J Korean Foot Ankle Soc.
2023 Dec;27(4):137-143. 10.14193/jkfas.2023.27.4.137.
Intermediate-Term Clinical Outcomes after Autologous Osteochondral Transplantation for Lateral Osteochondral Lesions of the Talus
- Affiliations
-
- 1Department of Orthopedic Surgery, Chungbuk National University Hospital, Cheongju, Korea
- KMID: 2552993
- DOI: http://doi.org/10.14193/jkfas.2023.27.4.137
Abstract
- Purpose
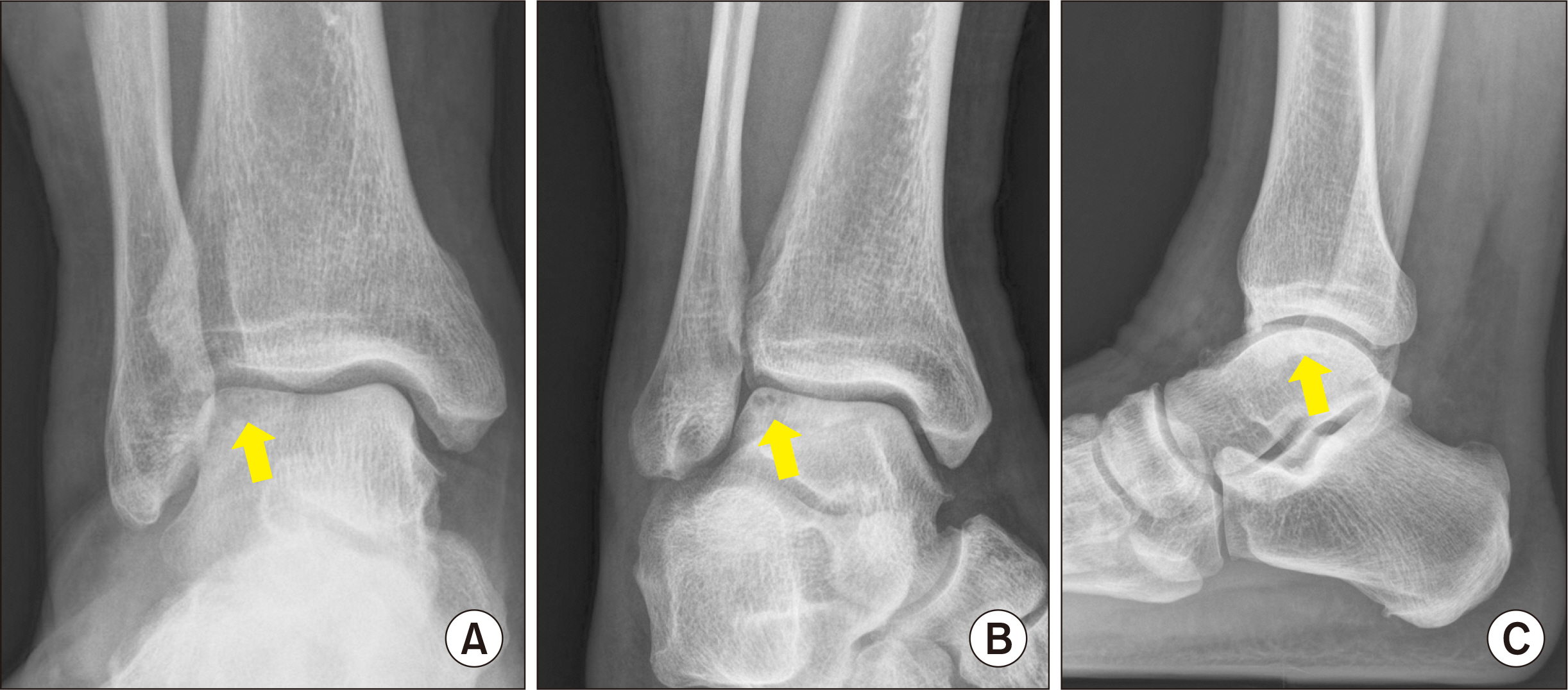
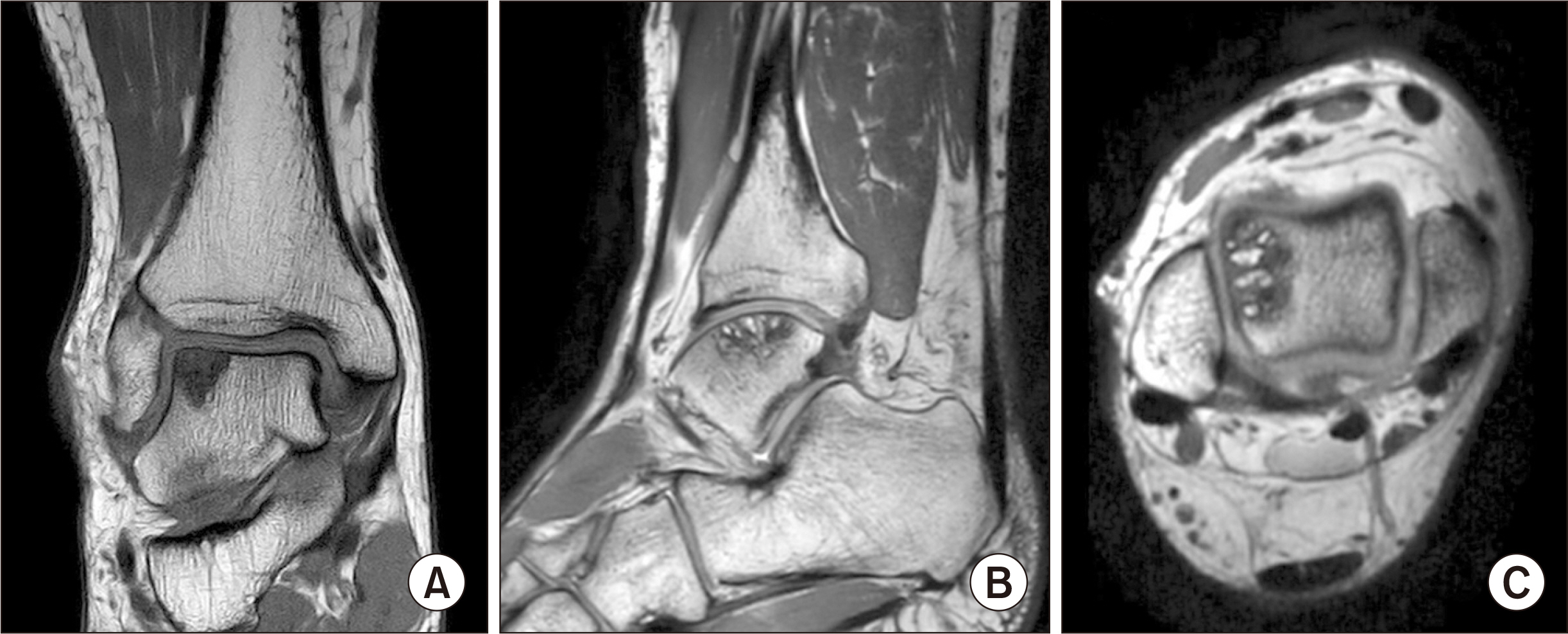
Autologous osteochondral transplantation (AOT) is indicated for patients with a large osteochondral lesion of the talus (OLT), accompanying subchondral cyst, and the failure of bone marrow stimulation (BMS) procedures. Despite the many reports on the clinical results of surgical treatment for medial osteochondral lesions, those of lateral lesions are rare. This paper reports the intermediate-term clinical outcomes after AOT for lateral OLTs.
Materials and Methods
Twenty-one patients with lateral OLTs were followed up for at least three years after AOT. The clinical evaluations comprised the Foot and Ankle Outcome Score (FAOS) and Foot and Ankle Ability Measure (FAAM). The radiographic assessment included the irregularity of the articular surface (subchondral plate), the progression of degenerative arthritis, and the changes in talar tilt angle and anterior talar translation.
