Ann Rehabil Med.
2024 Feb;48(1):65-74. 10.5535/arm.230012.
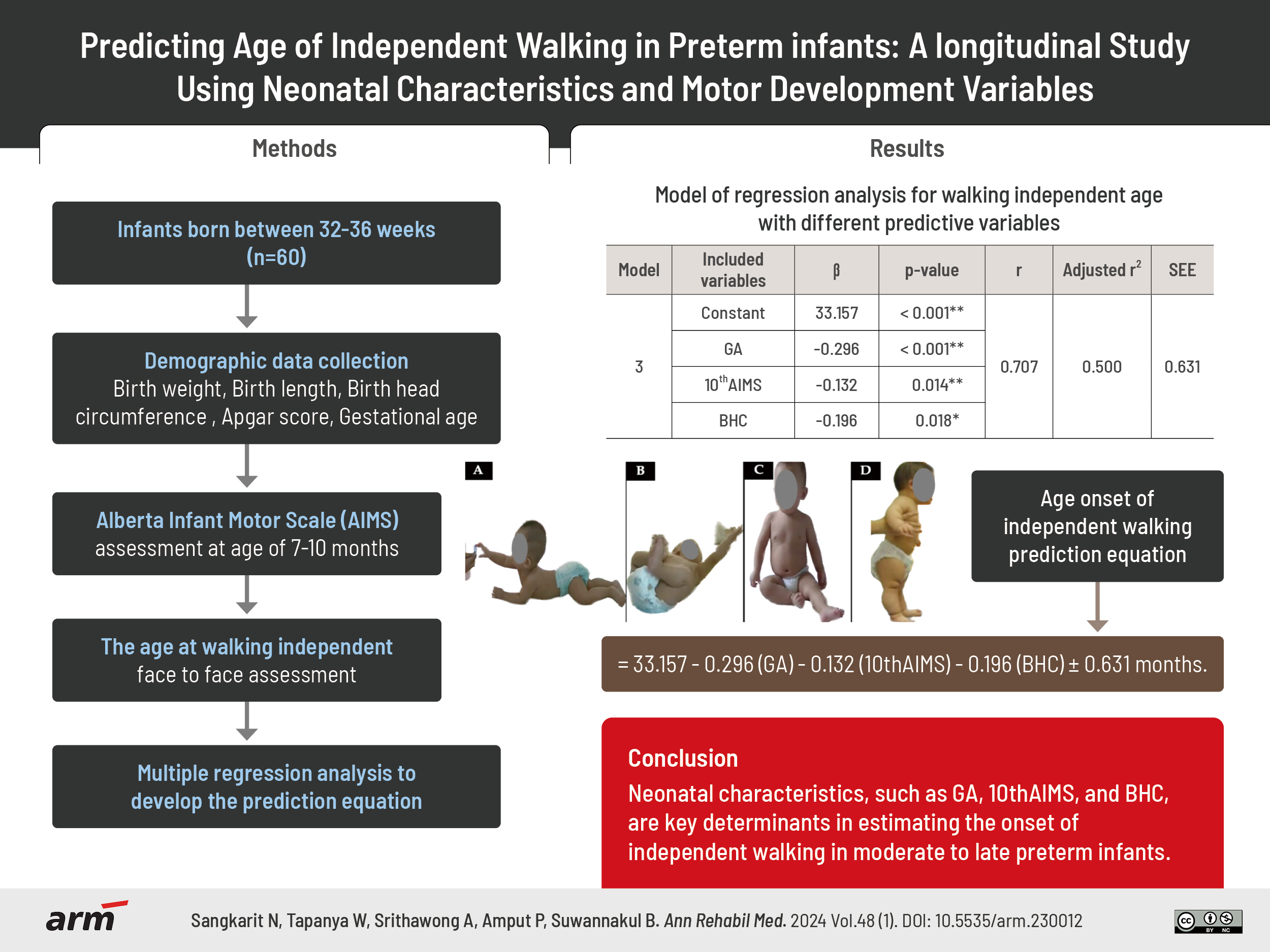
Predicting Age of Independent Walking in Preterm Infants: A Longitudinal Study Using Neonatal Characteristics and Motor Development Variables
- Affiliations
-
- 1Department of Physical Therapy, School of Allied Health Sciences, University of Phayao, Phayao, Thailand
- 2Unit of Excellence of Human Performance and Rehabilitations, University of Phayao, Phayao, Thailand
- KMID: 2553163
- DOI: http://doi.org/10.5535/arm.230012
Abstract
Objective
To formulate an equation estimating months to independent walking in moderate to late preterm infants based on neonatal characteristics and gross motor development from 7 months to independent walking.
