CA in patients with macrodactyly. Hum Mol Genet. 2013; 22:444–51.
Article78. Ezaki M, Beckwith T, Oishi SN. Macrodactyly: decision-making and surgery timing. J Hand Surg Eur Vol. 2019; 44:32–42.
Article79. Tsuge K, Ikuta Y. Macrodactyly and fibro-fatty proliferation of the median nerve. Hiroshima J Med Sci. 1973; 22:83–101.80. Barsky AJ. Macrodactyly. J Bone Joint Surg Am. 1967; 49:1255–66.
Article81. Tsuge K. Treatment of macrodactyly. J Hand Surg Am. 1985; 10(6 Pt 2):968–9.
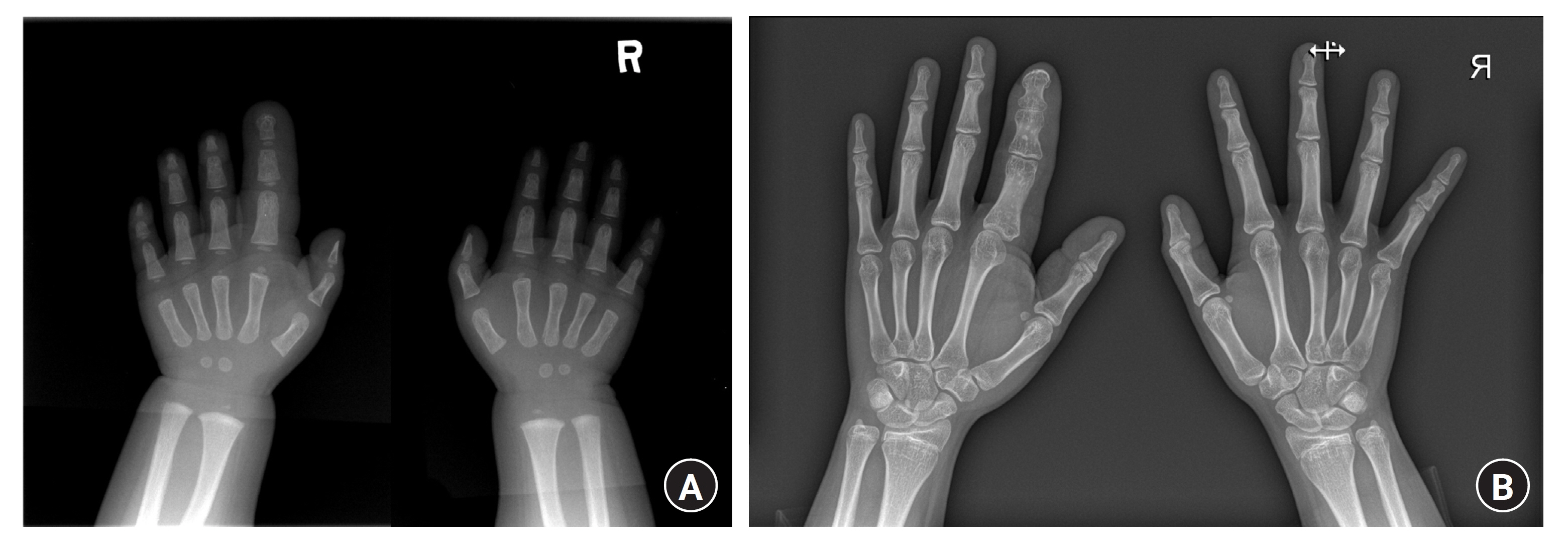
Article82. Cerrato F, Eberlin KR, Waters P, Upton J, Taghinia A, Labow BI. Presentation and treatment of macrodactyly in children. J Hand Surg Am. 2013; 38:2112–23.83. Woo SJ, Jung JH, Choi JH, Kim Y, Kwon ST, Kim BJ. The effect of epiphysiodesis on the longitudinal bone growth of hands or feet in children with macrodactyly based on long-term quantitative analysis. J Pediatr Orthop. 2023; 43:e363–9.
Article84. Shen XF, Gasteratos K, Spyropoulou GA, Yin F, Rui YJ. Congenital difference of the hand and foot: pediatric macrodactyly. J Plast Reconstr Aesthet Surg. 2022; 75:4054–62.