Results
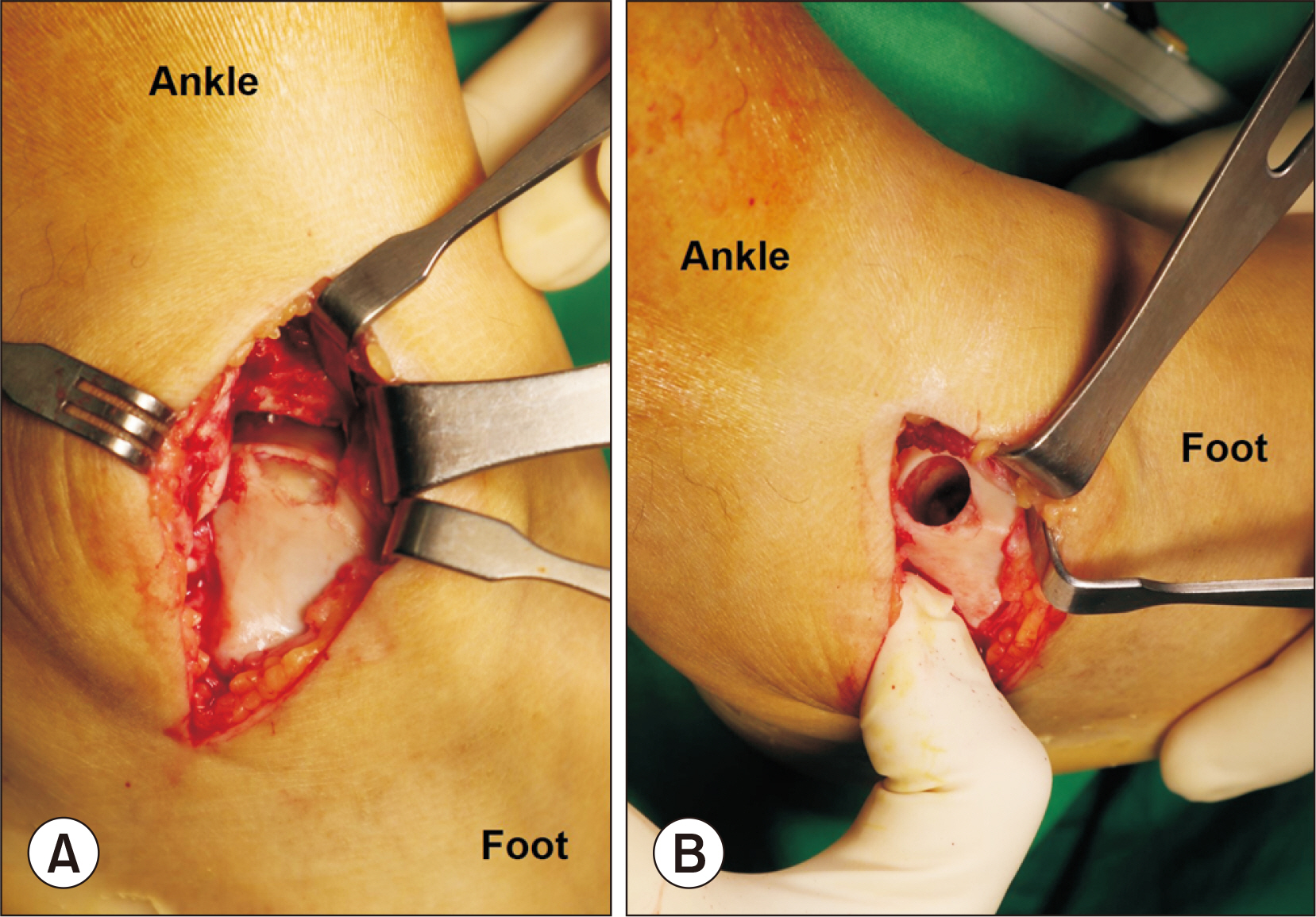
The mean FAOS and FAAM scores improved significantly from 42.1 to 89.5 and 39.5 to 90.6 points, respectively, at the final follow-up (p<0.001). The radiological evaluation revealed two cases (9.5%) of articular step-off ≥2 mm and 1 case (4.8%) of progressive arthritis. The mean talar tilt angle and anterior talar translation improved significantly. As postoperative complications, there was one case of a local wound problem, one case of superficial peroneal nerve injury, and one case of donor site morbidity. At a mean follow-up of 62.3 months, no patient showed a recurrence of instability or required reoperation for OLT.