Methods
Sixty infants born between 32 to 36 weeks were assessed using Alberta Infant Motor Scale (AIMS) for gross motor development. Neonatal characteristics were recorded at 7 months, and caregiver-reported independent walking onset. Pearson correlation analyzed age, AIMS scores, and neonatal factors. Multiple regression developed the prediction equation.
Results
The equation for independent walking onset, which included gestational age (GA) at birth, total AIMS score at 10 months of age (10th AIMS), and birth head circumference (BHC), exhibited a strong correlation (r=0.707) and had a predictive power of 50.0%. The equation is as follows: age onset of independent walking (months)=33.157, -0.296 (GA), -0.132 (10th AIMS), -0.196 (BHC), with an estimation error of 0.631 months.
Conclusion
Neonatal characteristics, such as GA, 10th AIMS, and BHC, are key determinants in estimating the onset of independent walking in moderate to late preterm infants.
Keyword
Figure
Reference
-
1. Prommin S, Siritaratiwat W, Bennett S, Mato L, Keeratisiroj O, Kamruecha W. Effects of play in an upright position on intra-individual variability of gross motor and language development in institutionalized infants. Int J Environ Res Public Health. 2022; 19:11804.2. WHO Multicentre Growth Reference Study Group. WHO Motor Development Study: windows of achievement for six gross motor development milestones. Acta Paediatr Suppl. 2006; 450:86–95.3. Pin TW, Butler PB, Cheung HM, Shum SL. Longitudinal development of segmental trunk control in full term and preterm infants- a pilot study: part I. Dev Neurorehabil. 2020; 23:185–92.4. Kayenne Martins Roberto Formiga C, Linhares MB. Motor development curve from 0 to 12 months in infants born preterm. Acta Paediatr. 2011; 100:379–84.5. Hadders-Algra M. Early human motor development: from variation to the ability to vary and adapt. Neurosci Biobehav Rev. 2018; 90:411–27.6. Fuentefria RDN, Silveira RC, Procianoy RS. Motor development of preterm infants assessed by the Alberta Infant Motor Scale: systematic review article. J Pediatr (Rio J). 2017; 93:328–42.7. Maia PC, Silva LP, Oliveira MMC, Cardoso MVLML. Motor development of preterm and term infants: using the Alberta Infant Motor Scale. Acta Paul Enferm. 2011; 24:670–5.8. Syrengelas D, Kalampoki V, Kleisiouni P, Manta V, Mellos S, Pons R, et al. Alberta Infant Motor Scale (AIMS) performance of greek preterm infants: comparisons with full-term infants of the same nationality and impact of prematurity-related morbidity factors. Phys Ther. 2016; 96:1102–8.9. Saccani R, Valentini NC, Pereira KR, Müller AB, Gabbard C. Associations of biological factors and affordances in the home with infant motor development. Pediatr Int. 2013; 55:197–203.10. Halpern R, Giugliani ER, Victora CG, Barros FC, Horta BL. [Risk factors for suspicion of developmental delays at 12 months of age]. J Pediatr (Rio J). 2000; 76:421–8. Portuguese.11. Casey BM, McIntire DD, Leveno KJ. The continuing value of the Apgar score for the assessment of newborn infants. N Engl J Med. 2001; 344:467–71.12. Keeratisiroj O, Thawinchai N, Siritaratiwat W, Buntragulpoontawee M, Pratoomsoot C. Prognostic predictors for ambulation in children with cerebral palsy: a systematic review and meta-analysis of observational studies. Disabil Rehabil. 2018; 40:135–43.13. Aimsamrarn P, Janyachareon T, Rattanathanthong K, Emasithi A, Siritaratiwat W. Cultural translation and adaptation of the Alberta Infant Motor Scale Thai version. Early Hum Dev. 2019; 130:65–70.14. Tupsila R, Siritaratiwat W, Bennett S, Mato L, Keeratisiroj O. Intra-individual variability in gross motor development in healthy full-term infants aged 0-13 months and associated factors during child rearing. Children (Basel). 2022; 9:801.15. de Vries LS, Eken P, Dubowitz LM. The spectrum of leukomalacia using cranial ultrasound. Behav Brain Res. 1992; 49:1–6.16. Papile LA, Burstein J, Burstein R, Koffler H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J Pediatr. 