Article85. Stern PJ, Nyquist SR. Macrodactyly in ulnar nerve distribution associated with cubital tunnel syndrome. J Hand Surg Am. 1982; 7:569–71.
Article86. Al-Qattan MM. Lipofibromatous hamartoma of the median nerve and its associated conditions. J Hand Surg Br. 2001; 26:368–72.
Article87. Waters PM, Bae DS. Pediatric hand and upper limb surgery: a practical guide. Philadelpia: Wolters Kluwer Health/Lippincott Williams & Wilkins;2012.88. Wu J, Tian G, Ji Y, Higgins JP, Lee WP. Clinical characteristics of 90 macrodactyly cases. J Hand Surg Am. 2020; 45:982.89. Kalb JP, Suarez DA, Herrera AM. Bilateral macrodactyly of the halluces in an adolescent girl corrected with shortening osteotomies of the first metatarsal and the phalangeal bones: a case report. JBJS Case Connect. 2018; 8:e58.90. Temtamy SA, Rogers JG. Macrodactyly, hemihypertrophy, and connective tissue nevi: report of a new syndrome and review of the literature. J Pediatr. 1976; 89:924–7.
Article91. Wiedemann HR, Burgio GR, Aldenhoff P, Kunze J, Kaufmann HJ, Schirg E. The Proteus syndrome. Partial gigantism of the hands and/or feet, nevi, hemihypertrophy, subcutaneous tumors, macrocephaly or other skull anomalies and possible accelerated growth and visceral affections. Eur J Pediatr. 1983; 140:5–12.92. Ishida O, Ikuta Y. Long-term results of surgical treatment for macrodactyly of the hand. Plast Reconstr Surg. 1998; 102:1586–90.
Article93. Topoleski TA, Ganel A, Grogan DP. Effect of proximal phalangeal epiphysiodesis in the treatment of macrodactyly. Foot Ankle Int. 1997; 18:500–3.
Article94. Badawy M, Ma Y, Baldrighi C, Oestreich K, Jester A. Efficacy of mTOR inhibitors (sirolimus) in isolated limb overgrowth: a systematic review. J Hand Surg Eur Vol. 2022; 47:698–704.
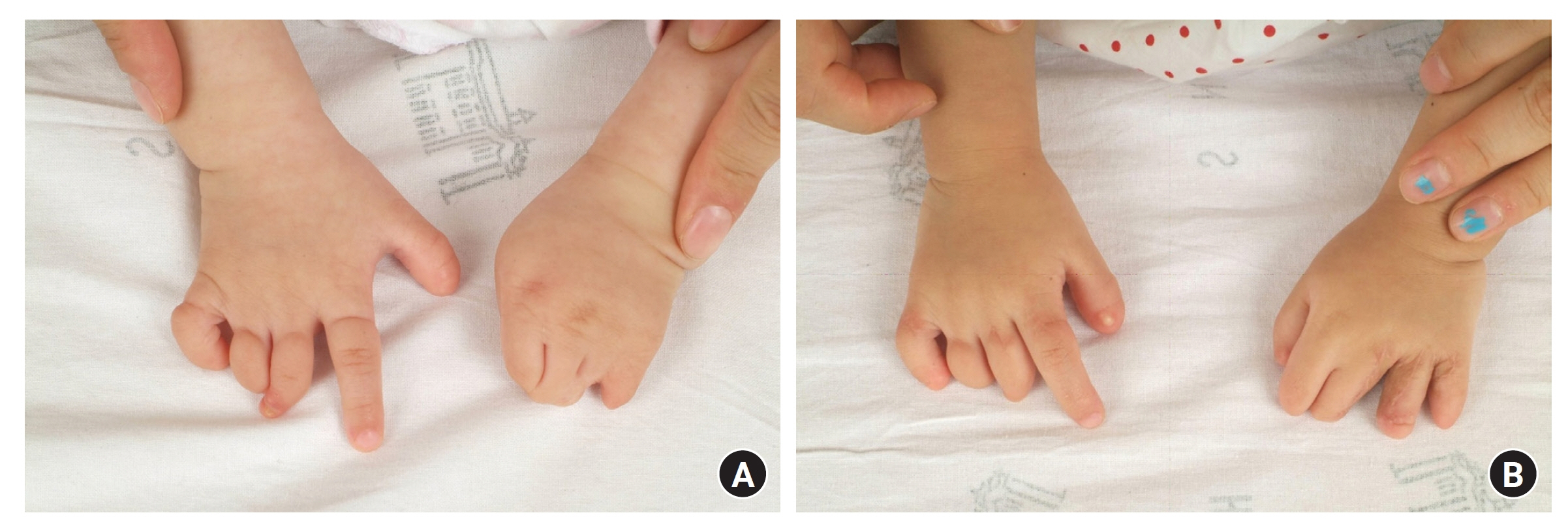
Article95. Inglesby DC, Janssen PL, Graziano FD, Gopman JM, Rutland JW, Taub PJ. Amniotic band syndrome: head-to-toe manifestations and clinical management guidelines. Plast Reconstr Surg. 2023; 152:338e–46e.
