J Korean Neurosurg Soc.
2024 Mar;67(2):237-248. 10.3340/jkns.2023.0100.
Medium and Long-Term Data from a Series of 96 Endoscopic Transsphenoidal Surgeries for Cushing Disease
- Affiliations
-
- 1Neurosurgery Clinic, Basaksehir Cam and Sakura City Hospital, Istanbul, Turkey
- 2University of Health Sciences Pituitary Diseases Practice and Research Center (PDPRC), Istanbul, Turkey
- 3Endocrinology and Metabolism Clinic, Bakirkoy Dr. Sadi Konuk Training & Research Hospital, University of Health Sciences, Istanbul, Turkey
- 4Endocrinology and Metabolism Clinic, Basaksehir Cam and Sakura City Hospital, Istanbul, Turkey
- KMID: 2553130
- DOI: http://doi.org/10.3340/jkns.2023.0100
Abstract
Objective
: Postoperative data on Cushing’s disease (CD) are equivocal in the literature. These discrepancies may be attributed to different series with different criteria for remission and variable follow-up durations. Additional data from experienced centers may address these discrepancies. In this study, we present the results obtained from 96 endoscopic transsphenoidal surgeries (ETSSs) for CD conducted in a well-experienced center.
Methods
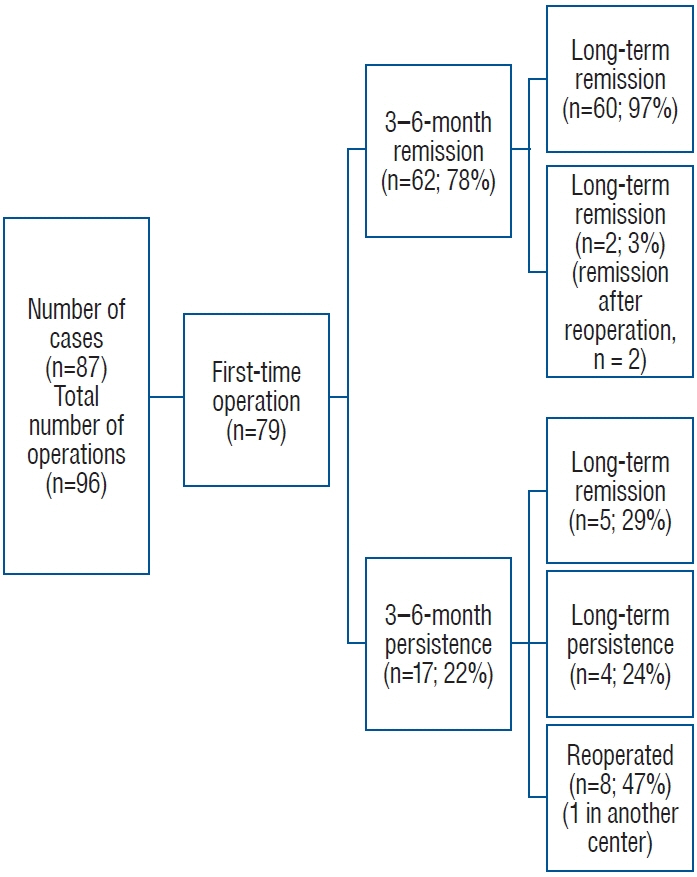
: Pre- and postoperative data of 96 ETSS in 87 patients with CD were included. All cases were handled by the same neurosurgical team between 2014 and 2022. We obtained data on remission status 3−6 months postoperatively (medium-term) and during the latest follow-up (long-term). Additionally, magnetic resonance imaging (MRI) and pathology results were obtained for each case.
