Brain Tumor Res Treat.
2024 Jan;12(1):40-49. 10.14791/btrt.2023.0046.
Suggestion of Follow-Up Period in Nonfunctioning Pituitary Incidentaloma Based on MRI Characteristics
- Affiliations
-
- 1Department of Neurosurgery, Dongguk University Ilsan Hospital, Goyang, Korea
- 2Department of Neurosurgery, Dongguk University College of Medicine, Seoul, Korea
- KMID: 2552337
- DOI: http://doi.org/10.14791/btrt.2023.0046
Abstract
- Background
For patients diagnosed with asymptomatic, non-functional pituitary incidentaloma (PI), periodic follow-up is generally proposed. However, the recommended follow-up period differs among existing guidelines and consensus is lacking. Thus, this study aimed to suggest follow-up periods for PI based on MRI characteristics.
Methods
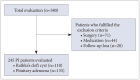
Between 2007 and 2023, 245 patients who were diagnosed with PI were retrospec- tively assessed. Their mean clinical and neuroradiological follow-up periods were 74.2 and 27.3 months, respectively. Their baseline clinical and neuroradiological characteristics were analyzed. These 245 patients were divided into two groups: those with PI size progression and those without PI size progression. Additionally, neuroradiological features of each group were analyzed according to presumptive diagnoses of PI.
Results
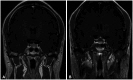
PI size increased in 33 of 245 patients. For the remaining 212 patients, PI size de- creased or stayed unchanged. Of the 33 patients with PI size progression, ten underwent surgery. Stalk deviation (p<0.001) and lesion enhancement (p=0.001) were significantly more observed in those with PI size progression than in those without PI size progression. MRI morphological factors were not related to changes in PI size in the presumptive Rathke’s cleft cyst group. In the presumptive pituitary adenoma group, absence of tumor enhancement (p<0.001) and stalk deviation (p<0.001) were significantly associated with tumor reduction and progression, respectively.
Conclusion
Our findings support an additional guideline for patients with asymptomatic non-func- tional PI without stalk deviation and enhancement. For these patients, the clinical and neuroradiological follow-up periods could be reduced.
Keyword
Figure
Reference
-
1. Tahara S, Hattori Y, Suzuki K, Ishisaka E, Teramoto S, Morita A. An overview of pituitary incidentalomas: diagnosis, clinical features, and management. Cancers (Basel). 2022; 14:4324. PMID: 36077858.
Article2. Giraldi E, Allen JW, Ioachimescu AG. Pituitary incidentalomas: best practices and looking ahead. Endocr Pract. 2023; 29:60–68. PMID: 36270609.
Article3. Constantinescu SM, Maiter D. Pituitary incidentaloma. Presse Med. 2021; 50:104081. PMID: 34687911.
Article4. Freda PU, Beckers AM, Katznelson L, Molitch ME, Montori VM, Post KD, et al. Pituitary incidentaloma: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2011; 96:894–904. PMID: 21474686.
Article5. Galland F, Vantyghem MC, Cazabat L, Boulin A, Cotton F, Bonneville JF, et al. Management of nonfunctioning pituitary incidentaloma. Ann Endocrinol (Paris). 2015; 76:191–200. PMID: 26054868.
Article6. Park M, Lee SK, Choi J, Kim SH, Kim SH, Shin NY, et al. Differentiation between cystic pituitary adenomas and Rathke cleft cysts: a diagnostic model using MRI. AJNR Am J Neuroradiol. 2015; 36:1866–1873. PMID: 26251436.7. Jhaveri MD. Diagnostic imaging: brain. 4th ed. Philadelphia, PA: Elsevier;2020.8. Bonneville JF, Bonneville F, Cattin F. Magnetic resonance imaging of pituitary adenomas. Eur Radiol. 2005; 15:543–548. PMID: 15627195.
Article9. Shih RY, Schroeder JW, Koeller KK. Primary tumors of the pituitary gland: radiologic-pathologic correlation. Radiographics. 2021; 41:2029–2046. PMID: 34597177.