Article96. Chiu DT, Patel A, Sakamoto S, Chu A. The impact of microsurgery on congenital hand anomalies associated with amniotic band syndrome. Plast Reconstr Surg Glob Open. 2018; 6:e1657.
Article97. Cignini P, Giorlandino C, Padula F, Dugo N, Cafà EV, Spata A. Epidemiology and risk factors of amniotic band syndrome, or ADAM sequence. J Prenat Med. 2012; 6:59–63.98. Jiang Y, Mao H, Yang X, et al. Single-stage resection of type II constriction rings in limbs on the basis of histologic and magnetic resonance imaging observations: a retrospective study of 21 consecutive patients. Plast Reconstr Surg. 2016; 138:164–73.
Article99. Mukherjee PM, Natera M, Drew H, Creanga A. Amniotic band syndrome: a multidisciplinary care approach to the treatment of a rare case. Cleft Palate Craniofac J. 2019; 56:105–9.
Article100. Torpin R. Amniochorionic mesoblastic fibrous strings and amnionic bands: associated constricting fetal malformations or fetal death. Am J Obstet Gynecol. 1965; 91:65–75.101. Van Allen MI, Siegel-Bartelt J, Dixon J, Zuker RM, Clarke HM, Toi A. Constriction bands and limb reduction defects in two newborns with fetal ultrasound evidence for vascular disruption. Am J Med Genet. 1992; 44:598–604.
Article102. Syvänen J, Raitio A, Nietosvaara Y, et al. Risk factors and prevalence of limb deficiencies associated with amniotic band sequence: a population-based case-control study. J Pediatr Orthop. 2021; 41:e94–7.
Article103. Patterson TJ. Congenital ring-constrictions. Br J Plast Surg. 1961; 14:1–31.
Article104. Weinzweig N, Barr A. Radial, ulnar, and median nerve palsies caused by a congenital constriction band of the arm: single-stage correction. Plast Reconstr Surg. 1994; 94:872–6.105. Dufournier B, Guero S, de Tienda M, et al. One-stage circumferential limb ring constriction release and direct circular skin closure in amniotic band syndrome: a 14-case series. Orthop Traumatol Surg Res. 2020; 106:1353–9.
Article106. Habenicht R, Hülsemann W, Lohmeyer JA, Mann M. Ten-year experience with one-step correction of constriction rings by complete circular resection and linear circumferential skin closure. J Plast Reconstr Aesthet Surg. 2013; 66:1117–22.107. Mutaf M, Sunay M. A new technique for correction of congenital constriction rings. Ann Plast Surg. 2006; 57:646–52.
Article108. Castro-Govea Y, Vela-Martinez A, Treviño-Garcia LA. Lipoinjection and multiple internal cuts for congenital constriction bands: a new treatment approach. Aesthetic Plast Surg. 2017; 41:375–80.
Article109. Mende K, Suurmeijer JA, Tonkin MA. Surgical techniques for reconstruction of the hypoplastic thumb. J Hand Surg Eur Vol. 2019; 44:15–24.
Article110. Tonkin M. Surgical reconstruction of congenital thumb hypoplasia. Indian J Plast Surg. 2011; 44:253–65.
Article111. Entin MA. Reconstruction of congenital aplasia of phalanges in the hand. Surg Clin North Am. 1968; 48:1155–68.