Results
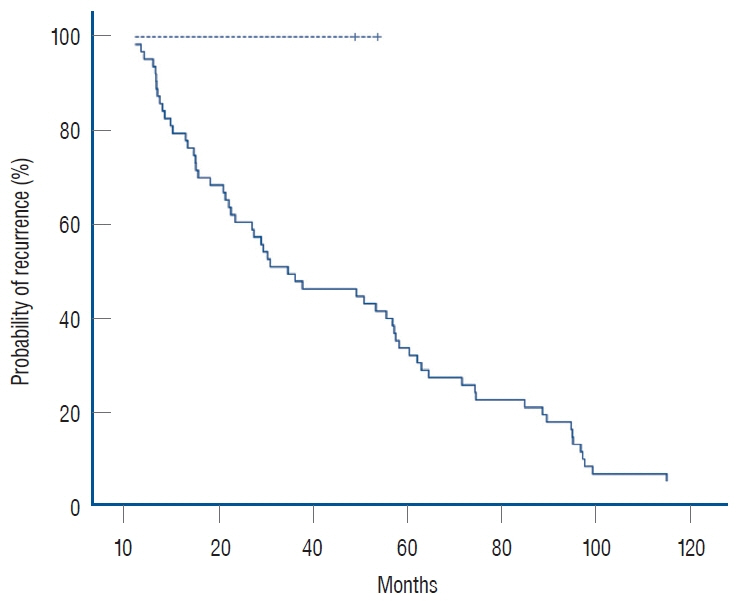
: The mean follow-up duration was 39.5±3.2 months. Medium and long-term remission rates were 77% and 82%, respectively. When only first-time operations were considered, the medium- and long-term remission rates were 78% and 82%, respectively. The recurrence rate in this series was 2.5%. Patients who showed remission between 3−6 months had higher longterm remission rates than did those without initial remission. Tumors >2 cm and extended tumor invasion of the cavernous sinus (Knosp 4) were associated with lower postoperative remission rates.
Conclusion
: Adenoma size and the presence/absence of cavernous sinus invasion on preopera-tive MRI may predict long-term postoperative remission. A tumor size of 2 cm may be a supporting criterion for predicting remission in Knosp 4 tumors. Further studies with larger patient populations are necessary to support this finding.
Figure
Reference
-
References
1. Acebes JJ, Martino J, Masuet C, Montanya E, Soler J. Early post-operative ACTH and cortisol as predictors of remission in Cushing’s disease. Acta Neurochir (Wien). 149:471–477. discussion 477-479. 2007.2. Aranda G, Enseñat J, Mora M, Puig-Domingo M, Martínez de Osaba MJ, Casals G, et al. Long-term remission and recurrence rate in a cohort of Cushing’s disease: the need for long-term follow-up. Pituitary. 18:142–149. 2015.3. Araujo-Castro M, Acitores Cancela A, Vior C, Pascual-Corrales E, Rodríguez Berrocal V. Radiological Knosp, revised-Knosp, and Hardy-Wilson classifications for the prediction of surgical outcomes in the endoscopic endonasal surgery of pituitary adenomas: study of 228 cases. Front Oncol. 11:807040. 2022.4. Biller BM, Grossman AB, Stewart PM, Melmed S, Bertagna X, Bertherat J, et al. Treatment of adrenocorticotropin-dependent Cushing’s syndrome: a consensus statement. J Clin Endocrinol Metab. 93:2454–2462. 2008.5. Brady Z, Garrahy A, Carthy C, O’Reilly MW, Thompson CJ, Sherlock M, et al. Outcomes of endoscopic transsphenoidal surgery for Cushing’s disease. BMC Endocr Disord. 21:36. 2021.6. Brichard C, Costa E, Fomekong E, Maiter D, Raftopoulos C. Outcome of transsphenoidal surgery for cushing disease: a single-center experience over 20 years. World Neurosurg. 119:e106–e117. 2018.7. Broersen LHA, Biermasz NR, van Furth WR, de Vries F, Verstegen MJT, Dekkers OM, et al. Endoscopic vs. microscopic transsphenoidal surgery for Cushing’s disease: a systematic review and meta-analysis. Pituitary. 21:524–534. 2018.8. Cebula H, Baussart B, Villa C, Assié G, Boulin A, Foubert L, et al. Efficacy of endoscopic endonasal transsphenoidal surgery for Cushing’s disease in 230 patients with positive and negative MRI. Acta Neurochir (Wien). 159:1227–1236. 2017.9. Chandler WF, Barkan AL, Hollon T, Sakharova A, Sack J, Brahma B, et al. Outcome of transsphenoidal surgery for cushing disease: a singlecenter experience over 32 years. Neurosurgery. 78:216–223. 2016.10. Ciric I, Zhao JC, Du H, Findling JW, Molitch ME, Weiss RE, et al. Transsphenoidal surgery for Cushing disease: experience with 136 patients. Neurosurgery. 70:70–80. discussion 80-81. 2012.11. Clayton RN, Raskauskiene D, Reulen RC, Jones PW. Mortality and morbidity in Cushing’s disease over 50 years in Stoke-on-Trent, UK: audit and meta-analysis of literature. J Clin Endocrinol Metab. 