Conclusion
AOT for the lateral OLTs demonstrated satisfactory intermediate-term clinical outcomes, including daily and sports activity abilities. Most OLT could be accessed through lateral ligament division and capsulotomy, and the incidence of iatrogenic complications, such as recurrent sprains or chronic instability, was minimal. AOT appears to be an effective and relatively safe treatment for patients with large lateral osteochondral lesions unresponsive to conservative therapy, with subchondral cysts, or with failed primary BMS.
Figure
Reference
-
References
1. Shimozono Y, Hurley ET, Nguyen JT, Deyer TW, Kennedy JG. 2018; Allograft compared with autograft in osteochondral transplantation for the treatment of osteochondral lesions of the talus. J Bone Joint Surg Am. 100:1838–44. doi: 10.2106/JBJS.17.01508. DOI: 10.2106/JBJS.17.01508. PMID: 30399078.
Article2. Prado MP, Kennedy JG, Raduan F, Nery C. 2016; Diagnosis and treatment of osteochondral lesions of the ankle: current concepts. Rev Bras Ortop. 51:489–500. doi: 10.1016/j.rboe.2016.08.007. DOI: 10.1016/j.rboe.2016.08.007. PMID: 27818968. PMCID: PMC5091026.
Article3. Murawski CD, Kennedy JG. 2013; Operative treatment of osteochondral lesions of the talus. J Bone Joint Surg Am. 95:1045–54. doi: 10.2106/JBJS.L.00773. DOI: 10.2106/JBJS.L.00773. PMID: 23780543.
Article4. Yoon HS, Park YJ, Lee M, Choi WJ, Lee JW. 2014; Osteochondral autologous transplantation is superior to repeat arthroscopy for the treatment of osteochondral lesions of the talus after failed primary arthroscopic treatment. Am J Sports Med. 42:1896–903. doi: 10.1177/0363546514535186. DOI: 10.1177/0363546514535186. PMID: 24907287.
Article5. Savage-Elliott I, Ross KA, Smyth NA, Murawski CD, Kennedy JG. 2014; Osteochondral lesions of the talus: a current concepts review and evidence-based treatment paradigm. Foot Ankle Spec. 7:414–22. doi: 10.1177/1938640014543362. DOI: 10.1177/1938640014543362. PMID: 25100765.6. Shim DW, Park KH, Lee JW, Yang YJ, Shin J, Han SH. 2021; Primary autologous osteochondral transfer shows superior long-term outcome and survival rate compared with bone marrow stimulation for large cystic osteochondral lesion of talus. Arthroscopy. 37:989–97. doi: 10.1016/j.arthro.2020.11.038. DOI: 10.1016/j.arthro.2020.11.038. PMID: 33276050.