Article112. Manske PR, McCarroll HR. Reconstruction of the congenitally deficient thumb. Hand Clin. 1992; 8:177–96.
Article113. Blauth W, Schneider-Sickert FR. Congenital deformities of the hand: an atlas of their surgical treatment. Berlin, Heidelberg: Springer;2012.
Article114. Blair WF, Buckwalter JA. Congenital malposition of flexor pollicis longus: an anatomy note. J Hand Surg Am. 1983; 8:93–4.115. Blair WF, Omer GE. Anomalous insertion of the flexor pollicis longus. J Hand Surg Am. 1981; 6:241–4.
Article116. Graham TJ, Louis DS. A comprehensive approach to surgical management of the type IIIA hypoplastic thumb. J Hand Surg Am. 1998; 23:3–13.
Article117. Dellon AL, Rayan G. Congenital absence of the thenar muscles. Report of two cases. J Bone Joint Surg Am. 1981; 63:1014–5.
Article118. Fitch RD, Urbaniak JR, Ruderman RJ. Conjoined flexor and extensor pollicis longus tendons in the hypoplastic thumb. J Hand Surg Am. 1984; 9:417–9.
Article119. Köster G. Isolated aplasia of the flexor pollicis longus: a case report. J Hand Surg Am. 1984; 9:870–1.
Article120. Tsuchida Y, Kasai S, Kojima T. Congenital absence of flexor pollicis longus and flexor pollicis brevis: a case report. Hand. 1976; 8:294–7.
Article121. Arminio JA. Congenital anomaly of the thumb: absent flexor pollicis longus tendon. J Hand Surg Am. 1979; 4:487–8.
Article122. Tupper JW. Pollex abductus due to congenital malposition of the flexor pollicis longus. J Bone Joint Surg Am. 1969; 51:1285–90.
Article123. Lister G. Pollex abductus in hypoplasia and duplication of the thumb. J Hand Surg Am. 1991; 16:626–33.
Article124. Neviaser RJ. Congenital hypoplasia of the thumb with absence of the extrinsic extensors, abductor pollicis longus, and thenar muscles. J Hand Surg Am. 1979; 4:301–3.
