J Korean Neurosurg Soc.
2024 Mar;67(2):177-185. 10.3340/jkns.2023.0182.
Monocyte Count and Systemic Immune-Inflammation Index Score as Predictors of Delayed Cerebral Ischemia after Aneurysmal Subarachnoid Hemorrhage
- Affiliations
-
- 1Department of Neurosurgery, Ajou University Hospital, Ajou University School of Medicine, Suwon, Korea
- KMID: 2553123
- DOI: http://doi.org/10.3340/jkns.2023.0182
Abstract
Objective
: Delayed cerebral ischemia (DCI) is a major cause of disability in patients who survive aneurysmal subarachnoid hemorrhage (aSAH). Systemic inflammatory markers, such as peripheral leukocyte count and systemic immune-inflammatory index (SII) score, have been considered predictors of DCI in previous studies. This study aims to investigate which systemic biomarkers are significant predictors of DCI.
Methods
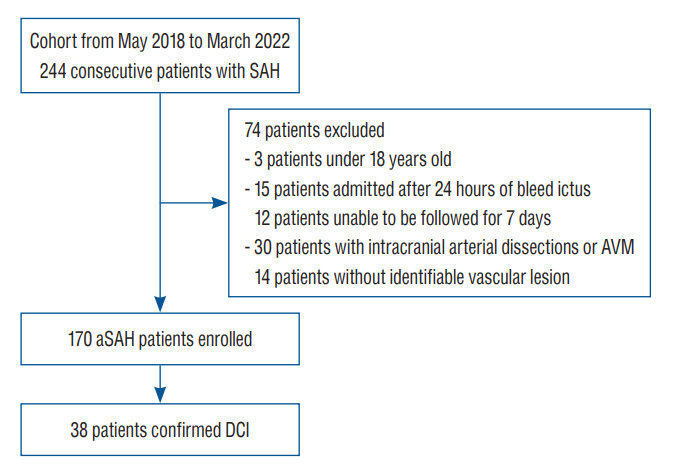
: We conducted a retrospective, observational, single-center study of 170 patients with SAH admitted between May 2018 and March 2022. We analyzed the patients’ clinical and laboratory parameters within 1 hour and 3–4 and 5–7 days after admission. The DCI and non-DCI groups were compared. Variables showing statistical significance in the univariate logistic analysis (p<0.05) were entered into a multivariate regression model.
Results
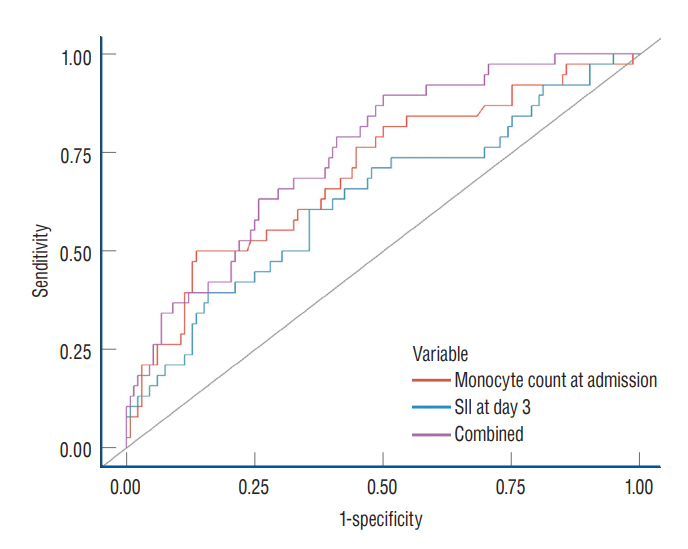
: Hunt-Hess grade “4–5” at admission, modified Fisher scale grade “3–4” at admission, hydrocephalus, intraventricular hemorrhage, and infection showed statistical significance (p<0.05) on a univariate logistic regression. Lymphocyte and monocyte count at admission, SII scores and C-reactive protein levels on days 3–4, and leukocyte and neutrophil counts on days 5–7 exhibited statistical significance on the univariate logistic regression. Multivariate logistic regression analysis revealed that monocyte count at admission (odds ratio [OR], 1.64; 95% confidence interval [CI], 1.04–2.65; p=0.036) and SII score at days 3–4 (OR, 1.55; 95% CI, 1.02–2.47; p=0.049) were independent predictors of DCI.
