J Surg Ultrasound.
2023 May;10(1):1-7. 10.46268/jsu.2023.10.1.1.
Ultrasonographic Evaluation of Cervical Lymph Nodes
- Affiliations
-
- 1Department of Surgery, Goo Hospital, Daegu, Korea
- KMID: 2552568
- DOI: http://doi.org/10.46268/jsu.2023.10.1.1
Abstract
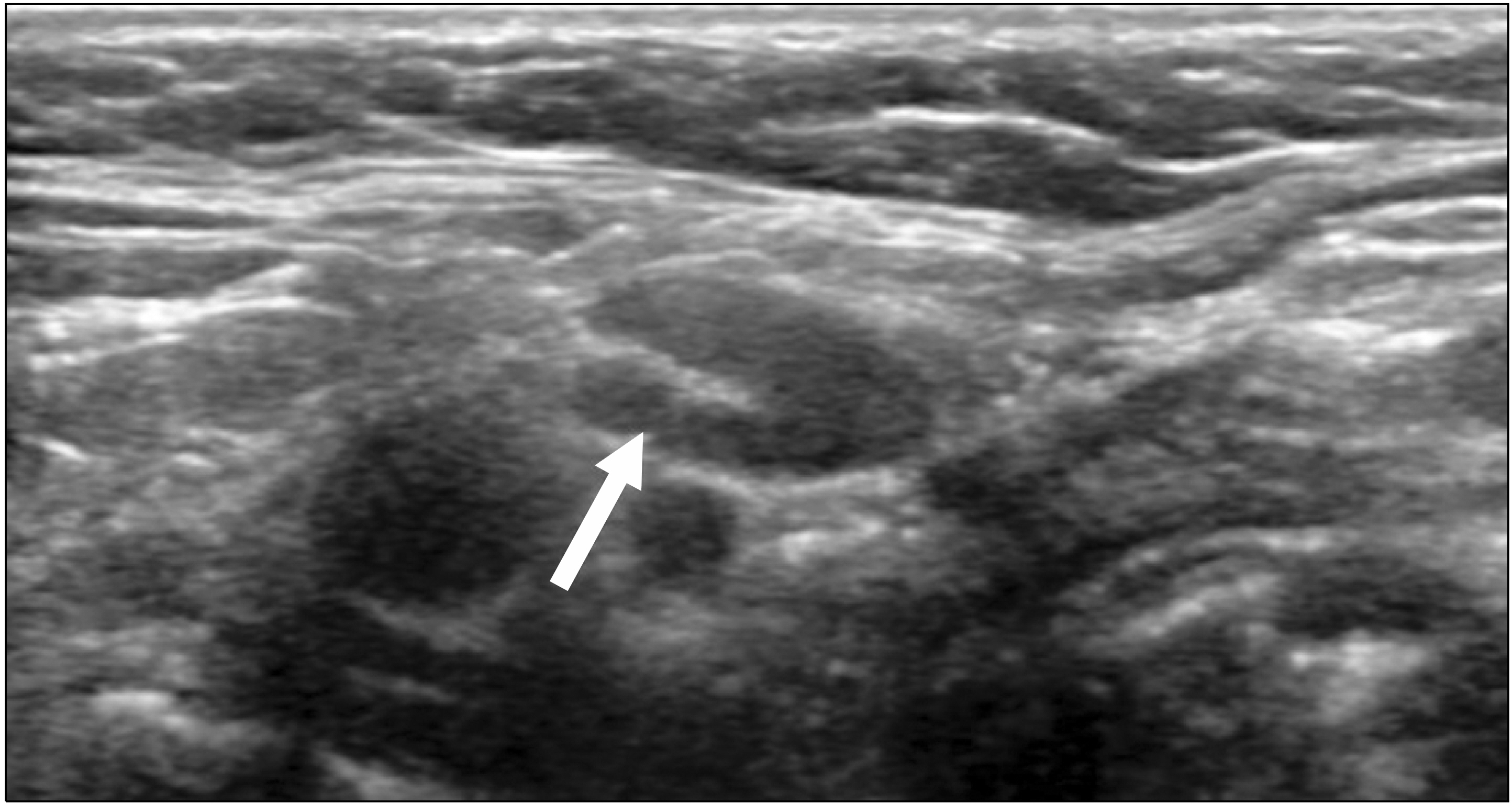