Article125. Kobayashi A, Ohmiya K, Iwakuma T, Mitsuyasu M. Unusual congenital anomalies of the thumb extensors. Report of two cases. Hand. 1976; 8:17–21.
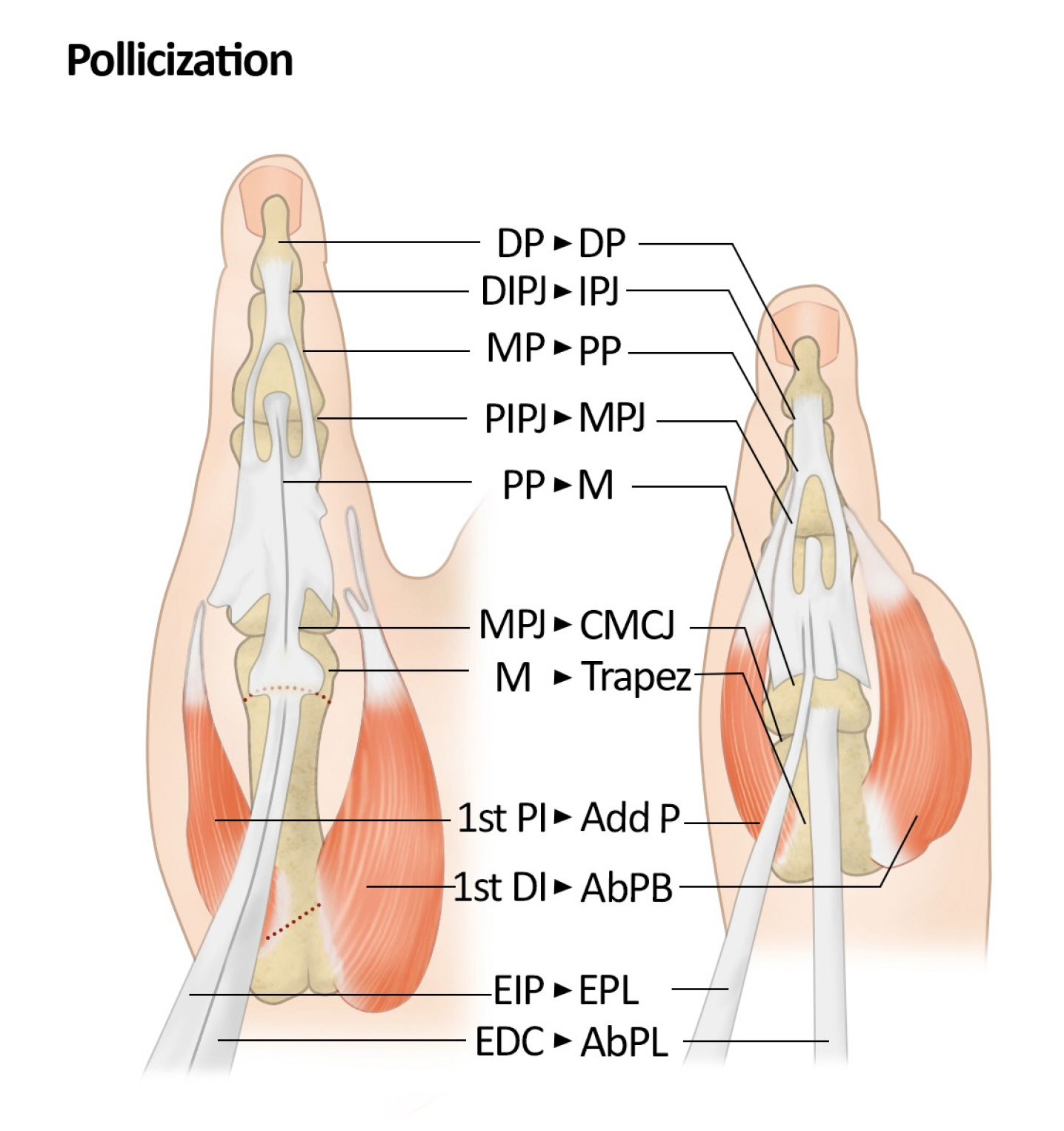
Article126. Upton J. Treatment of congenital forearm and hand anomalies. In : McCarthy JG, May JW, Littler JW, editors. Pleasetic surgery. Philadelphia: WB Saunders;1990. p. 5352–6.127. Taghinia AH, Littler JW, Upton J. Refinements in pollicization: a 30-year experience. Plast Reconstr Surg. 2012; 130:423e–33e.128. Manske PR, Rotman MB, Dailey LA. Long-term functional results after pollicization for the congenitally deficient thumb. J Hand Surg Am. 1992; 17:1064–72.
Article129. Upton J, Havlik RJ, Coombs CJ. Use of forearm flaps for the severely contracted first web space in children with congenital malformations. J Hand Surg Am. 1996; 21:470–7.
Article130. Coombs CJ, Mutimer KL. Tissue expansion for the treatment of complete syndactyly of the first web. J Hand Surg Am. 1994; 19:968–72.
Article131. Smith P, Sivakumar B, Hall R, Fleming A. Blauth II thumb hypoplasia: a management algorithm for the unstable metacarpophalangeal joint. J Hand Surg Eur Vol. 2012; 37:745–50.
Article132. Hovius SE, Versnel SL, Zuidam JM. Tendon transfers in the congenital hand. In : Friden J, editor. Tendon transfers in reconstructive hand surgery. London: CRC Press;2005. p. 121–32.133. de Kraker M, Selles RW, Zuidam JM, Molenaar HM, Stam HJ, Hovius SE. Outcome of flexor digitorum superficialis opponensplasty for Type II and IIIA thumb hypoplasia. J Hand Surg Eur Vol. 2016; 41:258–64.
Article134. Vuillermin C, Butler L, Lake A, Ezaki M, Oishi S. Flexor digitorum superficialis opposition transfer for augmenting function in types II and IIIA thumb hypoplasia. J Hand Surg Am. 2016; 41:244–9.
Article135. Manske PR, McCarroll HR. Abductor digiti minimi opponensplasty in congenital radial dysplasia. J Hand Surg Am. 1978; 3:552–9.