Conclusion
: Monocyte count at admission and SII score 3–4 days after rupture are independent predictors of clinical deterioration caused by DCI after aSAH. Peripheral monocytosis may be the primer for the innate immune reaction, and the SII score at days 3–4 can promptly represent the propagated systemic immune reaction toward DCI.
Keyword
Figure
Reference
-
References
1. Bacigaluppi S, Ivaldi F, Bragazzi NL, Benvenuto F, Gallo F, D’Andrea A, et al. An early increase of blood leukocyte subsets in aneurysmal subarachnoid hemorrhage is predictive of vasospasm. Front Neurol. 11:587039. 2020.2. Balança B, Bouchier B, Ritzenthaler T. The management of delayed cerebral ischemia after aneurysmal subarachnoid hemorrhage. Rev Neurol (Paris). 178:64–73. 2022.3. Bederson JB, Levy AL, Ding WH, Kahn R, DiPerna CA, Jenkins AL 3rd, et al. Acute vasoconstriction after subarachnoid hemorrhage. Neurosurgery. 42:352–360. discussion 360-362. 1998.4. Chen L, Pandey S, Shen R, Xu Y, Zhang Q. Increased systemic immuneinflammation index is associated with delayed cerebral ischemia in aneurysmal subarachnoid hemorrhage patients. Front Neurol. 12:745175. 2021.5. Connolly ES Jr, Rabinstein AA, Carhuapoma JR, Derdeyn CP, Dion J, Higashida RT, et al. Guidelines for the management of aneurysmal subarachnoid hemorrhage: a guideline for healthcare professionals from the American Heart Association/american Stroke Association. Stroke. 43:1711–1737. 2012.6. Dzenko KA, Song L, Ge S, Kuziel WA, Pachter JS. CCR2 expression by brain microvascular endothelial cells is critical for macrophage transendothelial migration in response to CCL2. Microvasc Res. 70:53–64. 2005.7. Geraghty JR, Davis JL, Testai FD. Neuroinflammation and microvascular dysfunction after experimental subarachnoid hemorrhage: emerging components of early brain injury related to outcome. Neurocrit Care. 31:373–389. 2019.8. Geraghty JR, Lung TJ, Hirsch Y, Katz EA, Cheng T, Saini NS, et al. Systemic immune-inflammation index predicts delayed cerebral vasospasm after aneurysmal subarachnoid hemorrhage. Neurosurgery. 89:1071–1079. 2021.9. Gusdon AM, Savarraj JPJ, Shihabeddin E, Paz A, Assing A, Ko SB, et al. Time course of peripheral leukocytosis and clinical outcomes after aneurysmal subarachnoid hemorrhage. Front Neurol. 12:694996. 2021.10. Lawton MT, Vates GE. Subarachnoid hemorrhage. N Engl J Med. 377:257–266. 2017.11. Lee H, Perry JJ, English SW, Alkherayf F, Joseph J, Nobile S, et al. Clinical prediction of delayed cerebral ischemia in aneurysmal subarachnoid hemorrhage. J Neurosurg. 130:1914–1921. 2018.12. Ma C, Zhou W, Yan Z, Qu M, Bu X. Toll-like receptor 4 (TLR4) is associated with cerebral vasospasm and delayed cerebral ischemia in aneurysmal subarachnoid hemorrhage. Neurol Med Chir (Tokyo). 55:878–884. 2015.13. Macdonald RL, Higashida RT, Keller E, Mayer SA, Molyneux A, Raabe A, et al. Randomised trial of clazosentan, an endothelin receptor antagonist, in patients with aneurysmal subarachnoid hemorrhage undergoing surgical clipping (CONSCIOUS-2). Acta Neurochir Suppl. 115:27–31. 2013.14. Macdonald RL, Higashida RT, Keller E, Mayer SA, Molyneux A, Raabe A, et al. Randomized trial of clazosentan in patients with aneurysmal subarachnoid hemorrhage undergoing endovascular coiling. Stroke. 