Korean J Gastroenterol.
2024 Jan;83(1):23-27. 10.4166/kjg.2023.112.
A Case of Type II Achalasia Occurring in a Nonagenarian Diagnosed with Acute Food Impaction
- Affiliations
-
- 1Department of Internal Medicine, Kosin University College of Medicine, Busan, Korea
- KMID: 2552239
- DOI: http://doi.org/10.4166/kjg.2023.112
Abstract
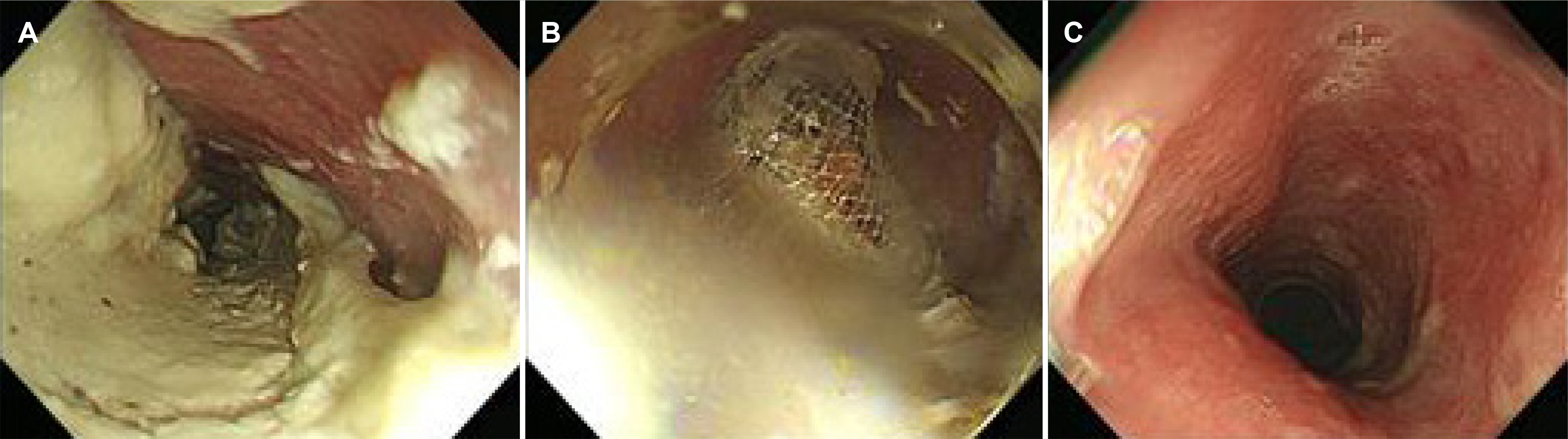
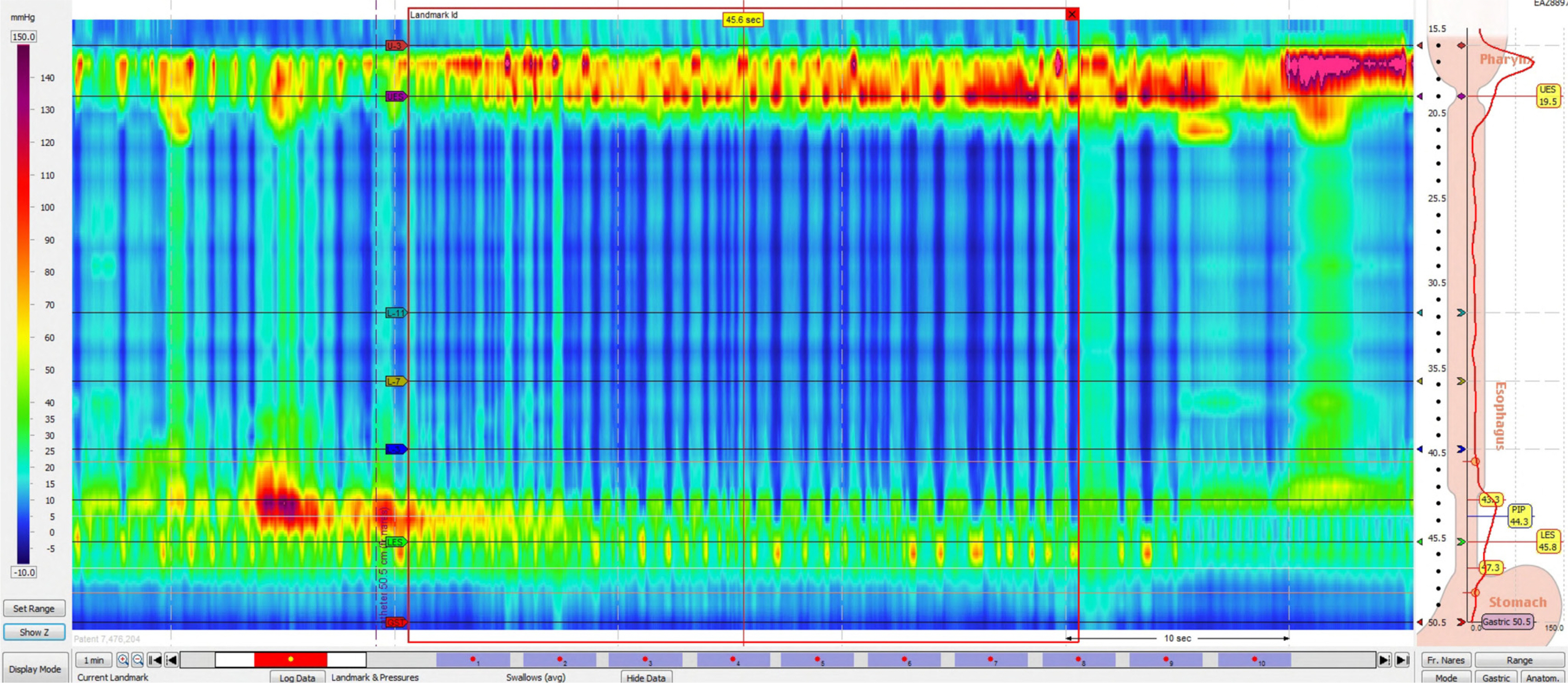
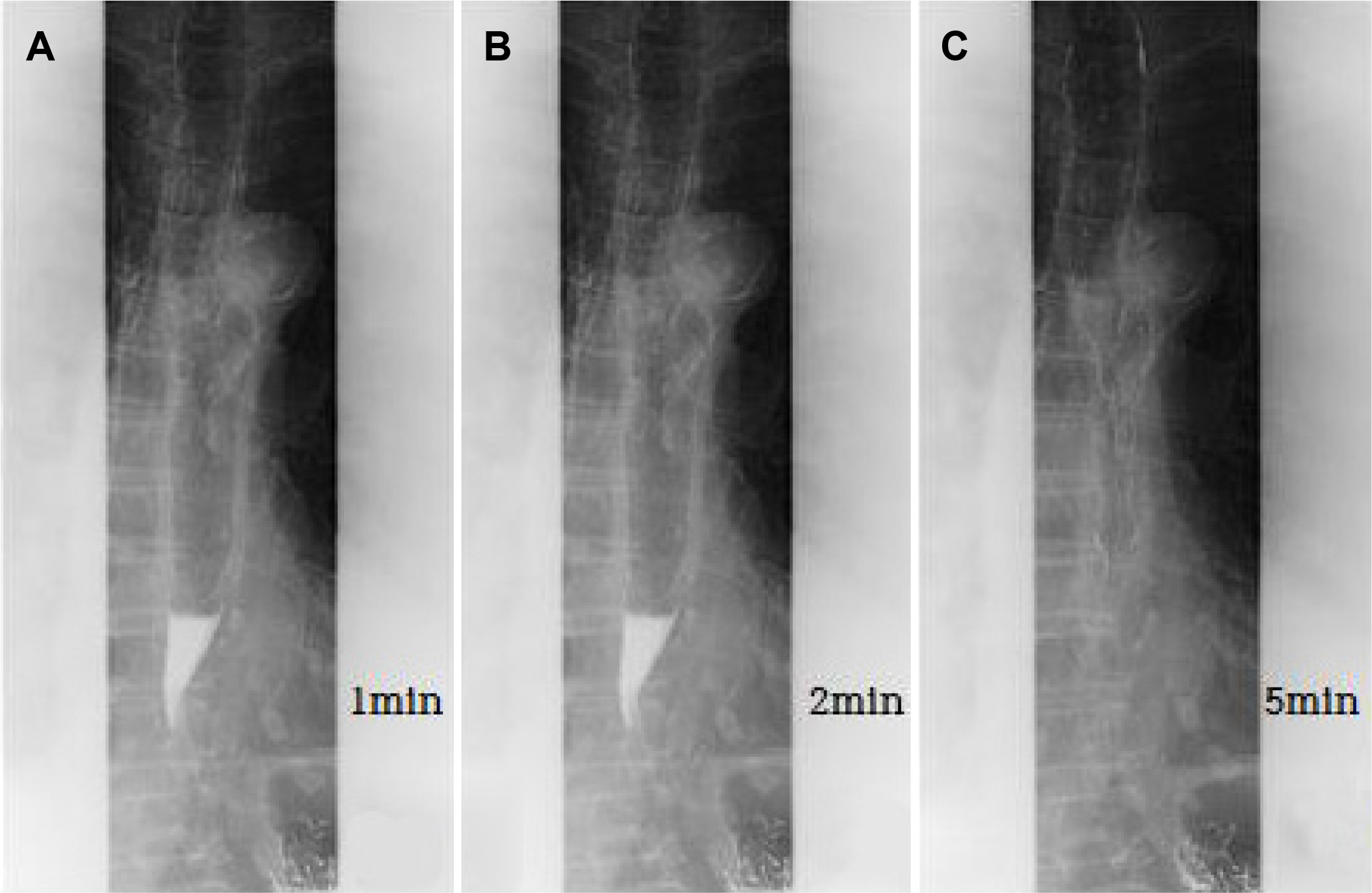
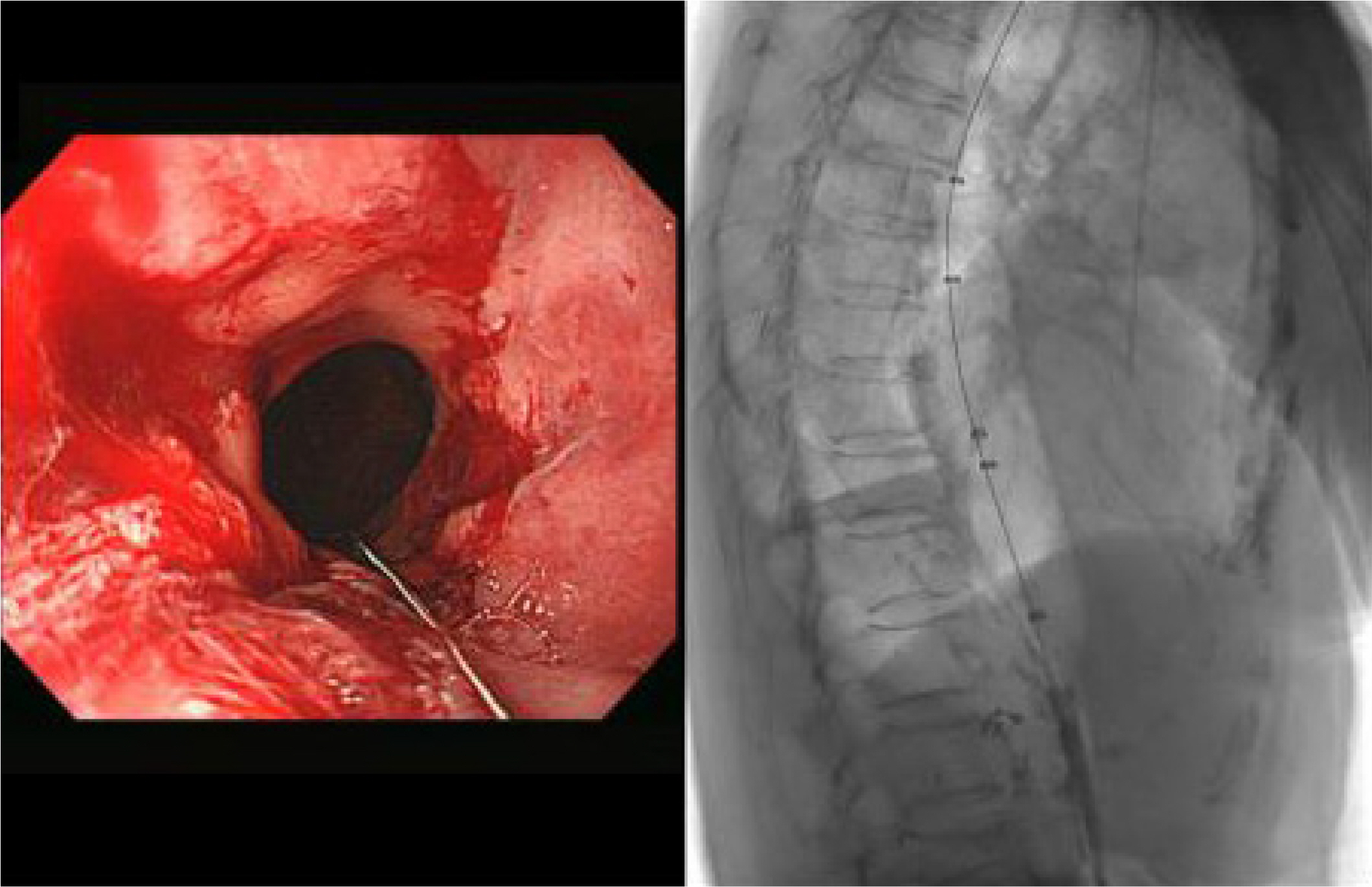
- Achalasia is an esophageal motility disorder characterized by loss of esophageal peristalsis and impaired relaxation of the lower esophageal sphincter. Patients with achalasia often complain of persistent symptoms for several years before diagnosis. On the other hand, achalasia diagnosed as a sudden esophageal food impaction is uncommon, and no report has been issued on the diagnosis and successful treatment of achalasia in a 95-year-old patient. We report a case of achalasia diagnosed by high-resolution esophageal manometry and timed barium esophagography after food material removal by endoscopy in a 95-year-old woman who visited the hospital due to sudden esophageal food impaction and was successfully treated by endoscopic balloon dilatation.