Article136. Ogino T, Minami A, Fukuda K. Abductor digiti minimi opponensplasty in hypoplastic thumb. J Hand Surg Br. 1986; 11:372–7.
Article137. Upton J, Taghinia AH. Abductor digiti minimi myocutaneous flap for opponensplasty in congenital hypoplastic thumbs. Plast Reconstr Surg. 2008; 122:1807–11.
Article138. Light TR, Gaffey JL. Reconstruction of the hypoplastic thumb. J Hand Surg Am. 2010; 35:474–9.
Article139. Christen T, Dautel G. Type II and IIIA thumb hypoplasia reconstruction. J Hand Surg Am. 2013; 38:2009–15.
Article140. Abdel-Ghani H, Amro S. Characteristics of patients with hypoplastic thumb: a prospective study of 51 patients with the results of surgical treatment. J Pediatr Orthop B. 2004; 13:127–38.
Article141. Buck-Gramcko D. Pollicization of the index finger. Method and results in aplasia and hypoplasia of the thumb. J Bone Joint Surg Am. 1971; 53:1605–17.142. Foucher G, Medina J, Lorea P, Pivato G. Principalization of pollicization of the index finger in congenital absence of the thumb. Tech Hand Up Extrem Surg. 2005; 9:96–104.
Article143. Kozin SH, Weiss AA, Webber JB, Betz RR, Clancy M, Steel HH. Index finger pollicization for congenital aplasia or hypoplasia of the thumb. J Hand Surg Am. 1992; 17:880–4.
Article144. Ozols D, Butnere MM, Petersons A. Methods for congenital thumb hypoplasia reconstruction. A review of the outcomes for ten years of surgical treatment. Medicina (Kaunas). 2019; 55:610.
Article145. Schneider W, Reichert B, Pallua N, Meyer H. Correction of hypoplastic thumb by free transfer of metatarsal bone: a case report. Microsurgery. 1993; 14:468–71.
Article146. Chow CS, Ho PC, Tse WL, Hung LK. Reconstruction of hypoplastic thumb using hemi-longitudinal metatarsal transfer. J Hand Surg Eur Vol. 2012; 37:738–44.
Article147. Zhong W, Tian W, Zhao J, et al. Nonvascularized iliac crest bone graft for reconstruction of the first metacarpal in type IIIB thumb hypoplasia: a radiographic follow-up study. J Hand Surg Am. 2023; 48:196.
Article148. O'Brien BM, Black MJ, Morrison WA, MacLeod AM. Microvascular great toe transfer for congenital absence of the thumb. Hand. 1978; 10:113–24.149. Ozols D, Zarins J, Petersons A. Novel technique for toe-to-hand transplantation: the fourth-toe as an alternative option for toe-to-hand transplantation for pediatric patients. Tech Hand Up Extrem Surg. 2019; 23:74–80.
Article150. Foucher G, Medina J, Navarro R. Microsurgical reconstruction of the hypoplastic thumb, type IIIB. J Reconstr Microsurg. 2001; 17:9–15.
Article151. Tu YK, Yeh WL, Sananpanich K, et al. Microsurgical second toe-metatarsal bone transfer for reconstructing congenital radial deficiency with hypoplastic thumb. J Reconstr Microsurg. 2004; 20:215–25.
Article152. Ozols D, Zariņš J, Pētersons A. Long-term evaluation of the functional and esthetical outcomes for the new method of the toe-to-hand transfer for full-length thumb reconstruction in congenital thumb’s hypoplasia in children. Proc Latv Acad Sci Sect B. 2019; 43:171–6.
Article153. Ozols D, Butnere MM, Petersons A. The second toe-to-hand transfer for full-length thumb reconstruction in congenital thumb’s grade IIIb to V hypoplasia: MTPJ arthrodesis instead of tendon rebalansing. Tech Hand Up Extrem Surg. 2020; 24:13–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Congenital Differences of the Upper Extremity: Classification and Treatment Principles
- A Case of Maffucci's Syndrome
- Macrodactylism Associated with Neurofibroma of the Median Nerve: A Case Report
- Congenital Dermatofibrosarcoma Protuberans: A Case Report and Literature Review
- Diagnosing Cervical Fusion: A Comprehensive Literature Review