43:1463–1469. 2012.15. Maruhashi T, Higashi Y. An overview of pharmacotherapy for cerebral vasospasm and delayed cerebral ischemia after subarachnoid hemorrhage. Expert Opin Pharmacother. 22:1601–1614. 2021.16. McMahon CJ, Hopkins S, Vail A, King AT, Smith D, Illingworth KJ, et al. Inflammation as a predictor for delayed cerebral ischemia after aneurysmal subarachnoid haemorrhage. J Neurointerv Surg. 5:512–517. 2013.17. Provencio JJ. Inflammation in subarachnoid hemorrhage and delayed deterioration associated with vasospasm: a review. Acta Neurochir Suppl. 115:233–238. 2013.18. Ray B, Tinsley L, Ford L, Thompson DM, Sidorov EV, Bohnstedt BN. Trends of platelet volume index predicts delayed cerebral ischemia after subarachnoid hemorrhage. World Neurosurg. 111:e624–e631. 2018.19. Shi H, Jiang Y, Cao H, Zhu H, Chen B, Ji W. Nomogram based on systemic immune-inflammation index to predict overall survival in gastric cancer patients. Dis Markers. 2018:1787424. 2018.20. Srinivasan A, Aggarwal A, Gaudihalli S, Mohanty M, Dhandapani M, Singh H, et al. Impact of early leukocytosis and elevated high-sensitivity C-reactive protein on delayed cerebral ischemia and neurologic outcome after subarachnoid hemorrhage. World Neurosurg. 90:91–95. 2016.21. Suzuki H, Kanamaru H, Kawakita F, Asada R, Fujimoto M, Shiba M. Cerebrovascular pathophysiology of delayed cerebral ischemia after aneurysmal subarachnoid hemorrhage. Histol Histopathol. 36:143–158. 2021.22. Unda SR, Birnbaum J, Labagnara K, Wong M, Vaishnav DP, Altschul DJ. Peripheral monocytosis at admission to predict cerebral infarct and poor functional outcomes in subarachnoid hemorrhage patients. World Neurosurg. 138:e523–e529. 2020.23. Vergouwen MD, Vermeulen M, van Gijn J, Rinkel GJ, Wijdicks EF, Muizelaar JP, et al. Definition of delayed cerebral ischemia after aneurysmal subarachnoid hemorrhage as an outcome event in clinical trials and observational studies: proposal of a multidisciplinary research group. Stroke. 41:2391–2395. 2010.24. Wang Z, Pei W, Chen L, Ning Y, Luo Y. Mean platelet volume/platelet count ratio is associated with poor clinical outcome after aneurysmal subarachnoid hemorrhage. J Stroke Cerebrovasc Dis. 29:105208. 2020.25. Xie QK, Chen P, Hu WM, Sun P, He WZ, Jiang C, et al. The systemic immune-inflammation index is an independent predictor of survival for metastatic colorectal cancer and its association with the lymphocytic response to the tumor. J Transl Med. 16:273. 2018.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Corrigendum to “Monocyte Count and Systemic Immune-Inflammation Index Score as Predictors of Delayed Cerebral Ischemia after Aneurysmal Subarachnoid Hemorrhage” by Lee et al. (J Korean Neurosurg Soc 67 : 177-185, 2024)
- Relation between Thromboembolism and Delayed Ischemic Neurological Deficits in Aneurysmal Subarachnoid Hemorrhage
- Two Cases of Subarachnoid Hemorrhage from Spontaneous Anterior Cerebral Artery Dissection : A Case of Simultaneous Hemorrhage and Ischemia Without Aneurysmal Formation and Another Case of Hemorrhage with Aneurysmal Formation
- Hemodynamics of Poor-grade Subarachnoid Hemorrhage
- Thromboembolism: Another substantial cause of delayed ischemic neurologic deficits after aneurysmal subarachnoid hemorrhage