1978; 92:529–34.17. Piper MC, Darrah J. Motor assessment of the developing infant. Saunders;1994. p. 1–210.18. Wijnhoven TM, de Onis M, Onyango AW, Wang T, Bjoerneboe GE, Bhandari N, et al. Assessment of gross motor development in the WHO Multicentre Growth Reference Study. Food Nutr Bull. 2004; 25(1 Suppl):S37–45.19. Thelen E. Dynamic systems theory and the complexity of change. Psychoanal Dialog. 2005; 15:255–83.20. Kurtoğlu S, Hatipoğlu N, Mazıcıoğlu MM, Akın MA, Çoban D, Gökoğlu S, et al. Body weight, length and head circumference at birth in a cohort of Turkish newborns. J Clin Res Pediatr Endocrinol. 2012; 4:132–9.21. Jenjarat K, Chamnanvanakij S. New reference for neonatal growth: 10-year data of Phramongkutklao Hospital. J Med Assoc Thai. 2020; 103:1284–91.22. Tupsila R, Bennett S, Mato L, Keeratisiroj O, Siritaratiwat W. Gross motor development of Thai healthy full-term infants aged from birth to 14 months using the Alberta Infant Motor Scale: inter individual variability. Early Hum Dev. 2020; 151:105169.23. Yaari M, Mankuta D, Harel-Gadassi A, Friedlander E, Bar-Oz B, Eventov-Friedman S, et al. Early developmental trajectories of preterm infants. Res Dev Disabil. 2018; 81:12–23.24. McGowan JE, Alderdice FA, Holmes VA, Johnston L. Early childhood development of late-preterm infants: a systematic review. Pediatrics. 2011; 127:1111–24.25. Adolph K, Karasik L, Tamis-LeMonda CS. Moving between cultures: cross-cultural research on motor development. In: Bornstein M, editor. Handbook of cross-cultural developmental science. Taylor and Francis; 2010.26. Bartlett D, Piper MC. Neuromotor development of preterm infants through the first year of life. Phys Occup Ther Pediatr. 1993; 12:37–55.27. Wang TN, Howe TH, Hinojosa J, Hsu YW. Postural control of pre-term infants at 6 and 12 months corrected age. Early Hum Dev. 2010; 86:433–7.28. Costa Wiltgen A, Valentini NC, Beltram Marcelino T, Santos Pinto Guimarães L, Homrich Da Silva C, Rombaldi Bernardi J, et al. Different intrauterine environments and children motor development in the first 6 months of life: a prospective longitudinal cohort. Sci Rep. 2023; 13:10325.29. Gaetan EM, Moura-Ribeiro MV. Developmental study of early posture control in preterm and fullterm infants. Arq Neuropsiquiatr. 2002; 60:954–8.30. Shapiro-Mendoza CK. Infants born late preterm: epidemiology, trends, and morbidity risk. NeoReviews. 2009; 10:e287–94.31. Sangkarit N, Keeratisiroj O, Yonglitthipagon P, Bennett S, Siritaratiwat W. Segmental assessment of trunk control in moderate-to-late preterm infants related to sitting development. Children (Basel). 2021; 8:722.32. Saavedra SL, van Donkelaar P, Woollacott MH. Learning about gravity: segmental assessment of upright control as infants develop independent sitting. J Neurophysiol. 2012; 108:2215–29.33. Pin TW, Butler PB, Cheung HM, Shum SL. Segmental Assessment of Trunk Control in infants from 4 to 9 months of age- a psychometric study. BMC Pediatr. 2018; 18:182.34. Zhou L, Zhong W, Liu L. Investigation and influence analysis of motor development in preterm infants. Am J Transl Res. 2023; 15:273–80.35. Duncan K, Goodworth A, Da Costa CSN, Wininger M, Saavedra S. Parent handling of typical infants varies segmentally across development of postural control. Exp Brain Res. 2018; 236:645–54.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparisons of Clinical Characteristics Affecting Readmission between Late Preterm Infants and Moderate Preterm Infants or Full-Term Infants
- Perinatal Outcome in Small for Gestational Age Versus Appropriate for Gestational Age in Preterm Infants
- Neurodevelopmental outcomes of preterm infants
- The Test of Infant Motor Performance (TIMP) in Preterm and Term Infants
- Neonatal outcomes of very low birthweight infants from spontaneous and indicated preterm delivery