Article7. Mittwede PN, Murawski CD, Ackermann J, Görtz S, Hintermann B, Kim HJ, et al. 2018; Revision and salvage management: proceedings of the International Consensus Meeting on Cartilage Repair of the Ankle. Foot Ankle Int. 39(1_suppl):54S–60S. doi: 10.1177/1071100718781863. Erratum in: Foot Ankle Int. 2021;42:248.DOI: 10.1177/1071100718781863. PMID: 30215315.8. Hangody L, Füles P. Autologous osteochondral mosaicplasty for the treatment of full-thickness defects of weight-bearing joints: ten years of experimental and clinical experience. J Bone Joint Surg Am. 2003; 85-A Suppl 2:25–32. doi: 10.2106/00004623-200300002-00004. DOI: 10.2106/00004623-200300002-00004. PMID: 12721342.9. Al-Shaikh RA, Chou LB, Mann JA, Dreeben SM, Prieskorn D. 2002; Autologous osteochondral grafting for talar cartilage defects. Foot Ankle Int. 23:381–9. doi: 10.1177/107110070202300502. DOI: 10.1177/107110070202300502. PMID: 12043980.
Article10. Hangody L, Dobos J, Baló E, Pánics G, Hangody LR, Berkes I. 2010; Clinical experiences with autologous osteochondral mosaicplasty in an athletic population: a 17-year prospective multicenter study. Am J Sports Med. 38:1125–33. doi: 10.1177/0363546509360405. DOI: 10.1177/0363546509360405. PMID: 20360608.
Article11. Hangody L, Kish G, Módis L, Szerb I, Gáspár L, Diószegi Z, et al. 2001; Mosaicplasty for the treatment of osteochondritis dissecans of the talus: two to seven year results in 36 patients. Foot Ankle Int. 22:552–8. doi: 10.1177/107110070102200704. DOI: 10.1177/107110070102200704. PMID: 11503979.
Article12. Scranton PE Jr, Frey CC, Feder KS. 2006; Outcome of osteochondral autograft transplantation for type-V cystic osteochondral lesions of the talus. J Bone Joint Surg Br. 88:614–9. doi: 10.1302/0301-620X.88B5.17306. DOI: 10.1302/0301-620X.88B5.17306. PMID: 16645106.
Article13. Hurley ET, Murawski CD, Paul J, Marangon A, Prado MP, Xu X, et al. 2018; Osteochondral autograft: proceedings of the International Consensus Meeting on Cartilage Repair of the Ankle. Foot Ankle Int. 39(1_suppl):28S–34S. doi: 10.1177/1071100718781098. Erratum in: Foot Ankle Int. 2021;42:248. DOI: 10.1177/1071100718781098. PMID: 30215309.14. Cuttica DJ, Smith WB, Hyer CF, Philbin TM, Berlet GC. 2011; Osteochondral lesions of the talus: predictors of clinical outcome. Foot Ankle Int. 32:1045–51. doi: 10.3113/FAI.2011.104. DOI: 10.3113/FAI.2011.104. PMID: 22338953.
Article15. Deol PP, Cuttica DJ, Smith WB, Berlet GC. 2013; Osteochondral lesions of the talus: size, age, and predictors of outcomes. Foot Ankle Clin. 18:13–34. doi: 10.1016/j.fcl.2012.12.010. DOI: 10.1016/j.fcl.2012.12.010. PMID: 23465946.16. Martin RL, Irrgang JJ, Burdett RG, Conti SF, Van Swearingen JM. 2005; Evidence of validity for the Foot and Ankle Ability Measure (FAAM). Foot Ankle Int. 26:968–83. doi: 10.1177/107110070502601113. DOI: 10.1177/107110070502601113. PMID: 16309613.17. Roos EM, Brandsson S, Karlsson J. 2001; Validation of the foot and ankle outcome score for ankle ligament reconstruction. Foot Ankle Int. 22:788–94. doi: 10.1177/107110070102201004. DOI: 10.1177/107110070102201004. PMID: 11642530.
Article18. Lee KM, Chung CY, Kwon SS, Sung KH, Lee SY, Won SH, et al. 2013; Transcultural adaptation and testing psychometric properties of the Korean version of the Foot and Ankle Outcome Score (FAOS). Clin Rheumatol. 32:1443–50. doi: 10.1007/s10067-013-2288-1. DOI: 10.1007/s10067-013-2288-1. PMID: 23703359.