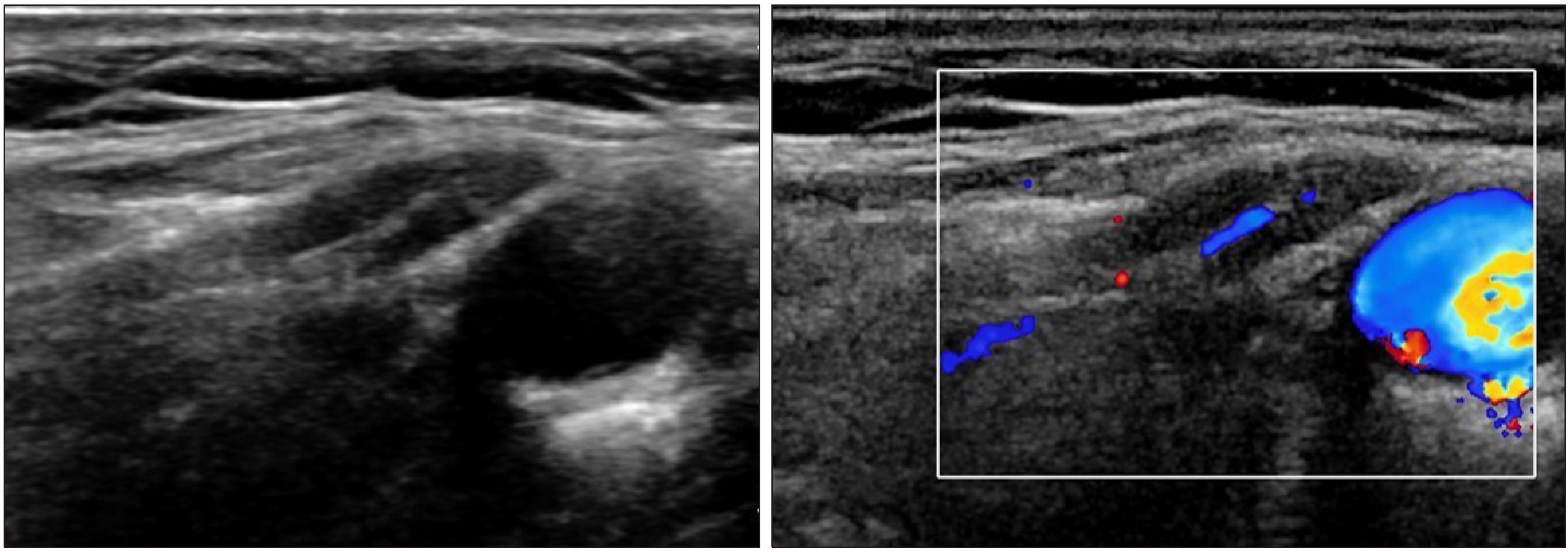
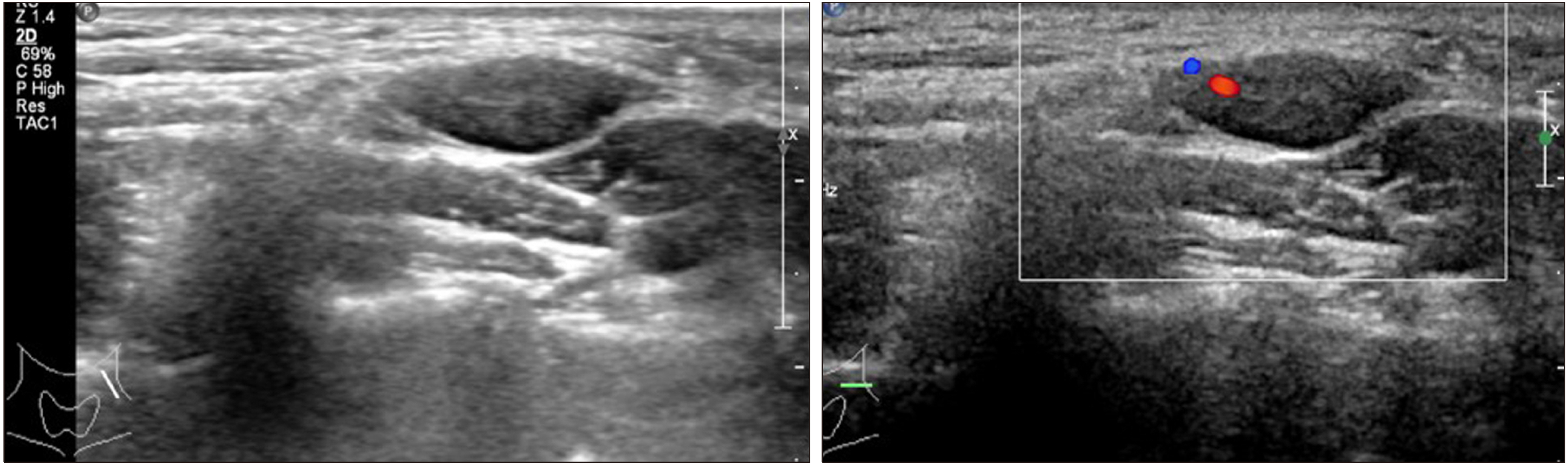
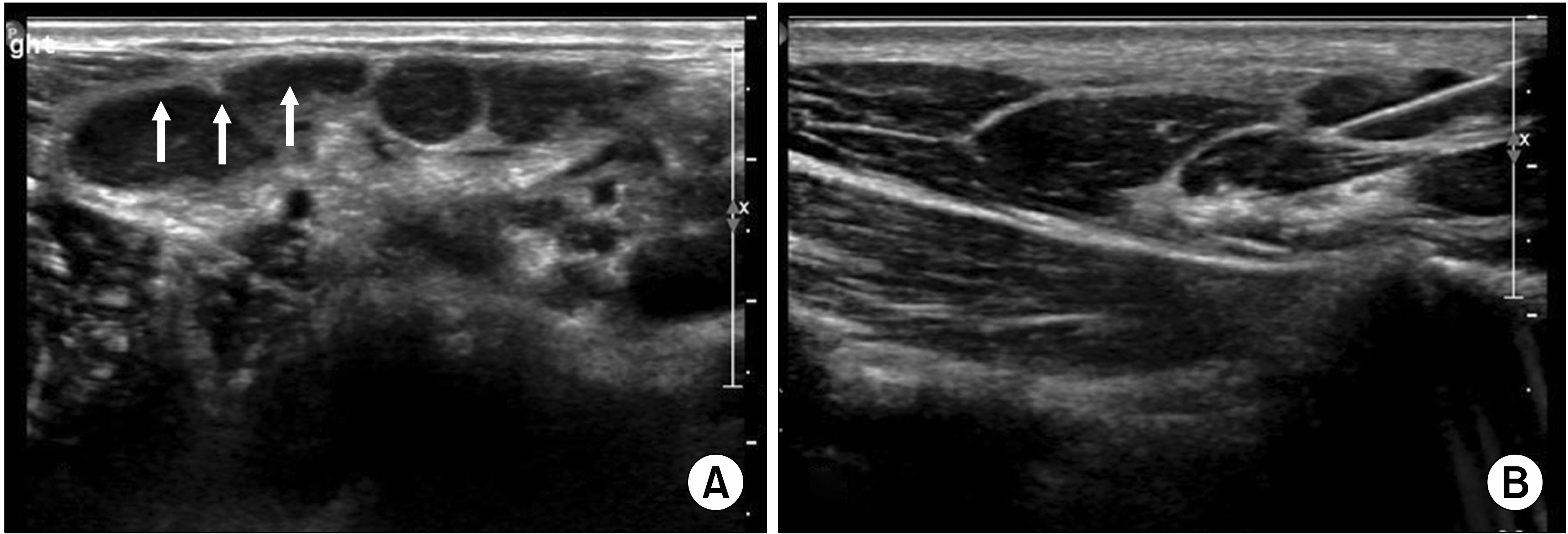
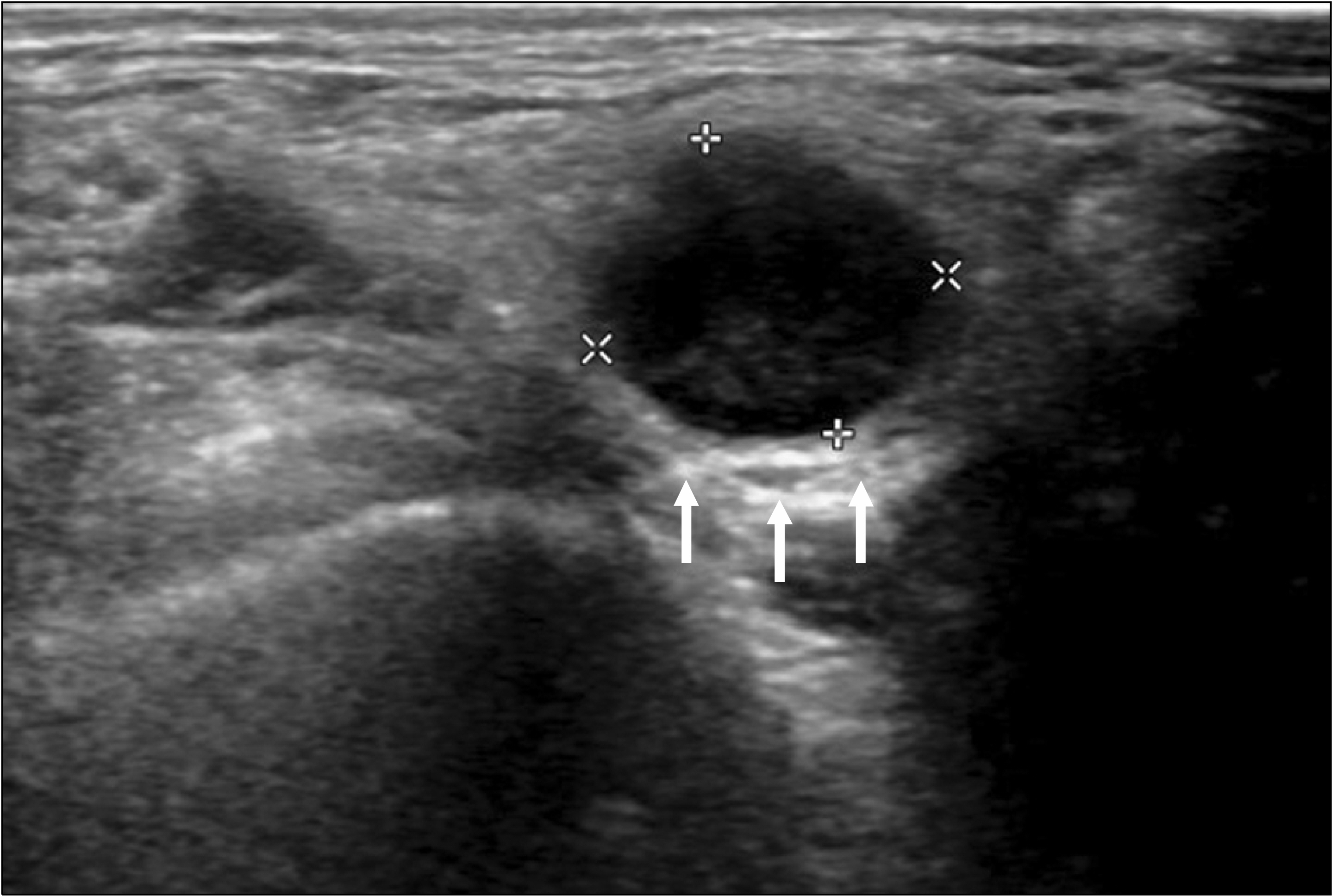
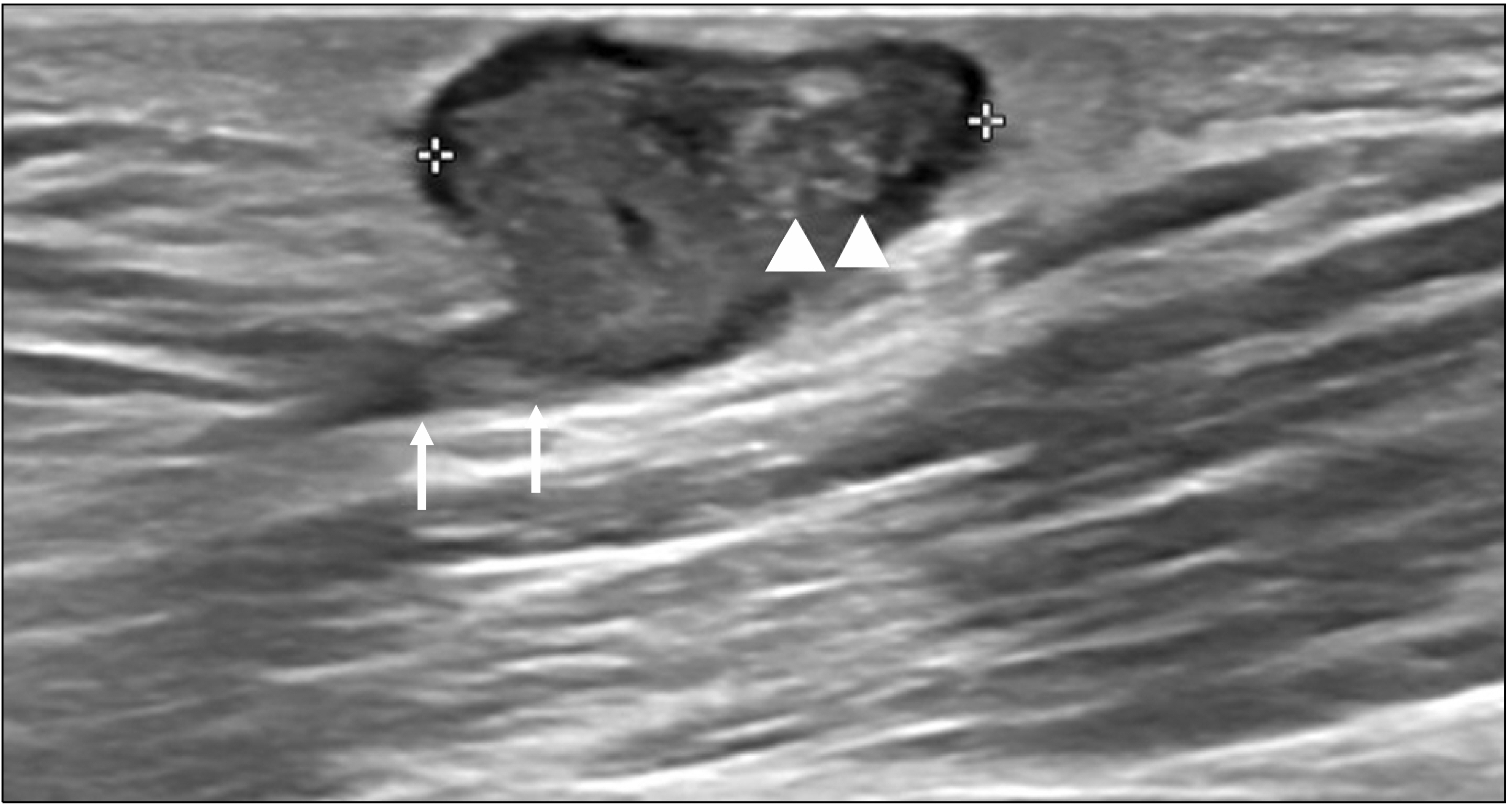
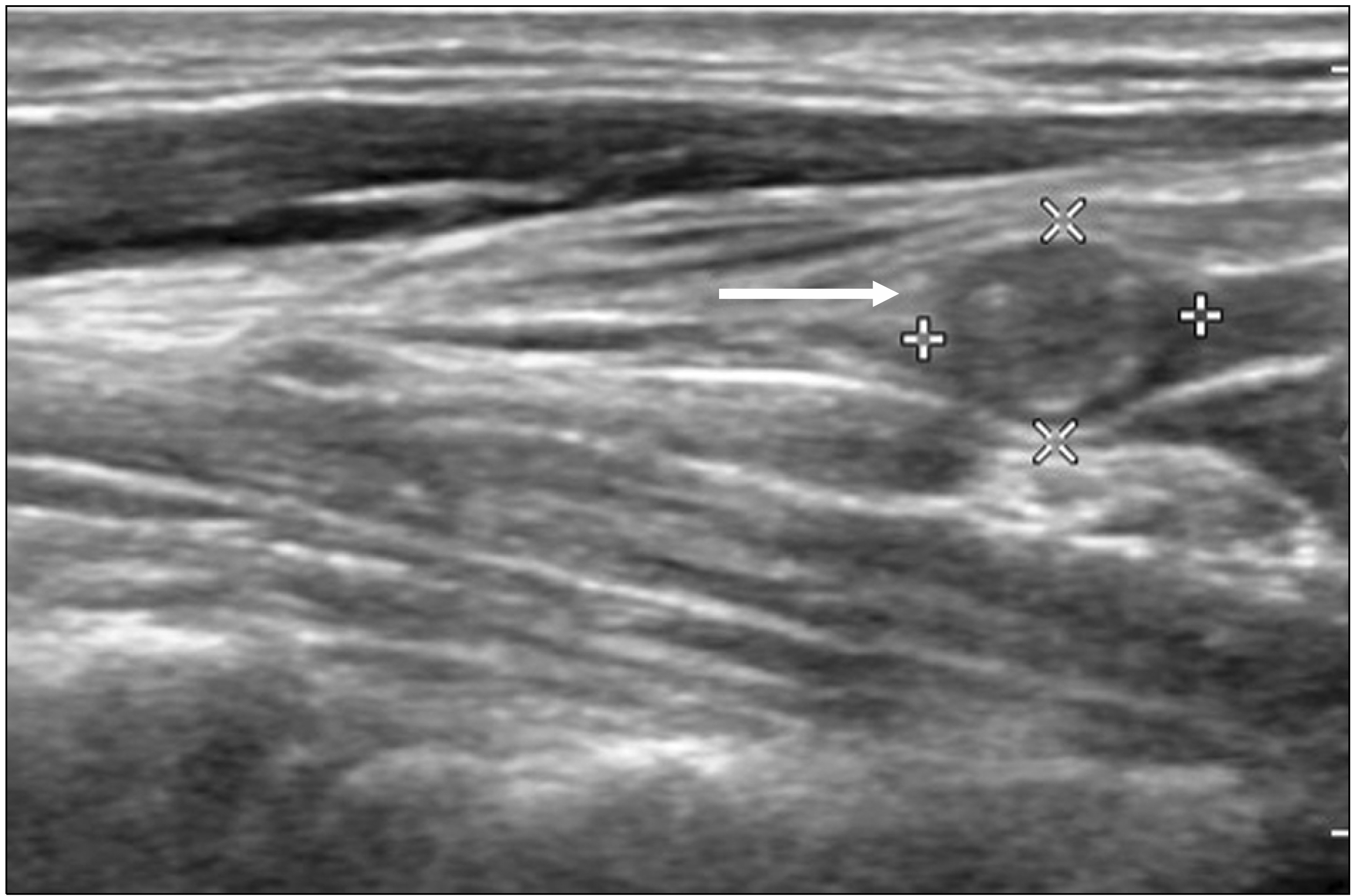
- There are about 200 lymph nodes in the neck, and lymph node enlargement can occur due to various diseases. Most cases of lymph node enlargement can be attributed to reactive lymph nodes due to an upper respiratory tract infection or inflammation of the head-neck area. However, lymph node enlargement can also occur due to viral or bacterial acute lymphadenitis, tuberculous lymphadenitis, histiocytic necrotizing lymphadenitis, malignant lymphoma, metastasis from other organs, etc. Therefore, for an accurate differential diagnosis, a comprehensive judgment must be made through the patient's past medical history, clinical symptoms, hematological findings, and imaging studies. Among imaging studies, ultrasonography is a widely used and valuable imaging modality in the evaluation of cervical lymph nodes due to its noninvasive nature, low cost, and high accuracy in detecting changes in the morphology and blood flow of the lymph nodes. It is an essential tool for the diagnosis and differential diagnosis of cervical lymphadenopathy. Therefore, in this article, the ultrasonographic findings of normal cervical lymph nodes, inflammatory cervical lymph node enlargement, and cervical lymph node metastasis due to thyroid cancer are reviewed.