Figure
Reference
-
1. Kim E, Lee H, Jung HK, Lee KJ. 2014; Achalasia in Korea: an epidemiologic study using a national healthcare database. J Korean Med Sci. 29:576–580. DOI: 10.3346/jkms.2014.29.4.576. PMID: 24753707. PMCID: PMC3991803.2. Park MI. 2014; Pathogenesis of achalasia. Korean J Helicobacter Up Gastrointest Res. 14:71–78. DOI: 10.7704/kjhugr.2014.14.2.71.3. Mari A, Sbeit W, Abboud W, Awadie H, Khoury T. 2021; Achalasia in the elderly: Diagnostic approach and a proposed treatment algorithm based on a comprehensive literature review. J Clin Med. 10:5565. DOI: 10.3390/jcm10235565. PMID: 34884267. PMCID: PMC8658648.4. Eckardt VF. 2001; Clinical presentations and complications of achalasia. Gastrointest Endosc Clin N Am. 11:281–292. DOI: 10.1016/S1052-5157(18)30071-0. PMID: 11319062.5. Jeon HH, Kim JH, Youn YH, Park H, Conklin JL. 2017; Clinical characteristics of patients with untreated achalasia. J Neurogastroenterol Motil. 23:378–384. DOI: 10.5056/jnm16177. PMID: 28351117. PMCID: PMC5503287.6. Eckardt VF, Köhne U, Junginger T, Westermeier T. 1997; Risk factors for diagnostic delay in achalasia. Dig Dis Sci. 42:580–585. DOI: 10.1023/A:1018855327960. PMID: 9073142.7. Schechter RB, Lemme EM, Novais P, Biccas B. 2011; Achalasia in the elderly patient: a comparative study. Arq Gastroenterol. 48:19–23. DOI: 10.1590/S0004-28032011000100005. PMID: 21537537.8. Kim KH, Choi SC, Seo GS, Kim YS, Choi CS, Im CJ. 2010; Esophageal bezoar in a patient with achalasia: case report and literature review. Gut Liver. 4:106–109. DOI: 10.5009/gnl.2010.4.1.106. PMID: 20479921. PMCID: PMC2871618.9. Sidhu GK, Sern GK, Khine HH. 2023; An Uncommon case of weight loss in a nonagenarian. Ann Geriatr Med Res. 27:172–174. DOI: 10.4235/agmr.23.0015. PMID: 37072905. PMCID: PMC10326406.10. Jung HK, Hong SJ, Lee OY, et al. 2020; 2019 Seoul consensus on esophageal achalasia guidelines. J Neurogastroenterol Motil. 26:180–203. DOI: 10.5056/jnm20014. PMID: 32235027. PMCID: PMC7176504.11. Yaqub S, Shafique M, Kjæstad E, et al. 2012; A safe treatment option for esophageal bezoars. Int J Surg Case Rep. 3:366–367. DOI: 10.1016/j.ijscr.2012.04.008. PMID: 22609703. PMCID: PMC3376689.12. Kang WR, Park SY, You HS, et al. 2023; A Single-center 12-year experience of patients with gastrointestinal bezoars. Korean J Gastroenterol. 81:253–258. DOI: 10.4166/kjg.2023.024. PMID: 37350520.13. Enestvedt BK, Williams JL, Sonnenberg A. 2011; Epidemiology and practice patterns of achalasia in a large multi-centre database. Aliment Pharmacol Ther. 33:1209–1214. DOI: 10.1111/j.1365-2036.2011.04655.x. PMID: 21480936. PMCID: PMC3857989.14. Ramchandani M, Nageshwar Reddy D, Nabi Z, et al. 2018; Management of achalasia cardia: Expert consensus statements. J Gastroenterol Hepatol. 33:1436–1444. DOI: 10.1111/jgh.14097. PMID: 29377271.15. Song JY, Park MI, Moon W, et al. 2008; A case of achalasia diagnosed before the detection of colon cancer with multiple metastasis. Kor J Neurogastroenterol Motil. 14:51–56.16. Choe AR, Jung HK. 2019; Management of achalasia: expert consensus statements. Korean J Gastroenterol. 73:294–298. DOI: 10.4166/kjg.2019.73.5.294.17. Tenlik İ, Öztürk Ö, Özin Y, et al. 2023; Pneumatic dilation in geriatric achalasia patients. Turk J Gastroenterol. 34:332–338. DOI: 10.5152/tjg.2023.22178. PMID: 36789986. PMCID: PMC10210637.18. Han SR, Park MI, Moon W, et al. 2006; A case of achalasia treated by two sessions of balloon dilatation: the long term follow-up. Kor J Neurogastroenterol Motil. 12:177–180.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Achalasia Cardia Subtyping by High-Resolution Manometry Predicts the Therapeutic Outcome of Pneumatic Balloon Dilatation
- Progression of Jackhammer Esophagus to Type II Achalasia
- A Clinical Study On The Occurrence Of Food Impaction
- Esophagography in Patients With Esophageal Achalasia Diagnosed With High-resolution Esophageal Manometry
- An Uncommon Case of Weight Loss in a Nonagenarian