Article10. Crenshaw WB, Chew FS. Rathke’s cleft cyst. AJR Am J Roentgenol. 1992; 158:1312. PMID: 1590132.11. Pisaneschi M, Kapoor G. Imaging the sella and parasellar region. Neuroimaging Clin N Am. 2005; 15:203–219. PMID: 15927868.
Article12. Jin YH. A new LogMAR vision chart: Jin’s vision chart. J Korean Ophthalmol Soc. 1997; 38:2036–2044.13. Winn HR. Youmans and Winn neurological surgery. 7th ed. Philadelphia, PA: Elsevier;2017.14. Chong GYC, Tan KCB, Lau EYF, Lai AYT, Man KKY, Chan TM, et al. A study on clinical outcomes of Rathke’s cleft cyst in patients managed conservatively. Pituitary. 2022; 25:258–266. PMID: 34807360.
Article15. Tosaka M, Sato N, Hirato J, Fujimaki H, Yamaguchi R, Kohga H, et al. Assessment of hemorrhage in pituitary macroadenoma by T2*-weighted gradient-echo MR imaging. AJNR Am J Neuroradiol. 2007; 28:2023–2029. PMID: 17898201.
Article16. Wen L, Hu LB, Feng XY, Desai G, Zou LG, Wang WX, et al. Rathke’s cleft cyst: clinicopathological and MRI findings in 22 patients. Clin Radiol. 2010; 65:47–55. PMID: 20103421.
Article17. Kim CW, Hwang K, Joo JD, Kim YH, Han JH, Kim CY. Spontaneous involution of Rathke’s cleft cysts without visual symptoms. Brain Tumor Res Treat. 2016; 4:58–62. PMID: 27867913.
Article18. Truong LUF, Marlier B, Decoudier B, Litre CF, Barraud S. Vanishing Rathke’s cleft cyst. Ann Endocrinol (Paris). 2022; 83:260–262. PMID: 35504336.
Article19. Kinoshita Y, Taguchi A, Yamasaki F, Tominaga A, Arita K, Horie N. Natural course of Rathke’s cleft cysts and risk factors for progression. J Neurosurg. 2022; 138:1426–1432. PMID: 36057119.
Article20. Fernandez-Balsells MM, Murad MH, Barwise A, Gallegos-Orozco JF, Paul A, Lane MA, et al. Natural history of nonfunctioning pituitary adenomas and incidentalomas: a systematic review and metaanalysis. J Clin Endocrinol Metab. 2011; 96:905–912. PMID: 21474687.
Article21. Thapa S, Bhusal K. Hyperprolactinemia. In: StatPearls [Internet]. Treasure Island, FL: StatPearls Publishing;2024. Accessed October 21, 2023. at. https://www.ncbi.nlm.nih.gov/books/NBK537331/.22. Dehelean L, Romosan AM, Papava I, Bredicean CA, Dumitrascu V, Ursoniu S, et al. Prolactin response to antipsychotics: an inpatient study. PLoS One. 2020; 15:e0228648. PMID: 32017792.
Article23. Vilar L, Abucham J, Albuquerque JL, Araujo LA, Azevedo MF, Boguszewski CL, et al. Controversial issues in the management of hyperprolactinemia and prolactinomas - An overview by the Neuroendocrinology Department of the Brazilian Society of Endocrinology and Metabolism. Arch Endocrinol Metab. 2018; 62:236–263. PMID: 29768629.
Article24. Imran SA, Yip CE, Papneja N, Aldahmani K, Mohammad S, Imran F, et al. Analysis and natural history of pituitary incidentalomas. Eur J Endocrinol. 2016; 175:1–9. PMID: 27037179.
Article25. Tresoldi AS, Carosi G, Betella N, Del Sindaco G, Indirli R, Ferrante E, et al. Clinically nonfunctioning pituitary incidentalomas: characteristics and natural history. Neuroendocrinology. 2020; 110:595–603. PMID: 31525736.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Characteristics and Natural Course of Pituitary Incidentaloma in Korea
- A Case of Adrenal Incidentaloma with a Pituitary Incidentaloma
- Developed diplopia and ptosis due to a nonfunctioning pituitary macroadenoma during pregnancy
- The Characteristics and Follow-up of Pituitary Incidentaloma
- A case of pituitary resistance to thyroid hormone with nonfunctioning pituitary microadenoma