96:632–642. 2011.12. Dai C, Feng M, Sun B, Bao X, Yao Y, Deng K, et al. Surgical outcome of transsphenoidal surgery in Cushing’s disease: a case series of 1106 patients from a single center over 30 years. Endocrine. 75:219–227. 2022.13. Doglietto F, Maira G. Cushing disease and negative magnetic resonance imaging finding: a diagnostic and therapeutic challenge. World Neurosurg. 77:445–447. 2012.14. Erkan B, Barut O, Akbas A, Akpinar E, Akdeniz YS, Tanriverdi O, et al. Results of endoscopic surgery in patients with pituitary adenomas : association of tumor classification grades with resection, remission, and complication rates. J Korean Neurosurg Soc. 64:608–618. 2021.15. Fang J, Xie S, Li N, Jiang Z. Postoperative complications of endoscopic versus microscopic transsphenoidal pituitary surgery: a meta-analysis. J Coll Physicians Surg Pak. 28:554–559. 2018.16. Feng M, Liu Z, Liu X, Bao X, Yao Y, Deng K, et al. Diagnosis and outcomes of 341 patients with Cushing’s disease following transsphenoid surgery: a single-center experience. World Neurosurg. 109:e75–e80. 2018.17. Fleseriu M, Hamrahian AH, Hoffman AR, Kelly DF, Katznelson L; AACE Neuroendocrine, Pituitary Scientific Committee. American Association of Clinical Endocrinologists and American College of Endocrinology Disease state clinical review: diagnosis of recurrence in Cushing disease. Endocr Pract. 22:1436–1448. 2016.18. Hakami OA, Ahmed S, Karavitaki N. Epidemiology and mortality of Cushing’s syndrome. Best Pract Res Clin Endocrinol Metab. 35:101521. 2021.19. Hameed N, Yedinak CG, Brzana J, Gultekin SH, Coppa ND, Dogan A, et al. Remission rate after transsphenoidal surgery in patients with pathologically confirmed Cushing’s disease, the role of cortisol, ACTH assessment and immediate reoperation: a large single center experience. Pituitary. 16:452–458. 2013.20. Hardy J, Vezina JL. Transsphenoidal neurosurgery of intracranial neoplasm. Adv Neurol. 15:261–273. 1976.21. Juszczak A, Ertorer ME, Grossman A. The therapy of Cushing’s disease in adults and children: an update. Horm Metab Res. 45:109–117. 2013.22. Knosp E, Steiner E, Kitz K, Matula C. Pituitary adenomas with invasion of the cavernous sinus space: a magnetic resonance imaging classification compared with surgical findings. Neurosurgery. 33:610–617. discussion 617-618. 1993.23. Lambert JK, Goldberg L, Fayngold S, Kostadinov J, Post KD, Geer EB. Predictors of mortality and long-term outcomes in treated Cushing’s disease: a study of 346 patients. J Clin Endocrinol Metab. 98:1022–1030. 2013.24. Lüdecke DK, Flitsch J, Knappe UJ, Saeger W. Cushing’s disease: a surgical view. J Neurooncol. 54:151–166. 2001.25. Mamelak AN, Dowd CF, Tyrrell JB, McDonald JF, Wilson CB. Venous angiography is needed to interpret inferior petrosal sinus and cavernous sinus sampling data for lateralizing adrenocorticotropin-secreting adenomas. J Clin Endocrinol Metab. 81:475–481. 1996.26. McCance DR, McIlrath E, McNeill A, Gordon DS, Hadden DR, Kennedy L, et al. Bilateral inferior petrosal sinus sampling as a routine procedure in ACTH-dependent Cushing’s syndrome. Clin Endocrinol (Oxf). 30:157–166. 1989.27. Netea-Maier RT, van Lindert EJ, den Heijer M, van der Eerden A, Pieters GF, Sweep CG, et al. Transsphenoidal pituitary surgery via the endoscopic technique: results in 35 consecutive patients with Cushing’s disease. Eur J Endocrinol. 