Article19. Verhagen RA, Struijs PA, Bossuyt PM, van Dijk CN. 2003; Systematic review of treatment strategies for osteochondral defects of the talar dome. Foot Ankle Clin. 8:233–42. viii–ix. doi: 10.1016/s1083-7515(02)00064-5. DOI: 10.1016/S1083-7515(02)00064-5. PMID: 12911238.
Article20. Dahmen J, Lambers KTA, Reilingh ML, van Bergen CJA, Stufkens SAS, Kerkhoffs GMMJ. 2018; No superior treatment for primary osteochondral defects of the talus. Knee Surg Sports Traumatol Arthrosc. 26:2142–57. doi: 10.1007/s00167-017-4616-5. DOI: 10.1007/s00167-017-4616-5. PMID: 28656457. PMCID: PMC6061466.
Article21. O'Loughlin PF, Heyworth BE, Kennedy JG. 2010; Current concepts in the diagnosis and treatment of osteochondral lesions of the ankle. Am J Sports Med. 38:392–404. doi: 10.1177/036354650933633. DOI: 10.1177/036354650933633. PMID: 19561175.22. Dekker TJ, Dekker PK, Tainter DM, Easley ME, Adams SB. 2017; Treatment of osteochondral lesions of the talus: a critical analysis review. JBJS Rev. 5:e4. doi: 10.2106/JBJS.RVW.16.00065. DOI: 10.2106/JBJS.RVW.16.00065. PMID: 28359070.23. Zengerink M, Struijs PA, Tol JL, van Dijk CN. 2010; Treatment of osteochondral lesions of the talus: a systematic review. Knee Surg Sports Traumatol Arthrosc. 18:238–46. doi: 10.1007/s00167-009-0942-6. DOI: 10.1007/s00167-009-0942-6. PMID: 19859695. PMCID: PMC2809940.
Article24. Paul J, Sagstetter M, Lämmle L, Spang J, El-Azab H, Imhoff AB, et al. 2012; Sports activity after osteochondral transplantation of the talus. Am J Sports Med. 40:870–4. doi: 10.1177/0363546511435084. DOI: 10.1177/0363546511435084. PMID: 22268232.
Article25. Fraser EJ, Harris MC, Prado MP, Kennedy JG. 2016; Autologous osteochondral transplantation for osteochondral lesions of the talus in an athletic population. Knee Surg Sports Traumatol Arthrosc. 24:1272–9. doi: 10.1007/s00167-015-3606-8. DOI: 10.1007/s00167-015-3606-8. PMID: 25962962.
Article26. Muir D, Saltzman CL, Tochigi Y, Amendola N. 2006; Talar dome access for osteochondral lesions. Am J Sports Med. 34:1457–63. doi: 10.1177/0363546506287296. DOI: 10.1177/0363546506287296. PMID: 16636351.
Article27. de Araujo MK, de Cillo MS, Bittar CK, Zabeu JL, Cezar CN. 2016; Arthroscopic treatment of osteochondral lesions of the talus. Acta Ortop Bras. 24:32–4. doi: 10.1590/1413-785220162401137414. DOI: 10.1590/1413-785220162401137414. PMID: 26997911. PMCID: PMC4775486.
Article28. Woelfle JV, Reichel H, Nelitz M. 2013; Indications and limitations of osteochondral autologous transplantation in osteochondritis dissecans of the talus. Knee Surg Sports Traumatol Arthrosc. 21:1925–30. doi: 10.1007/s00167-013-2483-2. DOI: 10.1007/s00167-013-2483-2. PMID: 23552666.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Autologous Osteochondral Transplantation as a Secondary Procedure after Failed Microfracture for Osteochondral Lesion of Talus
- Simultaneously Occurred Medial and Lateral Osteochondral Lesions of the Talus
- Osteochondral Lesions of the Talus: Autologous Osteochondral Transplantation
- Autologous Chondrocyte Implantation as a Secondary Procedure after Failed Microfracture for Osteochondral Lesion of Talus
- The Clinical Results of Autologous Osteochondral Grafts in Osteochondral Lesion of the Talus