Keyword
Figure
Reference
-
1. Stack BC Jr, Ferris RL, Goldenberg D, Haymart M, Shaha A, Sheth S, et al. 2012; American Thyroid Association consensus review and statement regarding the anatomy, terminology, and rationale for lateral neck dissection in differentiated thyroid cancer. Thyroid. 22:501–8. DOI: 10.1089/thy.2011.0312. PMID: 22435914.
Article2. Cheung YC, Wan YL, Lui KW, Lee KF. 2000; Sonographically guided core-needle biopsy in the diagnosis of superficial lymphade-nopathy. J Clin Ultrasound. 28:283–9. DOI: 10.1002/1097-0096(200007/08)28:6<283::AID-JCU3>3.0.CO;2-T. PMID: 10867666.
Article3. Robbins KT, Medina JE, Wolfe GT, Levine PA, Sessions RB, Pruet CW. 1991; Standardizing neck dissection terminology. Official report of the Academy's Committee for Head and Neck Surgery and Oncology. Arch Otolaryngol Head Neck Surg. 117:601–5. DOI: 10.1001/archotol.1991.01870180037007. PMID: 2036180.
Article4. American Institute of Ultrasound in Medicine. 2003; AIUM Practice Guideline for the performance of thyroid and parathyroid ultrasound examination. J Ultrasound Med. 22:1126–30. DOI: 10.7863/jum.2003.22.10.1126. PMID: 14606572.5. Solbiati L, Osti V, Cova L, Tonolini M. 2001; Ultrasound of thyroid, parathyroid glands and neck lymph nodes. Eur Radiol. 11:2411–24. DOI: 10.1007/s00330-001-1163-7. PMID: 11734934.
Article6. Kikuchi M. 1972; Lymphadenitis showing focal reticulin cell hyperplasia with nuclear debris and phagocytes: a clinicopathological study. Nihon Ketsueki Gakkai Zasshi. 35:379–80.7. Bosch X, Guilabert A, Miquel R, Campo E. 2004; Enigmatic Kikuchi- Fujimoto disease: a comprehensive review. Am J Clin Pathol. 122:141–52. DOI: 10.1309/YF081L4TKYWVYVPQ. PMID: 15272543.8. Yoo JL, Suh SI, Lee YH, Seo HS, Kim KM, Shin BK, et al. 2011; Gray scale and power Doppler study of biopsy-proven Kikuchi disease. J Ultrasound Med. 30:957–63. DOI: 10.7863/jum.2011.30.7.957. PMID: 21705728.
Article9. Tong TR, Chan OW, Lee KC. 2001; Diagnosing Kikuchi disease on fine needle aspiration biopsy: a retrospective study of 44 cases diagnosed by cytology and 8 by histopathology. Acta Cytol. 45:953–7. DOI: 10.1159/000328370. PMID: 11726124.10. Chou CH, Yang TL, Wang CP. 2014; Ultrasonographic features of tuberculous cervical lymphadenitis. J Med Ultrasound. 22:158–63. DOI: 10.1016/j.jmu.2014.06.007.
Article11. Knox J, Lane G, Wong JS, Trevan PG, Karunajeewa H. 2012; Diagnosis of tuberculous lymphadenitis using fine needle aspiration biopsy. Intern Med J. 42:1029–36. DOI: 10.1111/j.1445-5994.2012.02748.x. PMID: 22372860.