154:675–684. 2006.28. Nieman LK, Biller BM, Findling JW, Newell-Price J, Savage MO, Stewart PM, et al. The diagnosis of Cushing’s syndrome: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 93:1526–1540. 2008.29. Oldfield EH, Doppman JL, Nieman LK, Chrousos GP, Miller DL, Katz DA, et al. Petrosal sinus sampling with and without corticotropin-releasing hormone for the differential diagnosis of Cushing’s syndrome. N Engl J Med. 325:897–905. 1991.30. Petersenn S, Beckers A, Ferone D, van der Lely A, Bollerslev J, Boscaro M, et al. Therapy of endocrine disease: outcomes in patients with Cushing’s disease undergoing transsphenoidal surgery: systematic review assessing criteria used to define remission and recurrence. Eur J Endocrinol. 172:R227–R239. 2015.31. Prevedello DM, Pouratian N, Sherman J, Jane JA Jr, Vance ML, Lopes MB, et al. Management of Cushing’s disease: outcome in patients with microadenoma detected on pituitary magnetic resonance imaging. J Neurosurg. 109:751–759. 2008.32. Salenave S, Gatta B, Pecheur S, San-Galli F, Visot A, Lasjaunias P, et al. Pituitary magnetic resonance imaging findings do not influence surgical outcome in adrenocorticotropin-secreting microadenomas. J Clin Endocrinol Metab. 89:3371–3376. 2004.33. Semple PL, Laws ER Jr. Complications in a contemporary series of patients who underwent transsphenoidal surgery for Cushing’s disease. J Neurosurg. 91:175–179. 1999.34. Serban AL, Del Sindaco G, Sala E, Carosi G, Indirli R, Rodari G, et al. Determinants of outcome of transsphenoidal surgery for Cushing disease in a single-centre series. J Endocrinol Invest. 43:631–639. 2020.35. Sharifi G, Amin AA, Sabahi M, Echeverry NB, Dilmaghani NA, Mousavinejad SA, et al. MRI-negative Cushing’s disease: management strategy and outcomes in 15 cases utilizing a pure endoscopic endonasal approach. BMC Endocr Disord. 22:154. 2022.36. Sun Y, Sun Q, Fan C, Shen J, Zhao W, Guo Y, et al. Diagnosis and therapy for Cushing’s disease with negative dynamic MRI finding: a singlecentre experience. Clin Endocrinol (Oxf). 76:868–876. 2012.37. Valassi E, Biller BM, Swearingen B, Pecori Giraldi F, Losa M, Mortini P, et al. Delayed remission after transsphenoidal surgery in patients with Cushing’s disease. J Clin Endocrinol Metab. 95:601–610. 2010.38. Valderrábano P, Aller J, García-Valdecasas L, García-Uría J, Martín L, Palacios N, et al. Results of repeated transsphenoidal surgery in Cushing’s disease. Long-term follow-up. Endocrinol Nutr. 61:176–183. 2014.39. Wilson CB. A decade of pituitary microsurgery. The Herbert Olivecrona lecture. J Neurosurg. 61:814–833. 1984.40. Yamada S, Fukuhara N, Nishioka H, Takeshita A, Inoshita N, Ito J, et al. Surgical management and outcomes in patients with Cushing disease with negative pituitary magnetic resonance imaging. World Neurosurg. 77:525–532. 2012.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Treatment of Cushing’s disease with macroadenoma through transsphenoidal surgery
- The Results of Transsphenoidal Microsurgery for Pituitary Microadenama in Cushing's Disease
- Long-term follow-up on Cushing disease patient after transsphenoidal surgery
- A Case of Cushing's Disease in Pregnancy
- A Case of Persistent Cushing's Syndrome