Article12. Ryu YJ, Cha W, Jeong WJ, Choi SI, Ahn SH. 2015; Diagnostic role of core needle biopsy in cervical lymphadenopathy. Head Neck. 37:229–33. DOI: 10.1002/hed.23580. PMID: 24375555.
Article13. Noguchi S, Noguchi A, Murakami N. 1970; Papillary carcinoma of the thyroid. I. Developing pattern of metastasis. Cancer. 26:1053–60. DOI: 10.1002/1097-0142(197011)26:5<1053::AID-CNCR2820260513>3.0.CO;2-X. PMID: 5476786.
Article14. Park JH, Lee YS, Kim BW, Chang HS, Park CS. 2012; Skip lateral neck node metastases in papillary thyroid carcinoma. World J Surg. 36:743–7. DOI: 10.1007/s00268-012-1476-5. PMID: 22354485.
Article15. Rosário PW, de Faria S, Bicalho L, Alves MF, Borges MA, Purisch S, et al. 2005; Ultrasonographic differentiation between metastatic and benign lymph nodes in patients with papillary thyroid carcinoma. J Ultrasound Med. 24:1385–9. DOI: 10.7863/jum.2005.24.10.1385. PMID: 16179622.
Article16. Leboulleux S, Girard E, Rose M, Travagli JP, Sabbah N, Caillou B, et al. 2007; Ultrasound criteria of malignancy for cervical lymph nodes in patients followed up for differentiated thyroid cancer. J Clin Endocrinol Metab. 92:3590–4. DOI: 10.1210/jc.2007-0444. PMID: 17609301.
Article17. Park JS, Son KR, Na DG, Kim E, Kim S. 2009; Performance of preoperative sonographic staging of papillary thyroid carcinoma based on the sixth edition of the AJCC/UICC TNM classification system. AJR Am J Roentgenol. 192:66–72. Erratum. DOI: 10.2214/AJR.07.3731. PMID: 19098181.
Article18. Sohn YM, Kwak JY, Kim EK, Moon HJ, Kim SJ, Kim MJ. 2010; Diagnostic approach for evaluation of lymph node metastasis from thyroid cancer using ultrasound and fine-needle aspiration biopsy. AJR Am J Roentgenol. 194:38–43. DOI: 10.2214/AJR.09.3128. PMID: 20028903.19. Yoo RE, Kim JH, Bae JM, Hwang I, Kang KM, Yun TJ, et al. 2020; Ultrasonographic indeterminate lymph nodes in preoperative thyroid cancer patients: malignancy risk and ultrasonographic findings predictive of malignancy. Korean J Radiol. 21:598–604. DOI: 10.3348/kjr.2019.0755. PMID: 32323505. PMCID: PMC7183832.20. Ha EJ, Chung SR, Na DG, Ahn HS, Chung J, Lee JY, et al. 2021; 2021 Korean Thyroid Imaging Reporting and Data System and imaging-based management of thyroid nodules: Korean Society of Thyroid Radiology consensus statement and recommendations. Korean J Radiol. 22:2094–123. DOI: 10.3348/kjr.2021.0713. PMID: 34719893. PMCID: PMC8628155.21. Kim MJ, Kim EK, Kim BM, Kwak JY, Lee EJ, Park CS, et al. 2009; Thyroglobulin measurement in fine-needle aspirate washouts: the criteria for neck node dissection for patients with thyroid cancer. Clin Endocrinol (Oxf). 70:145–51. DOI: 10.1111/j.1365-2265.2008.03297.x. PMID: 18466347.22. Giovanella L, Bongiovanni M, Trimboli P. 2013; Diagnostic value of thyroglobulin assay in cervical lymph node fine-needle aspirations for metastatic differentiated thyroid cancer. Curr Opin Oncol. 25:6–13. DOI: 10.1097/CCO.0b013e32835a9ab1. PMID: 23090642.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Hyperechoic Cervical Lymph Nodes after Injection of Silicone into the Face: A Case Report
- Ultrasound elastography for evaluation of cervical lymph nodes
- The evaluation of the cervical lymph node metastases using computed tomography in the head and neck cancer
- Cervical lymph node pathology on lymphatic enhanced CT scan
- A case report of castleman disease in th neck: CT and MRI finding